■ Several anatomic anomalies are relevant to the surgeon, as they predispose patients to the development of TOS.
■ The most common is a cervical rib, and a preoperative chest radiograph is adequate for its detection. When present, cervical ribs appear as extensions of the transverse process of C7. Cervical ribs may be complete or partial, with the anterior end attaching to the 1st rib or floating freely. Additionally, the anterior end may be fibrous and not calcified and thus not completely visualized on chest radiograph. By rigidly confining the thoracic outlet, cervical ribs render the neurovascular structures more prone to compression. Although present in the general population with an incidence of 0.5% to 1%, they are found in 5% to 10% of all TOS patients.
■ A prominent C7 transverse process or bifid 1st rib is also associated with TOS.
Positioning
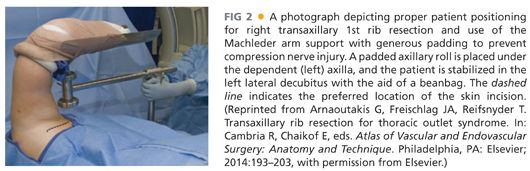
■ General endotracheal anesthesia is induced and sequential compression devices are applied.
■ The patient is then moved to the lateral decubitus position using a beanbag to facilitate positioning.
■ Care should be taken to pad the dependent axilla and support the head. The sterile field incorporates the arm, axilla, and shoulder.
■ An adjustable Machleder arm support is affixed to the operating table with the vertical support bar attached to the operating table at the level of the patient’s chin.
■ Generous padding around the patient’s arm prior to placement in the arm holder protects the median and ulnar nerves from compression as they cross the elbow joint (FIG 2).
TECHNIQUES
INCISION
■ Prophylactic antibiotics are administered. A first-generation cephalosporin is preferred. In patients with penicillin allergy, clindamycin or vancomycin is used.
■ After securing the arm in the retractor, the surgeon identifies the anterior border of the latissimus dorsi muscle and the posterior surface of the pectoralis major muscle.
■ A transverse skin line incision should be made in the inferior axillary hairline extending between these two muscle borders.
EXPOSURE
■ Electrocautery is used to divide the subcutaneous tissue until thin areolar tissue superficial to the chest wall is encountered. A self-retaining Cerebellar or Weitlaner retractor is then inserted into the wound. Upon encountering the chest wall—and if in the correct anatomic plane—gentle blunt dissection with the surgeon’s fingers or a pair of Kittner or peanut dissectors easily separates the soft tissues from the chest wall. This dissection is in a cephalad direction and the 2nd rib will rapidly come into view.
■ The intercostobrachial nerve is located in the 2nd intercostal space. Although frequently difficult to avoid, care should be taken not to impart excess traction as injury results in numbness or dysesthesia of the medial aspect of the proximal arm.
■ Raising the Machleder arm support at this point allows for optimal access to the 1st rib and thoracic outlet. The aid of fiberoptic-lighted Deaver retractors facilitates visualization during this portion of the dissection. Alternatively, the surgeon should wear a headlight.
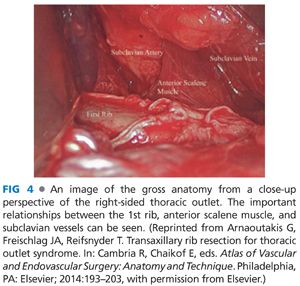
■ The 1st rib is identified near its insertion at the sternoclavicular joint and generally encountered higher than anticipated. A Kittner or peanut dissector is then used to gently sweep away the loose fibrous tissue overlying the 1st rib partially exposing the brachial plexus, subclavian artery and vein, and scalene muscles. There is occasionally a small branch of the subclavian artery that must be ligated and divided in order to fully expose the operative field.
■ The next step is to fully expose the rib. Depending on the patient’s anatomy, it generally is easiest to first clear off the intercostal muscles laterally. A Cobb periosteal elevator works best, but any type of long elevator may be used (FIG 3). The dissection proceeds in the anterior and posterior directions until all the intercostal muscle attachments are divided from the rib. The elevator can then be used to elevate the 1st rib, thus separating the rib from the underlying parietal pleura. This mobilization should continue from behind the brachial plexus in the posterior direction to beyond the subclavian vein in the anterior direction.
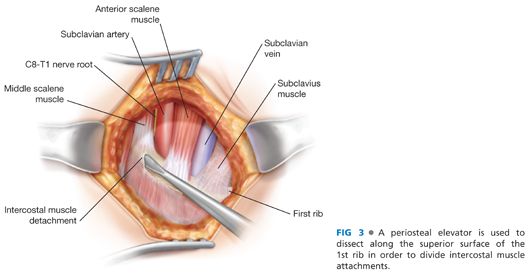
■ Attention is then directed to the superior border of the 1st rib, where the periosteal elevator is used to bluntly detach the scalene medius fibers from the rib. The long thoracic nerve courses along the lateral edge of the scalene medius muscle but is generally not visualized. Avoiding sharp dissection and closely adhering to the surface of the rib during blunt dissection prevents injury to the long thoracic nerve.
■ The anterior scalene muscle should now be clearly identified as it arises from the medial superior aspect of the 1st rib (FIG 4). A right-angled clamp is passed behind the anterior scalene muscle near its insertion on the scalene tubercle. Gently lifting the anterior scalene with the right-angled clamp protects the subclavian artery as it courses posterior to the muscle (FIG 5). It is important to free several centimeters of the muscle prior to dividing it with Metzenbaum scissors (FIG 6). This maneuver facilitates resection of a portion of the anterior scalene muscle, which has been shown to reduce recurrence rates when compared with division at its insertion point on the rib.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


