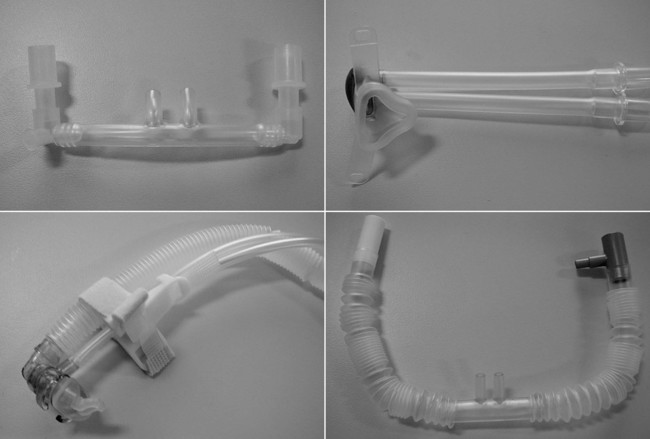
1. Identify indications for continuous positive airway pressure. 2. Initiate and assess neonatal and pediatric noninvasive positive pressure ventilation. 3. Identify indications for invasive mechanical ventilation. 4. Describe the complications associated with intubation. 5. Initiate and assess neonatal and pediatric invasive mechanical ventilation. 6. Initiate and assess high-frequency positive pressure ventilation, both high-frequency jet ventilation and high-frequency oscillatory ventilation. The use of mechanical ventilation is one of the most significant advances in the history of medicine, enabling therapies, procedures, and interventions in an incredibly wide array of otherwise unrelated subspecialties. Nearly all of the critical care and surgical interventions we currently provide would be impossible or prohibitively difficult without the use of mechanical ventilation. Many thousands, even millions, of lives have likely been saved because of this technology. However, the use of mechanical ventilation also brings with it a host of associated problems and complications. Referencing the delicate nature of the appropriate use of mechanical ventilation, and obviously indulging in a bit of hyperbole, a respected mentor of the author of this chapter once referred to the mechanical ventilator as “the single deadliest instrument ever placed in the hands of physicians” (and respiratory therapists [RTs]). As such, the appropriate selection of patients for, management of, and ultimate timely liberation from mechanical ventilation can dramatically affect patient outcomes. Noninvasive positive pressure ventilation is a life-saving intervention in neonatal and pediatric care. The ability to noninvasively provide respiratory support, improve upper and lower airway patency, and improve lung recruitment has proven invaluable. Noninvasive support can be utilized simply as CPAP or as bilevel positive airway pressure (BiPAP), with additional inspiratory pressure added to spontaneous or controlled breaths. Widespread use of nasal CPAP has reduced intubation times, intubation rates, pulmonary morbidity, and bronchopulmonary dysplasia rates dramatically in neonates. Pediatric applications of both CPAP and BiPAP, including those in acute lung injury, asthma, and postoperative conditions, have also resulted in significant improvements in care. Indications for CPAP in children are listed in Box 26-1. Noninvasive positive pressure ventilation is positive pressure applied to the upper oropharynx through a noninvasive interface, providing improved pulmonary mechanics and modest lung recruitment. Interfaces are varied but include nasal prongs, nasal masks, nasal–oral masks, full-face masks, and helmets. Images of these interfaces are given in Figure 26-1. The effort required to adequately set up a CPAP interface is well worth it, as avoiding intubation and its attendant complications is a worthy goal. A respiratory therapist skilled in the application of noninvasive ventilator interventions is invaluable in a pediatric or neonatal unit. The following is the step-by-step process for initiating neonatal and pediatric noninvasive positive pressure ventilation. 1. Review the patient’s chart. 2. Verify the physician’s order or the facility’s protocol for standard of care. 3. Obtain, clean, inspect, and test the appropriate equipment prior to entering the patient’s room. 4. Follow personal protective equipment (PPE) requirements, and observe standard precautions for any transmission-based isolation procedure. 5. Identify the patient using two patient identifiers. 6. Introduce yourself to the patient and to the family. 7. Explain the procedure to the patient and to the family, and acknowledge the patient’s understanding. 8. Perform proper hand hygiene, and put on gloves, mask, and protective eyewear, as appropriate for the procedure. 1. Place the patient in a comfortable position. 3. Assess the upper airway for abnormalities. 4. Obtain the interface and the securing devices. 5. Establish and implement the appropriate settings or execute the physician’s orders: b. Inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP) levels (if ordered) 6. Apply and secure the device to the patient. 7. Ensure suitable fit and minimal leak. 10. Set the alarms appropriately. 11. Set up the noninvasive monitors. 12. Remove the supplies from the patient’s room, and clean the area, as needed. 13. Remove PPE, and perform proper hand hygiene prior to leaving the patient’s room. 1. Review the patient’s chart for the patient’s current vital signs and NIV settings. 2. Review the patient’s most recent arterial blood gas (ABG) or SpO2 values. 3. Review the most recent chest radiograph. 4. Identify the current sedation medications. 5. Verify the physician’s order or the facility’s protocol for standard of care. 6. Obtain, clean, and inspect the appropriate equipment prior to entering the patient’s room. 7. Follow PPE requirements, and observe standard precautions for any transmission-based isolation procedure. 8. Identify the patient using two patient identifiers. 9. Introduce yourself to the patient and to the family. 10. Explain the procedure to the patient and to the family, and acknowledge the patient’s understanding. 11. Perform proper hand hygiene, and put on gloves, mask, and protective eyewear, as appropriate for the procedure. 1. Approach the patient before you approach the CPAP generator. a. Overall appearance and comfort b. Nasal prong or mask position c. Skin integrity at all contact points d. Breath sounds; suction, if indicated 3. Assess the NIV generator function and settings: a. Security of circuit connections b. Heat and humidification device and airway temperature d. Adequacy of delivery of tidal volume e. Pressure level(s), depending on mode: 4. Ensure that the manual ventilation device and the suction equipment are available at the patient’s bedside. 5. Remove the supplies from the patient’s room, and clean the area, as needed. 6. Remove PPE, and perform proper hand hygiene prior to leaving the patient’s room. The initiation of neonatal or pediatric mechanical ventilation begins with the decision to intubate or not intubate a patient. Clinical indications for mechanical ventilation and initial ventilator settings are given in Boxes 26-2 and 26-3. This decision is difficult and has many implications, as intubating too early or too late may both result in increased patient morbidity. Complications and hazards of endotracheal intubation in infants and children are listed in Box 26-4. In general, it is a well-tolerated and safe procedure when done with care and attention to detail. The RT plays a key role in the proper initiation of pediatric mechanical ventilation, and the establishment of age-appropriate and disease-appropriate therapeutic goals at the outset of therapy.
Neonatal and Pediatric Noninvasive and Invasive Ventilation
Procedural Assessments
Equipment
» Skill Check Lists
26-1 Initiation of Neonatal and Pediatric Noninvasive Positive Pressure Ventilation
Procedural Preparation
Implementation
26-2 Assessing the Neonatal and Pediatric Noninvasive Positive Pressure Ventilation System
Procedural Preparation
Implementation
26-3 Initiating Neonatal and Pediatric Mechanical Ventilation























