Wolff-Parkinson-White (WPW) syndrome carries a risk for symptomatic arrhythmias and sudden death. The aim of this study was to examine the natural history of patients with Wolff-Parkinson-White syndrome diagnosed in childhood followed longitudinally at a single institution. The study population consisted of 446 patients. The median age of diagnosis was 7 years, and 61% were male. Associated heart disease was present in 40 patients (9%). Modes of presentation included supraventricular tachycardia (38%), palpitations (22%), chest pain (5%), syncope (4%), atrial fibrillation (0.4%), sudden death (0.2%), and incidental findings (26%); data were unavailable in 4%. During the study period, a total of 243 patients (54%) had supraventricular tachycardia, and 7 patients (1.6%) had atrial fibrillation. Of patients who presented at ≤3 months of age, 35% had resolution of manifest preexcitation compared with 5.8% who presented at >3 months of age (p <0.0001). There were 6 sudden deaths (1.3%), with an incidence of 2.8 per 1,000 patient-years. Two of these patients had structurally normal hearts (incidence 1.1 per 1,000 patient-years). Four of these patients had associated heart disease (incidence 27 per 1,000 patient-years) (p <0.01). In conclusion, in a large population of patients with Wolff-Parkinson-White syndrome diagnosed in childhood, 64% had symptoms at presentation, and an additional 20% developed symptoms during follow-up. There were 6 sudden deaths (1.3%), with an overall incidence of 1.1 per 1,000 patient-years in patients with structurally normal hearts and 27 per 1,000 patient-years in patients with associated heart disease.
Wolff-Parkinson-White (WPW) syndrome is a condition characterized by a short PR interval associated with ventricular preexcitation manifested by a delta wave, first described in 1930. The clinical spectrum ranges from no cardiac symptoms to recurrent paroxysmal supraventricular tachycardia (SVT) to, in some cases, sudden cardiac collapse or death. Earlier natural history studies have included varying patient populations, with ages ranging from children to adults, and most have shown a low but finite incidence of sudden death. Concern about the actual risk for sudden death has a tremendous impact on the clinical management of these patients, particularly those who are incidentally found to have preexcitation on an electrocardiogram without associated cardiac symptoms. The purpose of the present study was to examine the natural histories of patients with WPW syndrome diagnosed in childhood followed longitudinally at a single institution.
Methods
This study was a retrospective review. Patients with diagnoses of WPW syndrome who were seen from 1960 to 2010 were identified from the Children’s Hospital of Pittsburgh cardiology database. During this time frame, Children’s Hospital of Pittsburgh Pediatric Cardiology represented the major cardiology presence in this region, seeing community-based referrals as well as tertiary care referrals. Patient data were obtained from hospital medical records. All patients aged <21 years with available records were included. All electrocardiograms were reviewed by 1 investigator to reconfirm the diagnosis of WPW syndrome. Data collected included patient demographics, hemodynamically significant associated heart disease, clinical presentation, documented arrhythmias, presence of persistent or intermittent preexcitation, spontaneous resolution of manifest preexcitation, and clinical events during follow-up. Patients with bicuspid aortic valves were not considered to have hemodynamically significant lesions unless they had more than mild aortic stenosis or insufficiency or concomitant lesions. The duration of follow-up was defined as time of presentation to last clinical follow-up, time of ablation, or time of death. Ablation was considered to have changed the patient’s natural history and thus was considered a primary end point.
Statistical analysis of continuous data was performed using Student’s t tests. Categorical data were evaluated using chi-square analysis. The incidence of sudden death was calculated from the number of cases observed relative to the total patient-years of observation as derived from the database.
Results
Six hundred patients were identified from the cardiology database search. Medical record patient data were available for 446 patients (75%), who constituted the study population. Some medical records spanning the data collection period were eliminated on the basis of hospital chart storage policy and were not available for review.
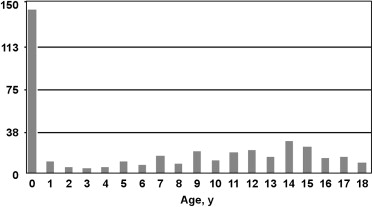
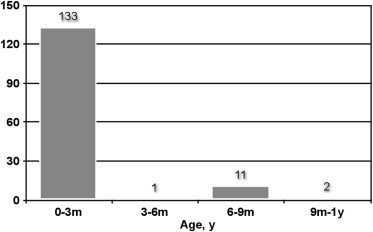
There were 274 male (61%) and 172 female (39%) patients. The median age of diagnosis was 7 years (range 0 to 20). The most common age of presentation was ≤3 months, with 133 patients (30%). The remainder of the patients were diagnosed between 4 months and 20 years of age ( Figures 1 and 2 ). The median duration of follow-up was 3 years (range 0 to 23). There was a total of 2,160 patient-years of follow-up. A total of 90 patients had >10 years of follow-up, 71 patients had 5 to 10 years, 164 patients had 1 to 4 years, and 121 patients had <1 year of follow-up. The group of patients with <1 year of follow-up fell primarily into 2 time frames. Many patients who were diagnosed in the 1970s and 1980s and were asymptomatic at diagnosis were given the diagnosis of “incidental WPW syndrome” and discharged from follow-up. Concurrently, many patients with recent diagnoses in the 2000s underwent electrophysiologic studies with ablation <1 year after diagnosis.
Forty patients (9%) had hemodynamically significant associated heart disease ( Table 1 ). The most commonly diagnosed heart diseases were ventricular septal defect, Ebstein’s anomaly, and congenitally corrected transposition of the great arteries. In the database, there were 7,055 patients with ventricular septal defects, compared with 126 patients with Ebstein’s anomaly and 106 patients with congenitally corrected transposition of the great arteries.
| Lesion | n (%) |
|---|---|
| Ventricular septal defect | 10 (25%) |
| Ebstein’s anomaly | 8 (20%) |
| Congenitally corrected transposition of the great arteries | 6 (15%) |
| Coarctation of the aorta | 3 (7.5%) |
| Complete atrioventricular septal defect | 3 (7.5%) |
| Dilated cardiomyopathy | 2 (5%) |
| Hypertrophic cardiomyopathy | 2 (5%) |
| Rhabdomyoma | 2 (5%) |
| Anomalous left coronary from pulmonary | 1 (2.5%) |
| Heterotaxy | 1 (2.5%) |
| Patent ductus arteriosus | 1 (2.5%) |
| Cor triatriatum | 1 (2.5%) |
Findings at presentation included documented SVT in 167 (37%), palpitations in 97 (22%), chest pain in 22 (5%), syncope in 18 (4%), congenital heart disease in 17 (3%), atrial fibrillation in 2 (0.4%), sudden death in 1 (0.2%), unknown presentation in 7 (1.5%), and incidental finding in 116 (26%) ( Figure 3 ). Of the 116 patients with incidental findings of WPW syndrome, 53 (46%) were being evaluated for murmurs; 49 (42%) underwent electrocardiography for noncardiac surgery, health fair screening, primary care physician screening, or attention deficit/hyperactivity disorder medication clearance; 8 (7%) had seizure disorders; 3 (3%) had respiratory distress; 2 (2%) had dizziness; and 1 had gastroesophageal reflux as a cause of “spells” (1%). See Figure 4 for age distribution and symptoms at diagnosis.
During the study period, a total of 243 patients (54%) had SVT, 167 (37%) at presentation and an additional 76 (17%) during follow-up. Seven patients (1.6%) had atrial fibrillation, 2 at presentation and 5 during follow-up. Thirty patients (6.7%) had ≥1 episode of syncope, 18 at presentation and 12 during follow-up. All episodes of syncope were believed to be vasovagal on the basis of the events surrounding the syncope, preceding symptoms, and clinician evaluation. Of these patients who had syncope, 12 received no further evaluation, 11 received Holter monitors, and 12 underwent exercise stress testing. Six of these patients were unable to be noninvasively risk stratified on either stress testing or Holter monitor and went on to undergo electrophysiology and ablation.
The mean age of atrial fibrillation in all patients was 14.7 years (range 11 to 18).
Of the 116 asymptomatic patients at presentation, 13 (11%) subsequently had documented SVT and 8 (7%) developed palpitations. Three (2.6%) of these asymptomatic patients had vasovagal syncope and underwent further testing, and none had atrial fibrillation.
Spontaneous resolution of manifest WPW syndrome, defined as disappearance of the delta wave on electrocardiography, occurred in 14.6% of the entire study group. A total of 133 patients (30%) presented at ≤3 months of age. Of these, 47 (35%) had spontaneous resolution of their WPW syndrome. Of the patients presenting at >3 months of age, 18 (5.7%) had spontaneous resolution, the oldest at 20 years of age. This difference was statistically significant (p <0.0001; Figure 5 ). Of the 116 asymptomatic patients, 14 (12%) had spontaneous resolution of their WPW syndrome.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


