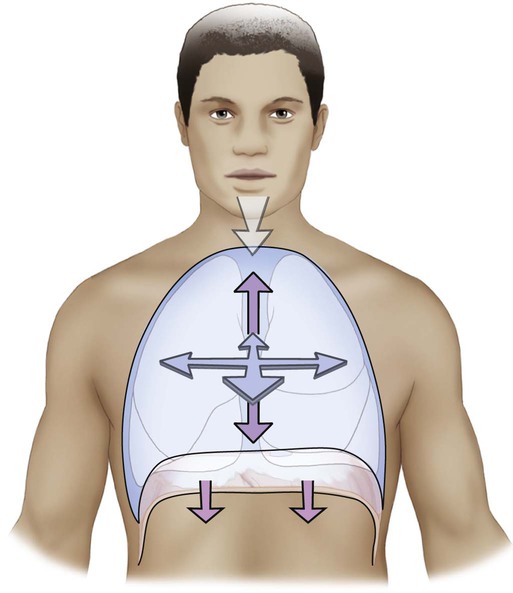
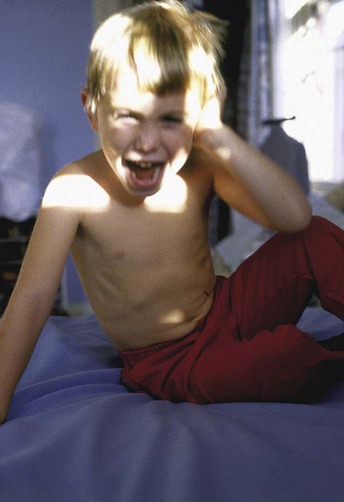
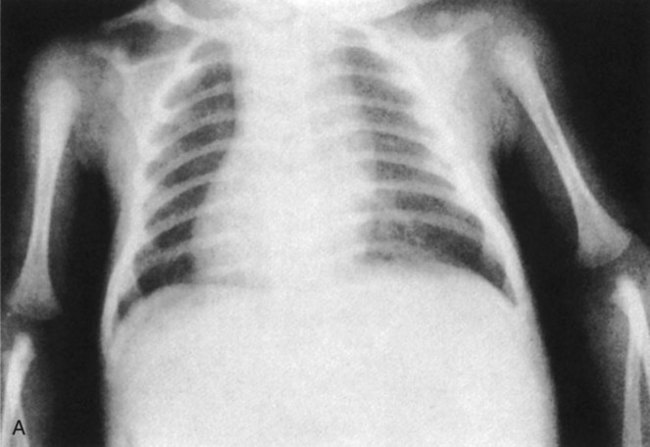
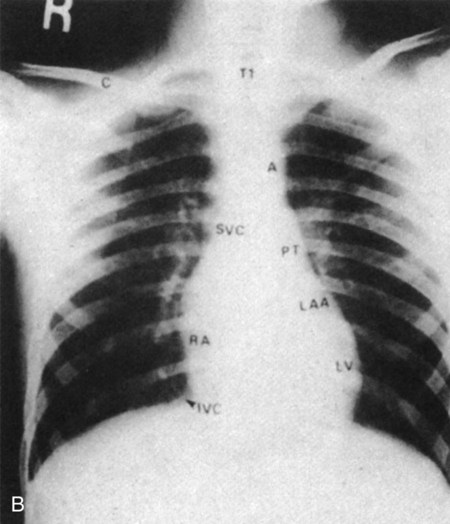
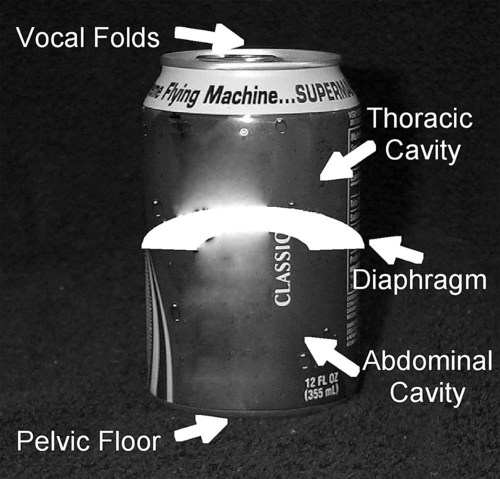
The cardiovascular and pulmonary systems provide both physiological support (oxygen delivery) (see Chapters 2 and 4) as well as a mechanical support (respiratory and trunk muscle control) for movement. This chapter focuses on breathing mechanics and their interactions with other organ systems in both health and dysfunction. Its three main premises are: 1. Breathing is a three-dimensional motor task that is influenced by gravity in the three planes of motion. 2. Breathing is influenced by multisystem interactions that simultaneously support respiratory and postural control during motor tasks. 3. The mechanics of breathing influence both health and motor performance outcomes related to participation. The four motor impairment categories identified in the Guide to Physical Therapist Practice, second edition, are incorporated into this chapter.1 A fifth category, the internal organs, has been added (Box 39-1). In addition to addressing the impact of these impairment categories on health and motor performance from a ventilatory perspective, we present a method to cross-reference impairment-based findings with functional limitations. Six common functional tasks that require the integration of breathing and movement are shown in Box 39-2. Children and adults with multiple physical challenges are patients in whom the interaction between respiratory control and postural control is particularly relevant. The role of multisystem interaction in effective breathing and postural control is an emerging field; hence it lacks rigorous evidence from experimental evaluation. Nonetheless, the physiologic evidence supporting the interactions among systems and their impact on breathing and posture (see Chapter 6) is compelling and sufficient to inform contemporary approaches to patient care in physical therapy practice. As an area of research, multisystem interaction represents a relatively new frontier that could have far-reaching implications for research in other physical therapy areas with respect to assessment, intervention, and evaluation. Ventilation is a three-dimensional activity. With each breath, the chest wall expands in the anterior-posterior plane, the inferior-superior plane, and the medial-lateral plane (Figure 39-1). The muscles that support breathing are resisted by gravity in one direction, assisted by gravity in another direction, and relatively unaffected in other directions. When a person is upright, superior expansion of the chest wall is resisted by gravity while inferior expansion is assisted, and other movements of the chest wall (anterior, posterior, and lateral expansion) are relatively unaffected by gravity. The adverse effects of gravity are counteracted by muscles that can function effectively in the presence of gravitational force. If the respiratory muscles become dysfunctional due to weakness, paralysis, or fatigue; or pathological conditions, the patient may no longer breathe effectively within gravity’s influence.2,3 Further, the impact of posture on breathing mechanics, as well as on cardiovascular function, has been well documented (see Chapter 20).4 Therefore, when physical therapists are positioning patients with impaired breathing mechanics or posture, they need to consider how gravity can affect the muscles that support breathing and posture in each body position, as well as how it affects oxygen transport overall. Gravitational force is crucial in the normal development of the skeleton. Typically developing infants move freely in and out of a range of body positions (prone, hands and knees, and standing), allowing gravity to alternately assist or resist their movements. Moving through these positions, the infant strengthens muscle groups and learns to interact with the gravitational force in his or her physical environment and compensate as needed.5 The development of the bones, muscles, and joints that constitute the trunk is influenced by genetic factors and movements performed in a gravitational field. Infants with limited ability to move and counteract gravity develop malaligned joints and impaired muscle support that, in turn, impair breathing mechanics, or vice versa.6–8 Cerebral palsy, spinal muscle atrophy, stroke, head trauma, and spinal cord injury are conditions that can cause such muscle imbalance in children.3 Weakness or fatigue of the trunk muscles can result from conditions outside the neuromuscular system9 (for example, oxygen transport deficits from bronchopulmonary dysplasia and congenital heart defects and nutrition-related deficits such as gastroesophageal reflux and malabsorption; see Chapters 6 and 32). Such symptoms can impair breathing mechanics, as well as muscle tone (as in hypertonicity or hypotonicity), and can contribute to deficits in motor planning and learning.10 Children who have impaired breathing mechanics and are recumbent for prolonged periods are exposed to abnormal gravitational stress. Over time, this leads to pathological changes and deformities such as retention of the primitive triangular shape of the newborn chest wall (Figure 39-2, A). In some cases, the child’s diaphragm remains functional in the presence of weak or paralyzed abdominal and intercostal muscles. In turn, this can affect skeletal development (Figure 39-2, B). Pronounced imbalance of the thoracic muscles can result in chest wall deformity, compromising the child’s ability to meet his or her ventilatory needs. Musculoskeletal abnormalities include anteriorly flared lower ribs, dynamic pectus deformity (most often, pectus excavatum; less often, pectus carinatum), laterally flared ribs, and chest wall asymmetry (Figure 39-2, B, C, D).6,8,11 These deformities have varying impact on ventilation depending on the gravitational consequences of each position. Understanding chest wall development in typically healthy children is essential for the physical therapist to assess chest wall deformities and their impact on oxygen transport.11 Chapter 37 describes normal growth and development of the cardiovascular and pulmonary systems during infancy and childhood. The present chapter takes this information a step further, and considers the impact of musculoskeletal and neuromuscular impairments on typical childhood development. Initially the newborn’s chest wall is triangular: narrow and flat in the upper portion and wider and rounded in the lower portion (Figure 39-3). The infant’s short neck reduces the effectiveness of the upper accessory muscles as ventilatory muscles. The infant’s arms tend to be flexed and adducted across the chest wall, hampering lateral or anterior movement of the chest wall. The infant, largely a diaphragmatic breather, shows disproportionate development of the lower chest wall, which promotes a triangular shape of the ribcage. Newborns breathe primarily in a single plane (inferior), rather than in three planes apparent in adults. From 3 to 6 months of age, the infant develops more trunk extension tone and spends more time on his or her elbows in prone. The baby begins to reach with the arms into the environment. This facilitates development of the anterior upper chest wall. Continuous stretching and upper extremity weight bearing helps to expand the anterior upper chest wall both anteriorly and laterally, while increasing posterior stabilization.5 An increase in the strength of the intercostal muscles and pectoralis muscles improves the infant’s ability to counteract gravity exerted on the anterior upper chest wall in the supine position, leading to the development of a slight convex configuration of the area and a rectangular shaping of the thorax from the frontal plane (Figure 39-4). The baby begins to breathe more effectively in multiple planes as the muscles’ length-tension relationships become more efficient. The next step in development occurs when the child assumes erect body positions independently (i.e., sitting, kneeling, and standing). Until this time, the ribs are aligned relatively horizontally, with narrow intercostal spacing (Figure 39-3). The newborn’s chest wall accounts for about one-third of the trunk cavity. As the child progressively moves against gravity, the ribs, with the aid of the abdominal muscles, rotate downward (more so in the longer lower ribs), creating the sharp angle of the ribs (Figure 39-5). This elongates the ribcage until it eventually occupies over half of the trunk cavity (Figure 39-6). Chest x-rays of newborns and adults, as well as pictures of infants, illustrate these developmental trends (Figure 39-7, A, B); details are further summarized in Table 39-1. Table 39-1 Typical Chest Wall Development from Infant to Adulthood Optimum respiratory function cannot be expected in a person with an underdeveloped or deformed chest wall, spine, or both.3 As long as the condition that caused the trunk muscle imbalance persists, regardless of whether that deficit was a neuromuscular disorder or an impairment in another motor impairment category (see Box 39-1), the chest wall and spine will likely develop atypically. Strategies to optimize trunk development include: Normal human movement reflects the interactions of multiple organ systems. If these interactions are atypical or inadequately compensated when impaired, motor impairments can result. Thus it is recommended that every physical therapy examination and evaluation include multisystem screening of the five impairment categories (Box 39-1) in order to determine the impact of each organ system on total motor performance. The following Soda Can Model of respiratory and postural control was developed to facilitate the clinician’s understanding of the multisystem interactions between the mechanics of breathing and the simultaneous needs of postural control The muscles of respiration are muscles of postural support and vice versa.14 Each muscle that originates from or inserts onto the trunk is both a respiratory muscle and a postural muscle. This duality of function means that respiratory and postural control should not be evaluated separately. External and internal forces that affect the function of the respiratory muscles also affect postural responses. The Soda Can Model illustrates this dual function. The shell of a soda or soft drink can is made of thin aluminum that is easily compressed when the can is open and empty. This same can, however, unopened and full, is almost impossible to compress or deform without puncturing the exterior shell. The strength of the can is derived from the positive pressure it exerts against atmospheric pressure and gravity through its closed (unopened) system (Figure 39-8, A). As soon as the closed system is compromised by either opening or puncturing the can, it loses its functional strength. It is no longer capable of counteracting the positive pressure forces acting on it. Once the can is opened, it is possible to compress it completely (Figure 39-8, B). The structural integrity of the trunk of the body is similar to that of the soda can described in the Soda Can Model. The skeletal support of the trunk is not inherently strong. The spine and ribcage alone cannot maintain their alignment against gravity without muscular support that enables them to generate pressure that is capable of countering gravitational pull. This is commonly observed in patients in intensive care. Weakened from prolonged illnesses and medical procedures, patients in the intensive care unit (ICU) typically slump into a forward, flexed posture when they sit up initially. This is associated with less ability to generate pressure through muscle activation to support alignment of the pelvis, spine, and ribcage in an upright position. In pediatric patients, the effects can be particularly alarming. Melissa provides such an example. She incurred a C5 spinal cord lesion from a vaginal birth injury and experienced marked collapse of the pelvis, ribcage, and spine when sitting upright. Melissa was incapable of making an effective inspiratory effort in this position, which explained her intolerance to upright activities. Figuratively, her “soda can” was compressed, and correspondingly, her breathing mechanics were severely compromised (Figure 39-8, C). The thoracic and abdominal chambers are separated by the diaphragm (Figure 39-9). The chambers are “sealed” at the top by the vocal folds, at the bottom by the pelvic floor, and circumferentially by the trunk muscles. Muscle support allows these chambers to match or exceed the positive pressure exerted on them by external forces to support the “flimsy” skeletal shell. The primary muscles involved in this support are the (1) intercostal muscles, which generate and maintain transthoracic pressure15; (2) the abdominal muscles, especially the transverse abdominus, which generate and maintain transabdominal pressure16,17; (3) the diaphragm, which regulates and uses the pressure in both chambers18,19; (4) the back muscles, which stabilize the spine to optimize its alignment and articulation with the ribcage20; (5) the pelvic floor muscles, which work synchronously with the diaphragm to support breathing and urinary control21,22; and (6) the vocal folds, which regulate intrathoracic pressure to stabilize the diaphragm and upper extremities.23 These muscles work synergistically to adjust the pressure in both chambers so that the demands of ventilation and posture are met simultaneously.24 The following synopsis of the biomechanics of breathing describes the interactions among the diaphragm, intercostals muscles, and abdominal muscles within the construct of a positive pressure chamber.24–27 The diaphragm is the primary muscle of respiration, but its function as a pressure regulating muscle may be less well recognized. The diaphragm separates the thoracic and abdominal cavities, thus creating and using the difference in pressure between the two chambers to support the simultaneous needs of respiration and trunk stabilization. The interactions among the diaphragm, intercostal muscles, and abdominal muscles, along with support from other trunk muscles, work synergistically to generate, regulate, and maintain thoracic and abdominal pressures necessary for the concurrent needs of breathing and motor control of the trunk.28 In summary, the diaphragm depends on the intercostal and abdominal muscles for effective and efficient breathing, and likewise, the trunk depends on the diaphragm for muscular support and pressure support during activities, particularly those with high postural demands.20,28–30 When the diaphragm contracts to effect inhalation, its central tendon descends inferiorly, creating negative pressure in the thoracic cavity. This draws air into the lungs due to the pressure difference with atmospheric pressure. Simultaneously, the intercostal muscles are activated to counter the negative pressure that draws them inward.7,31–34 Inadequate intercostal muscle support tends to collapse the chest wall, which in the long-term can cause musculoskeletal deformity (e.g., pectus excavatum) and secondary loss of chest wall compliance (see Figure 39-2, B).6,7,35,36 With descent of the diaphragm, positive pressure is created within the abdominal cavity and augmented by counterpressure exerted by the abdominal muscles, particularly the deepest muscle, the transverse abdominus.37 This pressure equals the negative pressure created in the thorax, based on Newton’s Law—that is, for every action, there is an equal and opposite reaction.38 Further, positive abdominal pressure provides a fulcrum for the diaphragm to stabilize its central tendon. This central stability mechanically supports the contractions of the lateral (peripheral) fibers up and over the abdominal viscera (lateral and superior chest wall expansion).24 That is, the coupling among the intercostals, abdominals, and diaphragm is greater than the sum of their parts for maximal respiratory function.26,39 The abdominal cavity has relatively higher pressure at rest than the thoracic cavity, as reflected by the position of the diaphragm within the trunk. Its dome is convex superiorly because the higher pressure from the abdominal cavity pushes it upward. In lung disease, the relationship between the abdominal and thoracic pressures may reverse and compromise the mechanics of breathing. For example, patients who have obstructive lung disease such as emphysema, trap air distally in the diseased lung segments.40 Air trapping and other manifestations of the condition cause the thoracic cavity to become the higher-pressure chamber at rest, pushing the diaphragm inferiorly and flattening its dome. The diaphragm’s mechanical support becomes compromised to the extent that it no longer functions well as an inspiratory muscle. To compensate, patients with end-stage emphysema tend to lean forward on extended arms, flex their trunks, and activate their abdominal muscles to increase abdominal pressure as a means of restoring the pressure relationship with the thoracic chamber. If successful, these patients are able to displace the dome of the diaphragm upward to enable it to function more effectively as an inspiratory muscle, thereby relieving dyspnea.41 Positive thoracic pressure is needed for both postural support of the upper trunk and expiratory maneuvers such as talking, coughing, and bowel and bladder evacuation.42–44 The vocal apparatus, including the vocal folds, provides the superior valve for pressure regulation of the thoracic chamber. If the vocal folds are compromised because of an impairment of the upper airway or because they are bypassed with a tracheostomy or endotracheal tube, the patient is incapable of generating and sustaining positive thoracic pressure support. After the patient has inhaled and achieved higher pressure inside than outside the lungs, the air is simply expired. There is no valve at the top to hold the pressure within the chest. Activities of the trunk that require positive thoracic pressure will be compromised. Without functioning vocal folds to regulate the controlled release of thoracic pressure during exhalation, the patient has no means of slowly, or eccentrically, releasing the air for speaking or performing eccentric trunk or extremity activities. The therapist may observe impairments such as dysfunctional speech and eccentric motor activity. The same is true for concentric contractions. Without the vocal folds being able to serve as the pressure valve, the patient is unable to generate intrathoracic pressure to elicit an effective cough.45 Similarly, if the patient is unable to close the glottis and direct thoracic positive pressure toward the pelvic floor, bowel and bladder evacuation may be compromised.46–49 Patients with tracheostomies often experience constipation. Bowel motility usually improves with decannulation when the vocal folds are restored as an active component of thoracic pressure regulation. The patient with compromised vocal folds can briefly generate positive expiratory pressure for activities such as coughing and yelling by concentrically contracting the trunk flexors, primarily the abdominal muscles, pelvic floor muscles, pectoralis muscles, latissimus dorsi muscles, or some combination, at peak inspiratory lung volume. This positive thoracic expiratory pressure, however, cannot be sustained because the expiratory pathway (e.g., tracheostomy tube or paralyzed vocal folds) is wider than the opening of the vocal folds, resulting in a larger volume of air to be expelled per second. Unlike patients with obstructive lung disease who have an abnormally prolonged expiration, patients with impaired pressure regulation at the top of the chamber have no mechanism to prolong exhalation for either eccentric or concentric motor tasks. In addition to regulating airflow from the lungs, the vocal folds have a role in generating increased thoracic pressure needed for stabilization associated with balance or activities such as lifting, pushing, and upper extremity weight-bearing activity.23,50–52 This response is called the glottal effort closure reflex.43 The vocal folds adduct and prevent air leakage while the chest wall, back, abdominal, and pelvic floor muscles contract to increase abdominal and thoracic pressures. Increased trunk pressure stabilizes the shoulder complex to enhance force production of the muscles of the upper extremities. For example, a tennis player with a strong serve often takes advantage of the glottal effort closure reflex. The server throws the ball up while taking a deep breath, then he or she closes the glottis at the peak of inspiration to trap the inspired air and activate the chest wall and abdominal muscles to increase thoracic pressure. When the tennis racket contacts the ball, the server explosively expels the air (usually with a grunt) to maximize the force production for the serve. This concept is used in every day life to perform tasks such as pushing open a heavy door, lifting a heavy box, or leaning on a table with one arm and reaching across to lift an object with the other arm. This mechanism is also used by infants to bear weight on their arms during activities such as crawling. These types of activities require full or partial glottal closure to increase the functional strength of the arms. This concept is consistent with that of the Soda Can Model, that is, providing a means of regulating pressure to augment functional strength and control.
Multisystem Clinical Implications of Impaired Breathing Mechanics and Postural Control
Breathing: A Three-Dimensional Gravity-Dependent Activity
Planes of Ventilation and Gravitational Influence
Effects of Gravity on Normal and Abnormal Chest Wall Development
Chest Wall Components
Infant
Adult
Size
Thorax occupies one third thoracic cavity
Thorax occupies more than half thoracic cavity
Shape
Triangular frontal plane, circular anterior-posterior plane
Rectangular frontal plane, elliptical anterior-posterior plane
Upper thoracic
Narrow, flat apex
Wide, convex apex
Lower thoracic
Circular, flared lower ribs
Elliptical, lower ribs integrated with abdominals
Ribs
Evenly horizontal
Rotated downward, especially inferiorly
Intercostal spacing
Narrow, limits movement of thoracic spine and cavity
Wide, allows for individual movement of ribs and spine
Diaphragm
Adequate, minimal dome shape
Adequate, large dome shape
Accessory muscles
Nonfunctional
Functional
Influence of Multisystem Interactions on Motor Performance: Relationship Between Respiratory and Postural Control
Soda Can Model of Respiratory and Postural Control
Structurally Weak, Yet Functionally Strong
Positive Pressure Support Instead of More Skeletal Support
Top and Bottom of the “Soda Can”: The Vocal Folds and Pelvic Floor
Vocal Folds and Vocal Apparatus
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree