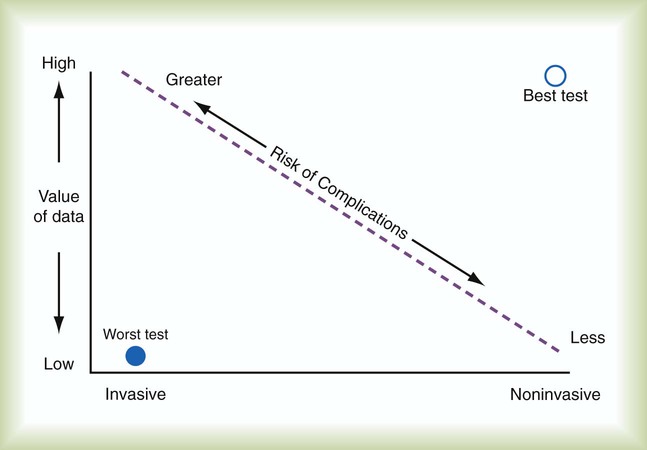
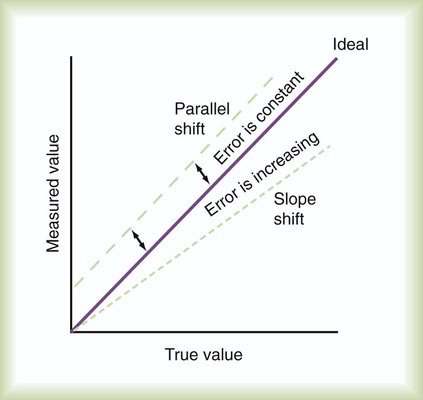
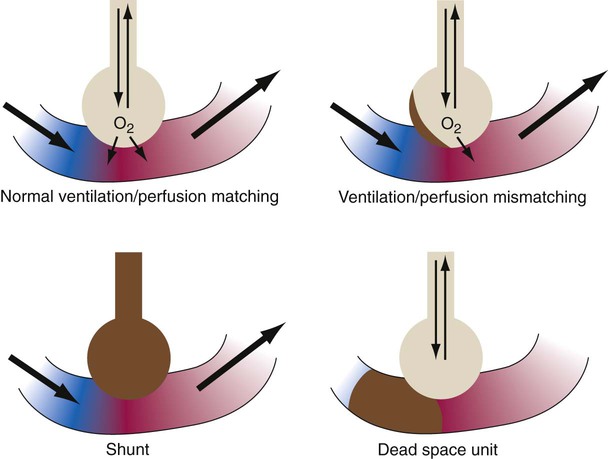
After reading this chapter you will be able to: The concept and purposes of monitoring have evolved over the past 50 years. The importance of monitoring was established with the advent of the intensive care unit (ICU) during the polio epidemic in the 1950s.1 Enhanced monitoring represents the main difference between a general hospital ward and the ICU. The purpose of monitoring is simple and clear: to measure in “real time” physiologic values that can change rapidly. The values can be analyzed and interpreted with the expectation that interventions such as fluid resuscitation, medication administration, or changes in ventilator settings can be made in time to prevent adverse consequences. Each monitoring test, procedure, or instrument carries certain risks and provides information that has value. There is an important balance between the risks and benefits of monitoring, especially when evaluating new monitoring techniques. Every test or monitoring technique should be continually judged for usefulness. Figure 46-1 depicts a continuum for judging the risk and benefit of tests, diagnostic procedures, and monitoring techniques. The most useful tests have little or no risk and high potential value. Less useful tests carry higher risk with little potential value. Use of a pulse oximeter probe carries little physical risk and provides valuable information about blood oxygenation (low risk-benefit ratio). However, there is a small but known risk of obtaining incorrect values with the instrument. Hemodynamic monitoring requires placement of a highly invasive Swan-Ganz catheter (pulmonary artery catheter) in the pulmonary artery to provide data that must be correctly interpreted. This type of monitoring should be undertaken only with an expectation of collecting important (high value) information. The risk-benefit ratio for pulmonary artery catheterization is high. For this reason and with fluid status data available from central venous pressure (CVP) monitoring, the widespread use of pulmonary arterial catheterization has markedly decreased.2 The measuring instrument can produce values that are shifted in a systematic way—consistently high or low or in error in relation to the magnitude of the signal. These shifts are referred to as either parallel or slope shifts (Figure 46-2). Generally, all values must be interpreted with a background of training and experience so that one can understand when a value is normal and when it should be considered abnormal. With the responsibility of detecting variations in physiologic data comes the responsibility of setting alarms appropriately. The alarms should be set to detect monitored values that require attention. Monitors also detect the artifacts, factitious events, and random variation often seen in the ICU. The ICU is a noisy environment with many alarms sounding that may not require immediate attention. Ventilators respond to coughs, and electrocardiographs (ECGs), oximeters, and vascular pressure monitors sound alarms with physical movements of the patient. Practitioners must develop mental filtering skills to evaluate true and false alarms and to know when to correct the alarm settings, when to wait for multiple alarms, and when to be concerned about an alarm signal (Box 46-1). The best monitor continues to be the caregiver: the respiratory therapist (RT), nurse, and physician. Changes in the patient’s condition are detected and monitored most directly by means of patient assessment in the ICU. Chapter 15 describes the important details and bedside assessment skills required of caregivers in the ICU. This assessment is valuable because the information is obtained by a decision maker—the caregiver. The art of the physical examination is being lost with the use of monitoring instruments. A common observation is a group of caregivers staring intently at monitors while a patient is waving for attention. Nevertheless, monitors continue to improve, and they are often relied on to substitute for skills of observation. Monitors are needed for two main reasons: (1) continuous assessment (humans need breaks) and (2) measurement of values that caregivers cannot detect, such as ECG findings or airway pressure. The lungs contain 300 million alveoli, but a basic model of lung injury reduces a lung disorder to three types of injured lung units (Figure 46-3): (1) alveoli that are ventilated but not perfused (dead space units), (2) alveoli that are perfused but not ventilated (shunt units), and (3) alveoli that are receiving either partial ventilation or partial perfusion ( The most important function of the lungs is uptake of O2 from air into the arterial blood and disposal of carbon dioxide (CO2) from mixed venous or pulmonary artery blood into the environment. Arterial blood gas (ABG) values contain this gas exchange information. A typical ABG report includes PaO2, PaCO2, pH, a calculated HCO3−, and an estimated base excess or deficit. ABG samples can be obtained quickly and analyzed rapidly. The typical absolute values, predicted values, derangements including compensation, and basic interpretation of ABGs are described in Chapter 18. However, ABGs do not tell the complete story; other values assessing gas exchange that are actively obtained or calculated are discussed in this section. The goal of breathing and circulation is adequate tissue oxygenation. All organs require O2 delivery that meets O2 use demands; the brain and kidneys have particularly high requirements. An important innovation in monitoring is the use of oximetry—a color spectrum measurement of pulsing arterial blood is used for continuous assessment of arterial oxygenation (SpO2). The human eye is not good at detecting or quantifying arterial hypoxemia. Frank cyanosis does not develop until there is at least 5 g/dl of deoxyhemoglobin in the blood.3 The threshold at which cyanosis becomes apparent is affected by skin perfusion, skin pigmentation, and hemoglobin concentration. ABG analysis has been the accepted method of detecting hypoxemia in critically ill patients, but obtaining arterial blood can be painful and cause complications, and ABG analysis does not provide immediate or continuous data. For these reasons, SpO2 has become the standard for a continuous, noninvasive assessment of SaO2. SpO2 does not measure PaCO2, and patients breathing an elevated FiO2 can build up CO2 (increased PaCO2), although SpO2 values are acceptable. Ventilatory failure may go unnoticed unless ABGs are measured. Tissue O2 sensors designed to measure SaO2 of muscle or the brain were developed more recently.4 Brain oxygenation is crucial, and deep muscle tissue in compartment syndromes can become deoxygenated. This tissue oxygen sensing technique involves positioning of an emitter and detector (of usually four wavelengths) on the skin surface over the tissue or organ of interest. Light from the emitter reflects from tissue at a depth of one-third the distance between the emitter and detector. The light received by the detector is read, and algorithms determine tissue oxygenation, not SpO2. Although SpO2 has been universally adopted, it does have limitations (Box 46-2).5,6 Motion artifact is an important problem, resulting in inaccurate readings and false alarms. Motion artifacts are common because of shivering, seizure activity, pressure on the sensor, or transport of the patient. The choice of probe site may also affect accuracy. Finger probes appear to be more accurate than forehead, nose, or earlobe probes during low perfusion states. Intense daylight and fluorescent, incandescent, xenon, and infrared light sources have caused errors in SpO2 readings. Anemia and deeply pigmented skin can affect the accuracy of SpO2; however, the effect of anemia is not clinically significant until the hemoglobin level is markedly reduced. Carboxyhemoglobin and methemoglobin can produce falsely high SpO2 values, and some colors of nail polish, particularly blue, green, and black, interfere with light transmission and absorbency, as do some blood-borne dyes, such as indocyanine green and methylene blue, which tend to produce falsely low SpO2 values. Although rare, exposure to numerous toxins and drugs, including topical benzocaine, can elevate methemoglobin and produce falsely elevated SpO2 values.
Monitoring the Patient in the Intensive Care Unit
 Discuss the principles of monitoring the respiratory system, cardiovascular system, neurologic status, renal function, liver function, and nutritional status of patients in intensive care.
Discuss the principles of monitoring the respiratory system, cardiovascular system, neurologic status, renal function, liver function, and nutritional status of patients in intensive care.
 Identify the risks and benefits of intensive care unit (ICU) monitoring techniques.
Identify the risks and benefits of intensive care unit (ICU) monitoring techniques.
 Explain why the caregiver is the most important monitor in the ICU.
Explain why the caregiver is the most important monitor in the ICU.
 Describe how to evaluate measures of patient oxygenation in the ICU.
Describe how to evaluate measures of patient oxygenation in the ICU.
 Explain why PaCO2 is the best index of ventilation for critically ill patients.
Explain why PaCO2 is the best index of ventilation for critically ill patients.
 Describe the approach used to evaluate changes in respiratory rate, tidal volume, minute ventilation, PaCO2, and end-tidal PCO2 values for monitoring purposes.
Describe the approach used to evaluate changes in respiratory rate, tidal volume, minute ventilation, PaCO2, and end-tidal PCO2 values for monitoring purposes.
 Identify monitoring techniques used in the ICU to evaluate lung and chest wall mechanics and work of breathing.
Identify monitoring techniques used in the ICU to evaluate lung and chest wall mechanics and work of breathing.
 Discuss the importance of monitoring peak and plateau pressures in patients receiving mechanical ventilatory support.
Discuss the importance of monitoring peak and plateau pressures in patients receiving mechanical ventilatory support.
 Identify monitoring techniques that have become available more recently, such as lung stress and strain, functional residual capacity, stress index, electrical impedance tomography, and acoustic respiratory monitoring.
Identify monitoring techniques that have become available more recently, such as lung stress and strain, functional residual capacity, stress index, electrical impedance tomography, and acoustic respiratory monitoring.
 Describe the approach used to interpret the results of ventilator graphics monitoring.
Describe the approach used to interpret the results of ventilator graphics monitoring.
 Describe the cardiovascular monitoring techniques used in the care of critically ill patients and how to interpret the results of hemodynamic monitoring.
Describe the cardiovascular monitoring techniques used in the care of critically ill patients and how to interpret the results of hemodynamic monitoring.
 Discuss the importance of monitoring neurologic status in the ICU and the variables that should be monitored.
Discuss the importance of monitoring neurologic status in the ICU and the variables that should be monitored.
 Discuss evaluation of renal function, liver function, and nutritional status in the ICU.
Discuss evaluation of renal function, liver function, and nutritional status in the ICU.
 List and discuss the use of composite and global scores to measure patient status in the ICU, such as the Murray lung injury score and the APACHE severity of illness scoring system.
List and discuss the use of composite and global scores to measure patient status in the ICU, such as the Murray lung injury score and the APACHE severity of illness scoring system.
 Discuss monitoring and troubleshooting of the patient-ventilator system in the ICU.
Discuss monitoring and troubleshooting of the patient-ventilator system in the ICU.
Principles of Monitoring
Pathophysiology and Monitoring
 mismatch). In terms of treatment options,
mismatch). In terms of treatment options,  mismatching is more responsive to oxygen (O2) therapy than shunt or dead space units. However, all three forms of disordered lung units display reduced O2 saturation. Within the context of this model, treatment should be aimed at the source of the disorder and not an attempt to “fix” the arterial partial pressure of oxygen (PaO2) or SpO2.
mismatching is more responsive to oxygen (O2) therapy than shunt or dead space units. However, all three forms of disordered lung units display reduced O2 saturation. Within the context of this model, treatment should be aimed at the source of the disorder and not an attempt to “fix” the arterial partial pressure of oxygen (PaO2) or SpO2.
Respiratory Monitoring
Gas Exchange
Monitoring Oxygenation
Arterial Pulse Oximetry
Monitoring the Patient in the Intensive Care Unit

 )
) )
)
 ) is the volume of O2 consumed by the body in milliliters per minute. Normal resting
) is the volume of O2 consumed by the body in milliliters per minute. Normal resting  is approximately 250 ml/min, and
is approximately 250 ml/min, and  increases with activity, stress, and temperature. The acquisition of O2 from the lungs into the circulatory system is described by the Fick equations:
increases with activity, stress, and temperature. The acquisition of O2 from the lungs into the circulatory system is described by the Fick equations:

