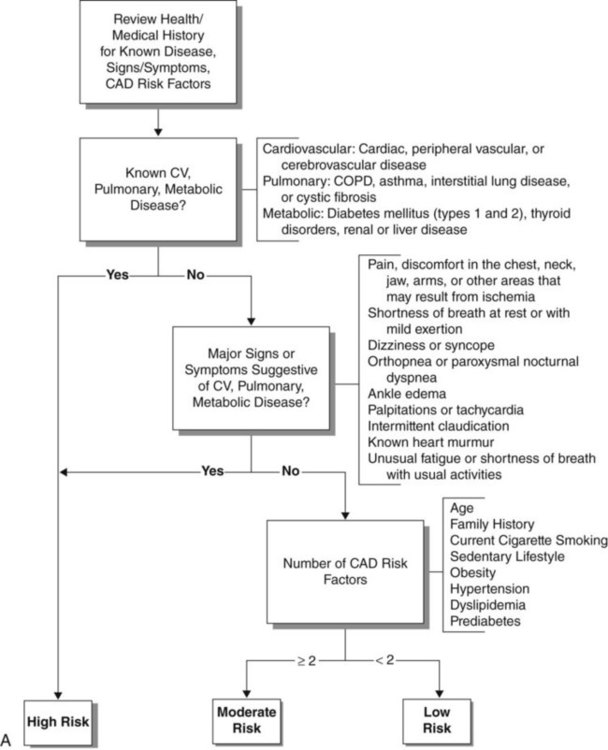
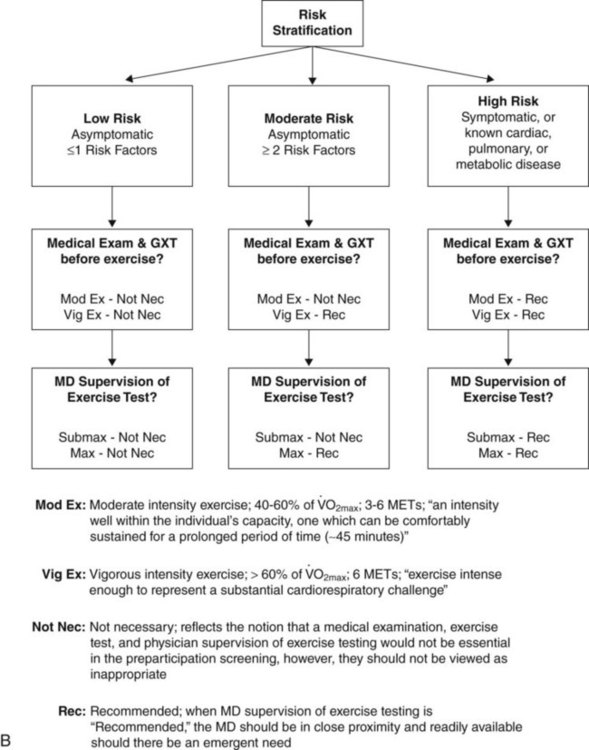
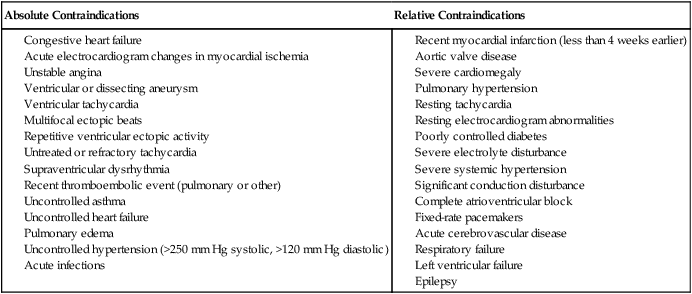
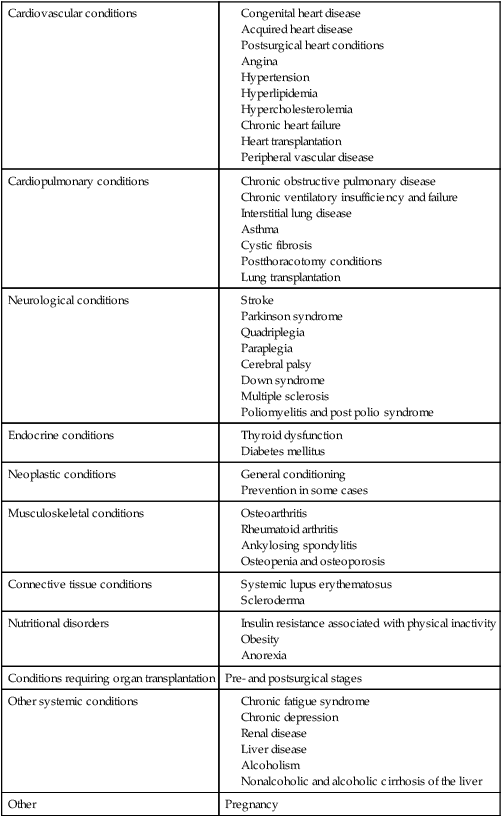
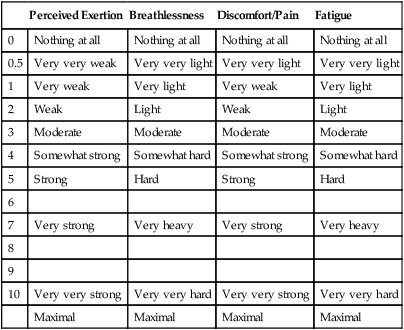
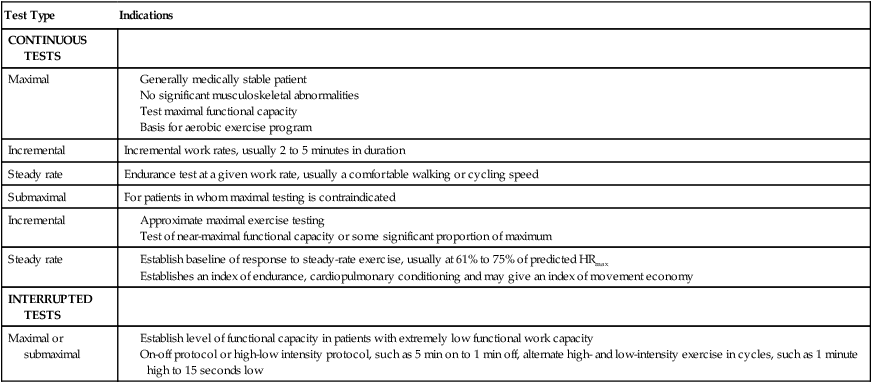
This chapter describes the principles and practices for exploiting the preventive, acute, and long-term effects of mobilization, exercise, and training. Mobilization and exercise are prescribed to elicit whichever of these distinct effects is indicated. They are prescribed on the basis of their indications, contraindications, and potential side effects for a given individual. Exercise to exploit each of these effects can be prescribed to address limitations in specific organ systems, as well as augment activity ability and participation. Chapters 24 and 25 expand on these topics, describing special considerations for patient populations with an emphasis on targeting exercise testing and prescription for training based on people with conditions rather than for the condition(s) a patient has. Exercise testing can pose a risk to the patient, so exercise testing must have clear indications, and any contraindications must be ruled out. On the other hand, earlier guidelines for exercise testing in patients, particularly those with cardiac conditions, were too conservative.1 Patients can be exercised aggressively provided that the indications are based on a comprehensive assessment and a judiciously selected exercise test and protocol and provided that the patient is appropriately monitored throughout testing. The American College of Sports Medicine (ACSM)2 has developed an algorithm (Figure 19-1, A) to determine the risk for cardiovascular events during exercise testing (Table 19-1) as well as guidelines for test selection and level of supervision required based on the risk assessment (Figure 19-1, B). As shown in Figure 19-1, A, patients with known cardiovascular, metabolic, or pulmonary disease are classified as having a high risk for sustaining a cardiovascular event during exercise. For these individuals, a comprehensive medical examination and physician-supervised exercise testing is recommended before starting a moderate or vigorous intensity exercise program (see Figure 19-1, B). For individuals who do not have the conditions listed above, the remainder of the algorithm describes how patient signs and symptoms and coronary artery disease risk factors determine the risk classification and exercise testing and supervision requirements. Physical therapists need to screen patients systematically before exercise testing or prescription. Table 19-1 Cardiovascular Risk Factor Threshold for Risk Stratification aProfessional opinions vary regarding the most appropriate markers and thresholds for obesity; therefore allied health professionals should use clinical judgment when evaluating the risk factor. Modified from the American College of Sports Medicine. (2010). Guidelines for exercise testing and prescription, ed 8. Philadelphia: Williams and Wilkins. Numerous conditions, including nonprimary cardiovascular and pulmonary conditions, have been shown to benefit from the long-term effects of aerobic exercise (Table 19-2) (see Chapters 24 and 25). Thus for each patient with these conditions, the exercise prescription differs. Comparable with prescribing mobilization in acute conditions, prescribing exercise for long-term adaptations is based on the patient’s presentation, history, premorbid status and conditioning level, lab and investigative reports related to physiological reserve capacity, the exercise test, and the goals of the exercise prescription. To promote health, as few as 30 minutes of moderately intense exercise a day on most days of the week is required.3 However, based on ACSM (2010)2 guidelines, optimal aerobic exercise adaptation requires an exercise stimulus of 70% to 85% of HRmax for 20 to 40 minutes, 3 to 5 times a week for at least 6 to 8 weeks. However, the effect of exercise intensity on Table 19-2 Chronic Conditions That Benefit from the Long-Term Effects of Mobilization and Exercise The indications for exercise testing are numerous (Box 19-1). They range from quantifying maximum functional, aerobic, or oxygen transport capacities to assessing endurance during low-level activities of daily living (ADLs). The capacity of the oxygen transport system is the most important determinant of maximum oxygen uptake in healthy people. Metabolic studies including Contraindications to exercise testing and, in particular, maximal testing are classified as relative or absolute (Box 19-2). Absolute contraindications prohibit the safe conduction of an exercise test, whereas the presence of relative contraindications requires that the test, protocol, physiological variables monitored, or end point of the test be modified. Both the indications for the test and any contraindications must be clearly established before performing an exercise test. The guidelines used to test and train healthy people with no disease are not directly generalizable to patients with chronic illness who are medically stable. Because of functional impairments in these patients (secondary to cardiopulmonary, cardiovascular, neuromuscular, or musculoskeletal dysfunction), exercise testing and training must be modified. Moreover, patients who are physically challenged experience more subjective symptoms in response to exercise than do healthy people, so monitoring the subjective responses to exercise is essential. The Borg scale of rating perceived exertion can be modified for clinical use to score breathlessness, discomfort, pain, and fatigue (Table 19-3).9,10 If the end points of the scale have been well described and are understood by the patient, the ratings can be used to compare the patient’s subjective exercise responses over repeated tests. The patient’s subjective reports can be correlated with the exercise response and so can provide a basis for exercise prescription as well as avoiding adverse responses. Table 19-3 Subjective Scales of Exercise Responses There are numerous variants of standard exercise tests (Table 19-4). They are categorized as continuous tests or interrupted tests. Continuous tests include maximal and submaximal incremental tests and steady-rate tests; interrupted tests include maximal interval and submaximal interval tests. Interrupted tests are designed for patients with low functional work capacity who cannot sustain prolonged periods of aerobic exercise. These patients can perform more work over time when the workload is intermittent. Specifically, the test allows for alternating fixed periods of work and rest or of high and low intensities of exercise. The proportion of work to rest or high to low exercise intensity is set according to the patient’s level of impairment. One patient, for example, may be able to tolerate 3 to 5 minutes of relatively high-intensity work alternated with bouts of 1 to 2 minutes of low-intensity work, whereas another patient may be able to tolerate only 1 minute of low-intensity work alternated with 10 to 20 seconds of rest. Table 19-4 Exercise Tests Applicable to Patient Populations For maximal standardization and the capacity to perform comprehensive monitoring, stationary exercise modalities such as the treadmill, ergometer, or step are recommended. However, there may be indications to perform an exercise test without a modality, such as the 12-minute walk test or some variant like 6 or 3 minutes.11–13 Standardization of such tests, however, is more challenging. Practice has a significant effect on the results of the 12-minute walk test, so this test must be repeated to achieve a valid test. Also, the instructions for this test are less well standardized clinically than are those for the treadmill or ergometer; this jeopardizes stringent test control and thus must be tightly standardized.14 Like other diagnostic and testing procedures, the validity and reliability of the exercise test depend on standardization of the procedures. Test validity and reliability can easily be compromised in the absence of repeated testing and controls.15,16 Early ergometer training responses at rest along with submaximal heart rates and reduction in EMG activity in the arms and legs can reflect familiarization.17 Repeated exercise tests reflect the marked effects of practice. Practice reduces energy output, improves practice-related coordination, and reduces muscle activation.18 However, with good quality control, a test’s validity and reliability can be maximized, even in patients with severe disease such as chronic heart failure.19 The pre-exercise test conditions and the preparation and testing procedures must be standardized (Box 19-3). The test is terminated as soon as the sign or symptom criteria for terminating the test are reached or when the criteria for prematurely terminating the test are reached (Table 19-5). Recording the test conditions and procedures in detail is essential. An example of an exercise test data sheet that can be modified to any testing protocol that includes an exercise modality is shown in Figure 19-2, A. Many patients are unable to be exercise-tested using a modality; these patients can walk on a marked circuit, and the results are recorded on an exercise test data sheet similar to the one shown in Figure 19-2, B. Systematic and detailed record keeping will maximize the test’s validity and its interpretation and will ensure that the same procedures are used in follow-up tests, thereby maximizing the comparability of the results of repeated tests. It is imperative that retests be comparable in every respect to the original test in terms of the preparation of the patient and the procedures. Table 19-5 Criteria for Prematurely Terminating an Exercise Test Symptomatic supraventricular tachycardia Sinus tachycardia displacement (3 mm) horizontal or downsloping from rest
Mobilization and Exercise
Testing and Training
Pre-exercise Test Evaluation
Pre-exercise Screening for Minimizing Cardiovascular Risk During Testing
Risk Factors
Defining Criteria
Positive
Age
Men ≥45 years; Women ≥55 years
Family history
Myocardial infarction, coronary revascularization, or sudden death before 55 years of age in father or other male first-degree relative, or before 65 years of age in mother or other female first-degree relative
Cigarette smoking
Current cigarette smoker or those who quit within the previous 6 months or exposure to environmental tobacco smoke
Sedentary lifestyle
Not participating in at least 30 minutes of moderate intensity (40% to 60%  ) physical activity on at least 3 days of the week for at least 3 months
) physical activity on at least 3 days of the week for at least 3 months
Obesitya
Body mass index: ≥30 kg × m2
– or –
Waist girth:
>102 cm (40 inches) for men
>88 cm (35 inches) for women
Hypertension
Systolic blood pressure ≥140 mm Hg and/or diastolic ≥90 mm Hg, confirmed by measurements on at least two separate occasions, or on antihypertensive medication
Dyslipidemia
Low-density lipoprotein (LDL-C) cholesterol ≥130 mg × dL-1 (3.37 mmol × L-1) – or –
High-density lipoprotein (HDL-C) cholesterol <40 mg × dL-1 (1.04 mmol × L-1) – or –
On lipid-lowering medication
If total serum cholesterol is all that is available, use ≥200 mg × dL-1 (5.18 mmol × L-1)
Prediabetes
Impaired fasting glucose (IFG) = fasting plasma glucose ≥100 mg × dL-1 (5.50 mmol × L-1) – or –
Impaired glucose tolerance (IGT) = 2-hour values in oral glucose tolerance test (OGTT) ≥140 mg × dL-1 (7.70 mmol × L-1) but <200 mg × dL-1 (11.00 mmol × L-1) confirmed by measurements on at least two separate occasions
Negative
High-serum HDL cholesterol
≥60 mg × dL-1 (1.55 mmol × L-1)
Exercise Testing
 and on CO continues to be studied.4 Improvement in
and on CO continues to be studied.4 Improvement in  does not appear to be achieved by the same central and peripheral adaptations across a range of exercise intensities. Some individuals have high
does not appear to be achieved by the same central and peripheral adaptations across a range of exercise intensities. Some individuals have high  , CO, and SV without a history of training.5 This may reflect a genetically determined greater blood volume.
, CO, and SV without a history of training.5 This may reflect a genetically determined greater blood volume.
Cardiovascular conditions
Cardiopulmonary conditions
Neurological conditions
Endocrine conditions
Neoplastic conditions
Musculoskeletal conditions
Connective tissue conditions
Nutritional disorders
Conditions requiring organ transplantation
Pre- and postsurgical stages
Other systemic conditions
Other
Pregnancy
 provide a link between impairment and functional capacity6 and can distinguish cardiac versus pulmonary contribution to exercise intolerance.7
provide a link between impairment and functional capacity6 and can distinguish cardiac versus pulmonary contribution to exercise intolerance.7  studies require the use of a nose clip or face mask, which may contribute to perceived exertion in addition to the increased dead space that is created by the inspiratory circuit. In a study comparing the two devices in patients with congestive heart failure, no difference in gas-exchange measurements was observed.8 Perceived exertion, however, was not reported. This is an important finding given that
studies require the use of a nose clip or face mask, which may contribute to perceived exertion in addition to the increased dead space that is created by the inspiratory circuit. In a study comparing the two devices in patients with congestive heart failure, no difference in gas-exchange measurements was observed.8 Perceived exertion, however, was not reported. This is an important finding given that  is a strong predictor of survival (see Chapter 24).
is a strong predictor of survival (see Chapter 24).
Contraindications to Exercise Testing
Perceived Exertion
Breathlessness
Discomfort/Pain
Fatigue
0
Nothing at all
Nothing at all
Nothing at all
Nothing at all
0.5
Very very weak
Very very light
Very very light
Very very light
1
Very weak
Very light
Very weak
Very light
2
Weak
Light
Weak
Light
3
Moderate
Moderate
Moderate
Moderate
4
Somewhat strong
Somewhat hard
Somewhat strong
Somewhat hard
5
Strong
Hard
Strong
Hard
6
7
Very strong
Very heavy
Very strong
Very heavy
8
9
10
Very very strong
Very very hard
Very very strong
Very very hard
Maximal
Maximal
Maximal
Maximal
Standardization of Exercise Tests and General Procedures
Test Type
Indications
CONTINUOUS TESTS
Maximal
Incremental
Incremental work rates, usually 2 to 5 minutes in duration
Steady rate
Endurance test at a given work rate, usually a comfortable walking or cycling speed
Submaximal
For patients in whom maximal testing is contraindicated
Incremental
Steady rate
INTERRUPTED TESTS
Maximal or submaximal
Miscellaneous
General signs and symptoms
Electrocardiogram signs
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree