The routine application of mobilization and exercise should be distinguished from the prescriptive application of mobilization and exercise; the three objectives of prescribing mobilization and exercise for the purpose of maximizing oxygen transport are differentiated in this chapter. The detrimental multisystem effects of prolonged sedentary activity and restricted activity (bed rest) in the general population are outlined, and techniques to counter those effects are described. The acute and chronic responses to exercise described in this chapter are typical for individuals without pathology. Chapter 19 outlines testing and training prescription principles and practical details for exercise testing and prescription. Special considerations in common patient populations with respect to exercise testing and training prescription are described in Chapters 24 and 25. Mobilization is the therapeutic and prescriptive application of low work load activity in the management of cardiovascular and pulmonary dysfunction. Primarily, the goal of mobilization is to exploit the acute effects of exercise in order to optimize oxygen transport. Although this activity is considered low work load, it can elicit high patient-specific relative metabolic demand. Even a relatively low dose of a mobilization stimulus can impose considerable metabolic demand on a patient with cardiovascular or pulmonary compromise, which is why it is prescribed for patients who are acutely ill. Mobilization is also used because of its beneficial effects on other organ systems such as the musculoskeletal, neurological, integumentary, gastrointestinal, and renal systems. Whenever possible, mobilization is performed in the upright position, which is the physiological position (Chapter 20), to optimize gravitational stress on fluid shifts and central and peripheral hemodynamics. Mobilization is thus prescribed as both a gravitational stimulus and an exercise stimulus. Although specific principles of training have been designed for athletes involved in performance-based activities, these principles also apply to any patient that physical therapists encounter. Training in both cases, is defined as the systematic application of progressive exercise stimuli to elicit a specific physiological, functional, or skill-based goal (or goals). Typically, to achieve specific patient-based goals, the application of multiple exercise modes and training guidelines is required. This type of training often involves both aerobic and anaerobic exercise using cyclic and resistance-based exercises. Application of training principles to exercise testing and prescription is discussed further in Chapter 19. Physiological response can vary in deconditioned people where a given work rate is perceived as highly strenuous, yet the absolute work rate is relatively low. These responses can be markedly altered in people with a range of pathologies (depending on their types and severities) and these differences need to be anticipated and considered (see Chapters 24 and 25) in the assessment of a patient. For evaluation, exercise tests can serve as standardized outcome measures. As evaluation tools, tests are repeated periodically (e.g., every few weeks) in order to progress the exercise or training prescription until the target conditioning goal is achieved. Special attention is paid in these cases to pre-exercise conditions and the standardization of both exercise procedures and measurement procedures (Chapter 19). Often for people with chronic conditions, many of whom may be older, submaximal tests can be used to compare responses from one time to another for given work rates. In other cases, the physical therapist may wish to estimate In patients whose oxygen transport capacity is reduced or threatened, mobilization and exercise constitute a metabolic load that is superimposed on other factors that increase metabolic cost (Table 18-1). Hospitalized patients may be hypermetabolic. In addition to their basal metabolic demands, their energy demands are increased secondarily to factors such as pain, anxiety, increased body temperature, healing and repair processes, increased work of breathing, and increased work of the heart, as well as in response to interventions and procedures such as physical therapy. The goal, therefore, in prescribing mobilization and exercise is to ensure a safety margin wherein the patient’s demand for oxygen does not exceed the available normal supply or delivery. This can be indicated clinically if the patient’s oxygen transport levels worsen by either objective or subjective measurement. Table 18-1 Factors That Contribute to Increased Metabolic Demand and Oxygen Consumption in Patient Populations Alerting, noxious, and painful responses to routine nursing, medical, and physical therapy interventions, including injections, insertion of lines, procedures, and neurological checks Feeding, enterally or parenterally Being handled physically (by health care workers) Changing body position (passive, active assist, or active changes) Range of motion exercises (passive, active assist, or active) Several interventions can increase Metabolic demand and The typical method for prescribing exercise to achieve desired acute and long-term adaptations is longer duration, whole-body aerobic exercise at a moderate-vigorous intensity. This type of stimulus appropriately optimizes both central (cardiac, blood volume, oxygen delivery) and peripheral (oxygen extraction, glycolytic/mitochondrial enzyme function, capillarization) components for increasing The integrity of the cardiopulmonary unit is fundamental to maximize oxygen transport and cellular respiration. Oxygen is continuously being used by every cell in the body for oxidative phosphorylation and the synthesis of adenosine triphosphate (ATP). The splitting of a phosphate bond from ATP to form adenosine diphosphate yields a considerable amount of energy for metabolism. The energy for this process comes from the reduction of hydrogen in the formation of water and carbon dioxide, which are the end products of the Krebs cycle and the electron transfer chain (i.e., cellular respiration). These metabolic processes, which make up oxidative phosphorylation, take place in the mitochondria of the cells (see Chapter 2). The balance between oxygen consumption and oxygen delivery is precisely regulated to ensure not only that there is an adequate supply of oxygen but also that, under typical resting conditions, approximately four times as much oxygen is delivered to the tissues as is used. This safety margin permits the immediate availability of oxygen when the system is perturbed by physical, gravitational, or psychological challenges (see Chapter 2). Lactic acid accumulates in the blood during anaerobic metabolism. In healthy, untrained individuals lactic acid increases exponentially at an exercise intensity of about 55% of maximal aerobic power.6 The first line of defense is the response to an increase in pericellular pH. The concentration of carbon dioxide is increased, and this, as a result of the decrease in pH, facilitates the dissociation of oxygen from hemoglobin (i.e., it shifts the oxyhemoglobin dissociation curve to the right). CO, the product of stroke volume and heart rate (SV × HR), increases commensurate with metabolic demand. The immediate response to oxygen utilization and lowered tissue oxygen is an increase in CO to increase DO2. This averts arterial desaturation that is not typically observed in health, even with extreme exertion. With progressive exercise intensity, SV increases disproportionately at lower intensities to increase CO, with HR contributing to a greater extent at moderate and high exercise intensities. However, older individuals exercising at high intensity in upright positions rely more on the Frank-Starling effect than on HR.7 In health, exercise-induced cardiac fatigue has been proposed as a limiter to prolonged exercise.8 The mechanisms of the associated reduced left ventricular systolic and diastolic function are unclear. The increase in systemic CO results in increased venous return and pulmonary CO. The SV plateaus at 40% of Conversely, the absence of gravitational stress and exercise stress are the two primary factors contributing to impaired oxygen transport secondary to bed rest deconditioning. Exploiting both gravitational and exercise stress to prevent cardiovascular and pulmonary dysfunction is thus indicated. Further, mobilization and exercise are the two most vital physiological interventions available to the physical therapist for remediating cardiovascular and pulmonary dysfunction. Body position has marked effects on pulmonary and cardiovascular function (Chapter 20) and thus on exercise performance. The more acutely ill a patient is, the more important it is that upright body positioning be coupled with mobilization to increase aerobic capacity and tolerance to exercise stress. The degree to which this is done, however, depends on the patient’s status and ongoing monitoring (see Chapters 16, 34, and 35). The prescription of exercise is fundamental to the management of primary and secondary cardiovascular and pulmonary dysfunction. Guidelines have been well developed for prescribing exercise to maximize functional work capacity or aerobic power for healthy people and individuals with chronic heart and lung conditions.14–21 As clinical exercise specialists, physical therapists strive to take advantage of the effects of exercise in most patients and adapt the prescription based on the patient’s clinical presentation and needs. Exercise training is typically based on a person’s responses to a maximum graded exercise test. Although somewhat less precise, exercise training intensity can be prescribed based on a proportion of the individual’s age-predicted maximum heart rate provided there is no significant medical history. Submaximal exercise testing is often indicated for patients with severely impaired functional work capacity because of the inherent risks associated with maximal testing and the potential for invalid test results.22 Submaximal exercise testing has had a greater role in patient assessment and evaluation than as a basis for exercise prescription. Because of the greater utility of submaximal exercise testing in patient populations, guidelines for the latter warrant being better elucidated. The prescription of mobilization for the patient with acute cardiovascular and pulmonary dysfunction has been a relatively neglected research priority when compared with the number of studies concerning the prescription of exercise. This is surprising, given that early mobilization is generally a key component of cardiovascular and pulmonary physical therapy for patients who are acutely ill. Orlava (1959)23 was among the first to report the beneficial use of mobilization to manage acute cardiovascular and pulmonary compromise; specifically, bronchopulmonary pneumonia. In addition, the physiological literature has long supported an unequivocal role for therapeutic mobilization to maximize oxygen transport in patients with acute cardiovascular and pulmonary dysfunction.24 Even for patients who are critically ill, the goal of mobilization is to evaluate the patient’s responses with respect to oxygen transport reserve capacity and use this as a basis for estimating the limits of a patient’s physiological capacity to be mobilized, with a view to returning the patient to living within the community. The more critically ill the patient, the greater the need to assess the relationship between the patient’s Unlike exercise testing and prescription for the patient with chronic cardiovascular and pulmonary conditions, the patient with acute dysfunction is not exercise-tested in the conventional manner because of understandable risk and the patient’s incapacity to perform such a test. Given the profound and direct effects of mobilization and exercise on cardiovascular and pulmonary function, the physical therapist needs to identify the specific effects of exercise required and define the optimal therapeutic stimulus (i.e., the stimulus that yields the maximal benefit to oxygen transport with the least risk). The parameters for the mobilization prescription are based on factors other than a maximal or peak effort (see Chapters 16, 34, and 35). Acute and chronic cardiovascular and pulmonary pathology have the additional challenges of compromising functional capacity in two ways. First, in acute illness, the patient tends to be recumbent in bed a great proportion of the time; second, in both acute and chronic illnesses, the patient’s physical activity is reduced. Recumbency and restricted mobility have physiologically distinct effects on oxygen transport that contribute jointly to bed rest deconditioning; recumbency, however, has been considered to be the primary determinant of bed rest deconditioning.26–28 The impact of these factors is exaggerated in smokers, young people, older adults, obese individuals, and patients who are mechanically ventilated. The goals of mobilization and exercise are directed at correcting impairments and enhancing the patient’s capacity for activity and participation (see overview of the WHO International Classification of Function, Disability and Health in Chapters 1 and 17). Outcomes related to improving abilities and participation include self-care, home management, return to work, and resumption of avocational activities. Return to work warrants special mention. Return to work is often related to oxygen transport capacity in terms of aerobic and muscle power. However, there are economic, psychosocial, and environmental factors that need to be considered. These factors, too, should be part of the overall assessment and incorporated when setting overall goals and establishing the appropriate outcomes for a given patient. The preventive effects of exercise are evident in prehabilitation. The term prehabilitation can be used to refer to patient conditioning before a surgical intervention or hospital admission.29 Individuals can be prescribed exercise programs commensurate with their age, functional status, and anticipated procedure or surgery. The purpose is to reduce complications, speed recovery, minimize the time until discharge, and promote a complete return to daily living as soon as possible. When prescribing exercise to elicit its optimal preventive effects, the physical therapist needs to consider the same variables as when prescribing exercise for its beneficial acute and long-term effects—that is, the patient’s age, capabilities, premorbid functional work capacity, and the type, distribution, and severity of the patient’s underlying condition(s). Such preventive mobilization or exercise must be prescribed in such a way as to avoid having any deleterious effects on the patient’s overall condition. Even after highly invasive investigative procedures such as heart catheterization, patients can benefit from safe early ambulation.30 Although much is known about the protective benefits of cardiovascular and pulmonary fitness and conditioning and about the negative effects of bed rest and restricted mobility (discussed later in this section), little has been documented about prescribing exercise to counter orthostatic intolerance in a given patient.31 The characteristics of deconditioning or detraining in a given individual are determined by age, sex, conditioning status before bed rest, underlying pathophysiology, fluid and electrolyte balance, medications, and the duration of bed rest.32 The preventive effects of an exercise stimulus can be defined as that exercise dose that will maintain the patient’s conditioning level and prevent deterioration. At present, the prescription of preventive mobilization and exercise is nonspecific. Aerobic exercise and resistance muscle training have differential effects in countering the effects of restricted mobility.33,34 Although the upright position is the primary means of countering orthostatic changes associated with recumbency, exercise may have a limited role.35 Even though high-intensity, short-duration, isotonic cycle ergometry training (ITE) and intermittent resistive isokinetic training (IKE) have no effect on orthostatic intolerance associated with recumbency in healthy people, ITE maintains plasma volume, red blood cells, and positive fluid balance, and IKE has no effect on plasma loss but mitigates red blood cell loss. These differential training effects are of considerable clinical interest; however, they are the result of high-intensity training, and further recumbent exercise should not be considered a substitute for the gravitational stress associated with the upright position. Although patients who are severely ill are not usually capable of performing intense exercise, it is important to note that the responses to upright exercise by healthy people after 5 days of bed rest can be maintained with a daily 30-minute session of intense interval upright exercise training.36 Further, moderately intense exercise performed against lower body negative pressure to simulate an upright 1-g environment fails to counter orthostatic intolerance after 15 days of bed rest.37 Also, aerobic pedaling exercise in the supine position during bed rest may be inadequate to maintain hemodynamic function and Resistance training fails to counter the cardiovascular deconditioning associated with bed rest.40 Some evidence suggests that isometric exercise during bed rest can attenuate the decrement in Cardiorespiratory conditioning or fitness is related to the volume of regular physical activity; however, its relationship to health measures is less strong.42 Physical inactivity has been causally implicated in lifestyle-related conditions (Chapter 1), but in general, it is not known whether a precise dose of activity or exercise exists that can provide protection against these conditions. One exception to this occurs with ischemic heart disease, in which a threshold intensity of 6 metabolic equivalents (METs) in conjunction with a minimal volume of regular physical activity is recommended for optimal cardiovascular health.43 The precise dose for prevention of hypertension and stroke is less clear.44 Moderate as opposed to heavy exercise has been recommended.43 The choice of relative or absolute intensity of effort depends on the desired preventive outcomes, as well as the patient’s specific characteristics and history. Although a person may exercise an hour a day, the question arises about the remaining 23 hours. Over the past decade, investigators have focused on the health consequences not only of physical inactivity but of prolonged periods of sedentary behavior as well. Research has shown that in addition to regular physical exercise, breaks during periods of sedentary activity (including screen-based activities) are essential to offset the effects of chronic inactivity.45,46 With the advent of screen-based entertainment, children today are at serious risk for the consequences of hours of sedentary activity; furthermore, sedentary children are more likely to become sedentary adults. Conversely, children who are active and move frequently are more likely to do so as adolescents and adults.47 Chronic inactivity increases the risk for chronic lifestyle-related conditions and promotes premature aging. Alternatively, a physically active lifestyle promotes health and well-being, even offsetting lifestyle-related chronic conditions, as people age.48 Humans are designed to be upright and moving; indeed “upright and moving” can be described as the normal physiological position. The deconditioning associated with restricted activity in patients is comparable to detraining in athletes,32,39 yet is distinct from bed rest deconditioning, which is associated with recumbency as well as restricted mobility. When people are recumbent and inactive, gravitational stress (the vertical gravitational gradient) and exercise stress are removed. Bed rest, which requires patients to remain in this recumbent and inactive state, is one of the most commonly used yet seldom questioned therapeutic practices. Despite its widespread acceptance, the body positions it promotes are nonphysiological (Chapter 20). The harmful sequelae of this posture have been well documented;24,39,49–56 yet the more severely ill the patient is, the more confined that individual is to the bed—thereby the greater the risk for multisystem complications (Table 18-2). Table 18-2 Physiological Consequences of Bed Rest Adapted from Woods SL: Cardiac nursing, ed 5, Philadelphia, 2010, JB Lippincott, Williams & Wilkins. The classic study by Saltin and colleagues (1968)57 demonstrated marked multisystem deterioration within 3 weeks of bed rest in five healthy young men and the restoration of aerobic capacity with strenuous training afterwards. In a follow-up of the same subjects 30 years later,58 all were found to have an age-related decrement in aerobic power. When their exercise responses were compared over that time frame, it was revealed that bed rest had had a more profound impact on physical work capacity than 30 years of aging. Of clinical importance is the fact that deterioration of cardiovascular and pulmonary function occurs at a faster rate than musculoskeletal deterioration and that the rate of recovery from the negative effects of bed rest is generally slower than the rate of impairment.59,60 These effects of bed rest are accentuated in older adults61 and are likely to further compound the oxygen transport and other deficits of patients with pathology. Oxidative stress has been implicated in age-related physiological changes.62 Disuse deconditioning has been implicated as an oxidative stressor contributing to aging, especially when combined with the effects of smoking and a Western-type diet (see Chapter 1). In fact, half of the physical decline associated with aging has been attributed to lack of physical activity.63 With regular physical activity and prescribed aerobic and strengthening programs, these changes can be substantially offset. As a result, functional capacity is maximized and, in the event of illness, the individual has better physiological reserve to deal with the pathophysiological insult. Regardless of age, however, exercise-induced physiological and health advantages are lost following cessation of exercise.64 Restricted mobility in older adults has been also associated with clinical depression.65 Thus the evidence supports the need for sustained physical activity and exercise throughout life to derive their functional and health benefits. The recumbent, immobile positions associated with bed rest adversely affect most organ systems by means of an apparent down-regulation of the oxygen transport system.66 This is clinically important because in conventional patient management, there is a direct relationship between how sick the patient is and the amount of time she or he is confined to bed. In addition, the musculoskeletal, neurological, gastrointestinal, and genitourinary systems are adversely affected. A primary effect of mobilization and exercise on the cardiovascular and pulmonary systems is enhanced mucociliary transport and airway clearance.12 Frequent changes in body position augment airway clearance and minimize the pooling and stagnation of bronchial secretions, hence reducing airway obstruction and airflow resistance (Chapter 20). The benefits of frequent body position changes to prevent the accumulation of secretions or resolve them can be augmented when combined with mobilization. The cardiovascular deconditioning resulting from bed rest includes the loss of fluid-volume and pressure regulating mechanisms, the loss of plasma volume, and diuresis.67–70 In turn, the hematocrit is increased, and the risk for developing deep vein thromboses and thromboemboli is increased. This is exacerbated by increases in blood viscosity, platelet count, platelet stickiness, plasma fibrinogen,71 and stasis of venous blood flow. Venous thromboembolic disease is preventable with conservative management, including prophylactic anticoagulation in some instances.72 In addition to restricted mobility, other risk factors include being older, undergoing venous catheterization, and hormone replacement therapy. Conditions that are associated with risk include previous thromboembolus, myocardial infarction, heart failure, severe lung disease, cancer, obesity, and paralytic conditions such as stroke. After acute stroke, patients are particularly at risk due to paresis, recumbency, restricted mobility, and circulatory stasis.73 The work of the heart is increased in a patient who is immobile and recumbent, as is the work of breathing. The work of the heart is greater as a result of the increased filling pressures and heart rate associated with chronic recumbency and the increased blood viscosity. The work of breathing is increased because of reduced lung volumes secondary to visceral encroachment on the underside of the diaphragm, increased intrathoracic blood volume, and restricted chest wall motion. Pulmonary sequelae of recumbency include reduced lung volumes and capacities, particularly functional residual capacity (FRC), residual volumes (RV), and forced expiratory volumes.74–78 A reduction in FRC in the supine position compared with the sitting position has been attributed to both a decrease in thoracic volume and an increase in thoracic blood volume, thereby increasing pulmonary venous engorgement.79 Thus alveolar-arterial oxygen difference and arterial oxygen tension are reduced during bed rest.80–82 Closing volumes are increased, precipitating arterial desaturation in recumbent positions and subsequent complications. With bed rest, the blood vessels of the muscles and splanchnic circulation dilate. With prolonged bed rest, they may lose their ability to constrict. The ability of these vessels to constrict is essential for preventing the pooling of blood and maintaining circulating blood volume when the patient assumes the upright position. Following bed rest, a patient may feel lightheaded or dizzy and may faint. Individual differences in terms of orthostatic intolerance have been reported and need to be assessed.67,68,83,84 Individuals with greater venous compliance in the legs recruit mechanisms to compensate, such as activation of the renin-angiotensin-aldosterone system, activation of the sympathetic nervous system, and inhibition of the parasympathetic nervous system, so they tolerate orthostatic challenges better. With only a few days of bed rest, muscle atrophy is initiated, leading to weakness, discoordination, and balance difficulty.57,85 With severe weakness, excessive strain may be placed on ligaments and joints. Muscles and their inert structures are differentially affected. In the knee extensors, for example, tendon stiffness is reduced and their hysteresis characteristics become exaggerated, whereas this does not occur in the plantar flexors.86 Muscle mass and strength may be lost, and muscle and ligament shortening may occur along with joint contractures, skin lesions, and decubitus ulcers.87,88 At the cellular level, disuse atrophy begins within 4 hours of bed rest. Compared with type IIa muscle fibers in vastus lateralis, type I fibers have been reported to be more seriously affected by bed rest, and they respond less favorably to muscle-resistance training.89 Differences in fiber type may explain why muscles in the lower limbs are differentially affected; for example, the plantar flexors are particularly affected.90 Also, sex differences in muscle strength loss with bed rest have been reported.91 Muscle imbalance may result from poor postural alignment. Skeletal muscle protein synthesis is compromised by bed rest, aging, nutritional deficit, uncontrolled diabetes mellitus, and sepsis.92 Disuse osteoporosis results from reduction of the mechanical stress caused by gravity and from lack of active muscle contraction across joints. Prevention is a primary goal because recovery of mineral loss in bone is prolonged and its loss is largely irreversible.93 Bone mass is restored later than muscle mass and function after a period of restricted mobility, which contributes to fracture risk.94 The limited positioning alternatives in bed may contribute to poor postural alignment, stiffness, and soreness. Bed rest allocates weight bearing to various body parts not adapted for weight bearing. Skin breakdown most commonly occurs over bony prominences, such as the sacrum, trochanters, elbows, scapulae, and heels. Risk factors for pressure ulcers include age, prolonged hospitalization, restricted mobility and general debility, low body weight, low diastolic BP, and surgical intervention.95 Immobile patients are at risk for bone demineralization. An issue of particular importance in older populations, patients with disabilities, postmenopausal women, and patients on steroids is calcium loss. Prevention of disuse osteoporosis is the primary aim because remineralization of bone, even with aggressive exercise, body positioning, electrical stimulation, and possible pharmaceutical agents, is unlikely.93 In patients who are critically ill, cytokines have been implicated in inactivity-related inflammation and muscle injury and atrophy. Activity has been proposed as a countermeasure.96 Bed rest–induced diuresis increases renal load. Patients with renal insufficiency are particularly seriously affected by this effect, as well as by other sequelae of bed rest.97 As a result, they may exhibit dysrhythmias, muscle wasting, weakness, neuropathy, glucose intolerance, and reduced bone density. With bed rest and recumbency, orthostatic intolerance in combination with resting tachycardia and reduced exercise capacity occur, reflecting diminished reflex activity of the sympathetic nervous system. Baroreceptor-mediated activity is blunted and appears to involve abnormal processing in the central nervous system at the level of the ventrolateral medulla.98 CNS changes include slowed electrical activity of the brain, emotional and behavioral changes, slowed reaction times, sleep disturbances, and impaired psychomotor performance.88,99
Mobilization and Exercise
Physiological Basis for Assessment, Evaluation, and Training
Terminology in Mobilization and Exercise
Mobilization
Training
Basic Principles of Mobilization and Exercise
Exercise as an Assessment and Evaluation Tool
 by conducting a
by conducting a  test, which can be done directly or indirectly. Direct measurement of
test, which can be done directly or indirectly. Direct measurement of  requires metabolic measurement with a cart and capacity for expired gas analysis for O2 and CO2 (Figure 18-1). Such carts require pretest gas calibration in addition to calibration of the exercise modality (treadmill or ergometer). The patient needs to be familiarized and habituated to the tester(s) and testing situation, and practice beforehand, to ensure the results are valid. Indirect assessment of
requires metabolic measurement with a cart and capacity for expired gas analysis for O2 and CO2 (Figure 18-1). Such carts require pretest gas calibration in addition to calibration of the exercise modality (treadmill or ergometer). The patient needs to be familiarized and habituated to the tester(s) and testing situation, and practice beforehand, to ensure the results are valid. Indirect assessment of  is imprecise but can provide an index of general conditioning if methods are tightly standardized; this is particularly important when test results are used as outcome measures. Practices related to exercise testing and training prescription are detailed in Chapter 19.
is imprecise but can provide an index of general conditioning if methods are tightly standardized; this is particularly important when test results are used as outcome measures. Practices related to exercise testing and training prescription are detailed in Chapter 19.
Oxygen Transport and Metabolic Demand of Patients
Type of Factors
Specific Factors
Pathophysiological Factors
Intervention-Related Factors
Psychosocial Factors
Miscellaneous
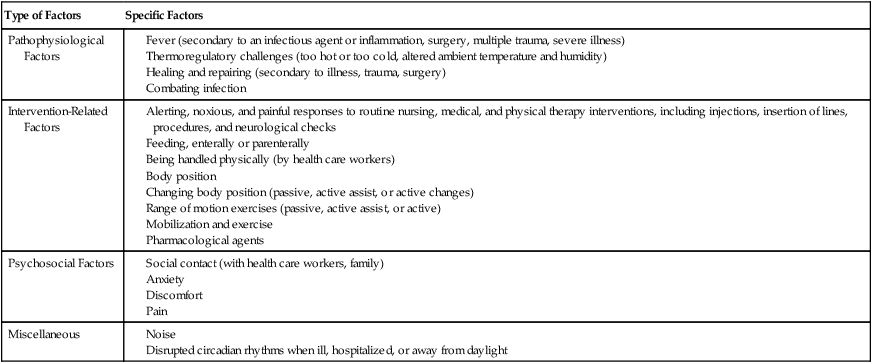
 and overall metabolic demand;1,2 therefore the capacity of the oxygen transport system to meet the patient’s metabolic demands needs to be established in the assessment. These interventions include:
and overall metabolic demand;1,2 therefore the capacity of the oxygen transport system to meet the patient’s metabolic demands needs to be established in the assessment. These interventions include:
 are determined by many factors. In patients, the effect of arousal, anxiety, pain, and noxious stimulation, in addition to the hypermetabolic demands of recovery, contribute to energy cost and demand on the oxygen transport system. Thus relaxing and calming patients are central components of physical therapy because these interventions reduce oxygen demand, as do physical therapy interventions for pain management. Although relaxation, often coupled with sedation or analgesia, is central to physical therapy management in other settings, relaxation procedures should be applied in the management of patients with cardiovascular and pulmonary dysfunction in situations in which agitation, anxiety, and pain contribute to increased oxygen demand. This is especially true in intensive care, where oxygen transport is compromised or threatened in most patients (see Chapters 34 and 35).
are determined by many factors. In patients, the effect of arousal, anxiety, pain, and noxious stimulation, in addition to the hypermetabolic demands of recovery, contribute to energy cost and demand on the oxygen transport system. Thus relaxing and calming patients are central components of physical therapy because these interventions reduce oxygen demand, as do physical therapy interventions for pain management. Although relaxation, often coupled with sedation or analgesia, is central to physical therapy management in other settings, relaxation procedures should be applied in the management of patients with cardiovascular and pulmonary dysfunction in situations in which agitation, anxiety, and pain contribute to increased oxygen demand. This is especially true in intensive care, where oxygen transport is compromised or threatened in most patients (see Chapters 34 and 35).
 . This type of training, however, also requires an adequate central response of the cardiovascular and/or respiratory systems to produce a high level of cardiac output during exercise. In patients with compromised cardiovascular or respiratory function, this type of exercise is extremely difficult and can often lead to undue fatigue. The stimulus for increasing metabolic demand with exercise can be achieved in ways that can help minimize
. This type of training, however, also requires an adequate central response of the cardiovascular and/or respiratory systems to produce a high level of cardiac output during exercise. In patients with compromised cardiovascular or respiratory function, this type of exercise is extremely difficult and can often lead to undue fatigue. The stimulus for increasing metabolic demand with exercise can be achieved in ways that can help minimize  , thus reducing the impact of reduced cardiovascular and/or respiratory function.3 For example, in patients with chronic obstructive lung disease, breathing a low-density helium gas mixture relieves some of the respiratory loading, resulting in increases in exercise tolerance4 and peripheral muscle trainability.5 Use of such breathing gases is not usually practical in clinical settings, however. Other methods such as single limb training and high-intensity interval training, have been shown to reduce central demand and optimize peripheral load (see Chapter 19).
, thus reducing the impact of reduced cardiovascular and/or respiratory function.3 For example, in patients with chronic obstructive lung disease, breathing a low-density helium gas mixture relieves some of the respiratory loading, resulting in increases in exercise tolerance4 and peripheral muscle trainability.5 Use of such breathing gases is not usually practical in clinical settings, however. Other methods such as single limb training and high-intensity interval training, have been shown to reduce central demand and optimize peripheral load (see Chapter 19).
Cellular Energetics in Response to Acute Mobilization and Exercise
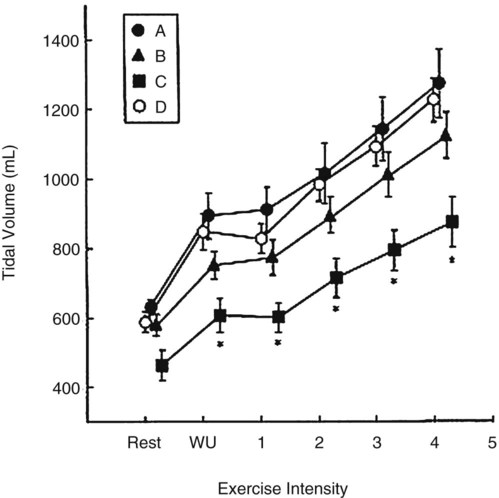
 , and thereafter CO is augmented by increases in HR (Figure 18-2). One exception in health is in elite athletes, whose SV may continue to increase commensurate with exercise intensity.9 To oxygenate a greater volume of blood in the lungs, an increased volume of air must be inspired. To increase
, and thereafter CO is augmented by increases in HR (Figure 18-2). One exception in health is in elite athletes, whose SV may continue to increase commensurate with exercise intensity.9 To oxygenate a greater volume of blood in the lungs, an increased volume of air must be inspired. To increase  , tidal volume (VT) and respiratory rate (RR) increase. At low intensities of exercise, VT increases disproportionately to RR, whereas at moderate to high intensities, VT plateaus and further increases in
, tidal volume (VT) and respiratory rate (RR) increase. At low intensities of exercise, VT increases disproportionately to RR, whereas at moderate to high intensities, VT plateaus and further increases in  are effected by an increase in RR (Figure 18-3).10 Exercise is associated with a small increase in airway diameter and length of pulmonary structures, hence, a reduction in airway resistance. Zone 2, the zone of greatest alveolar ventilation to perfusion (
are effected by an increase in RR (Figure 18-3).10 Exercise is associated with a small increase in airway diameter and length of pulmonary structures, hence, a reduction in airway resistance. Zone 2, the zone of greatest alveolar ventilation to perfusion ( ) matching in the lungs, is increased as a result of pulmonary capillary dilation and recruitment. Diaphragmatic excursion is enhanced, and the distributions of ventilation and perfusion become more uniform throughout the lungs, which minimizes airway closure and atelectasis. Exercise increases diaphragmatic excursion, which leads to inflation of the lungs in three planes (anteroposterior, transverse, and cephalocaudal, particularly in the upright position).
) matching in the lungs, is increased as a result of pulmonary capillary dilation and recruitment. Diaphragmatic excursion is enhanced, and the distributions of ventilation and perfusion become more uniform throughout the lungs, which minimizes airway closure and atelectasis. Exercise increases diaphragmatic excursion, which leads to inflation of the lungs in three planes (anteroposterior, transverse, and cephalocaudal, particularly in the upright position).
 First, this action increases alveolar ventilation (
First, this action increases alveolar ventilation ( ) by a primary increase in VT.
) by a primary increase in VT.
 Second, exercise-induced lung motion facilitates lymphatic flow and drainage. Optimal lymphatic drainage is essential for lung water balance with the increased volume of blood being processed through the pulmonary circulation and lung parenchyma. This action may explain, in part, the beneficial effect of mobilization on the distribution and function of pulmonary immune factors.11 The increased movement of the lungs during exercise has a primary effect on mucociliary transport and mucus clearance.12 Physical activity may also minimize bacterial colonization in the airways, hence reducing the risk for pulmonary infection.13
Second, exercise-induced lung motion facilitates lymphatic flow and drainage. Optimal lymphatic drainage is essential for lung water balance with the increased volume of blood being processed through the pulmonary circulation and lung parenchyma. This action may explain, in part, the beneficial effect of mobilization on the distribution and function of pulmonary immune factors.11 The increased movement of the lungs during exercise has a primary effect on mucociliary transport and mucus clearance.12 Physical activity may also minimize bacterial colonization in the airways, hence reducing the risk for pulmonary infection.13
 Finally, lung movement stimulates surfactant production and its distribution over parenchymal tissue. Surfactant is essential for reducing surface tension in the alveoli, maintaining alveolar stability, and maintaining lung compliance, thereby minimizing airway closure and areas of lung collapse.
Finally, lung movement stimulates surfactant production and its distribution over parenchymal tissue. Surfactant is essential for reducing surface tension in the alveoli, maintaining alveolar stability, and maintaining lung compliance, thereby minimizing airway closure and areas of lung collapse.
Effects of Mobilization and Exercise on Oxygen Transport
The Prescription of Mobilization and Exercise
 and oxygen delivery (DO2) (see Chapter 2);25 this ensures that the patient’s capacity for oxygen transport is not exceeded.
and oxygen delivery (DO2) (see Chapter 2);25 this ensures that the patient’s capacity for oxygen transport is not exceeded.
Preventive Effects of Exercise
Prescription of Prehabilitation Exercise
 .38 With respect to the parameters for prescription of mobilization, the intensity of training appears to be singularly important in attenuating the deconditioning effects associated with bed rest. In terms of importance, intensity is followed by frequency.39
.38 With respect to the parameters for prescription of mobilization, the intensity of training appears to be singularly important in attenuating the deconditioning effects associated with bed rest. In terms of importance, intensity is followed by frequency.39
 and maintain muscle integrity better than isotonic exercise.41 Markers of lactic dehydrogenase, hence anaerobic threshold, increase with both types of exercise. Over time, however, reduced hydrostatic stress contributes to reduced lactic dehydrogenase in both types of training.
and maintain muscle integrity better than isotonic exercise.41 Markers of lactic dehydrogenase, hence anaerobic threshold, increase with both types of exercise. Over time, however, reduced hydrostatic stress contributes to reduced lactic dehydrogenase in both types of training.
 What preventive mobilization/exercise is best for which individuals and under what conditions (i.e., what are the principles of prescription)?
What preventive mobilization/exercise is best for which individuals and under what conditions (i.e., what are the principles of prescription)?
 How do different types of exercise compare with respect to their preventive effects when all else is constant (i.e., patient’s age and demographic profile, smoking history, general health, presenting illness and severity, body weight, nutritional status, aerobic condition, stress levels, cognitive status, and medication schedule)?
How do different types of exercise compare with respect to their preventive effects when all else is constant (i.e., patient’s age and demographic profile, smoking history, general health, presenting illness and severity, body weight, nutritional status, aerobic condition, stress levels, cognitive status, and medication schedule)?
 Does exercising in some body positions elicit better preventive effects than exercise in other body positions?
Does exercising in some body positions elicit better preventive effects than exercise in other body positions?
 What principles establish the mobilization/exercise intensity, duration, and frequency that are optimal for a given individual whose mobility is restricted?
What principles establish the mobilization/exercise intensity, duration, and frequency that are optimal for a given individual whose mobility is restricted?
 What types of exercise are best suited for cross-transfer of their effects between the ipsilateral and contralateral limbs, to limit deconditioning when one limb is immobilized?
What types of exercise are best suited for cross-transfer of their effects between the ipsilateral and contralateral limbs, to limit deconditioning when one limb is immobilized?
 What are the parameters that should guide physical activity during the day to limit prolonged periods of sitting (i.e., maximal duration of periods of inactivity, degree of physical activity needed to offset the deleterious effects of sedentary periods)?
What are the parameters that should guide physical activity during the day to limit prolonged periods of sitting (i.e., maximal duration of periods of inactivity, degree of physical activity needed to offset the deleterious effects of sedentary periods)?
 What constitutes an adequate stimulus to maximize the preventive effects of exercise for a given patient, particularly a patient who is critically ill?
What constitutes an adequate stimulus to maximize the preventive effects of exercise for a given patient, particularly a patient who is critically ill?
Hazards of Sedentary Activity
Physiological Effects of Bed Rest
Bed Rest Consequence
Potential Mechanisms
I.Fluid volume redistribution
II.Muscular inactivity
III.Altered distribution of body weight and pressure
IV.Aerobic deconditioning
V.Other
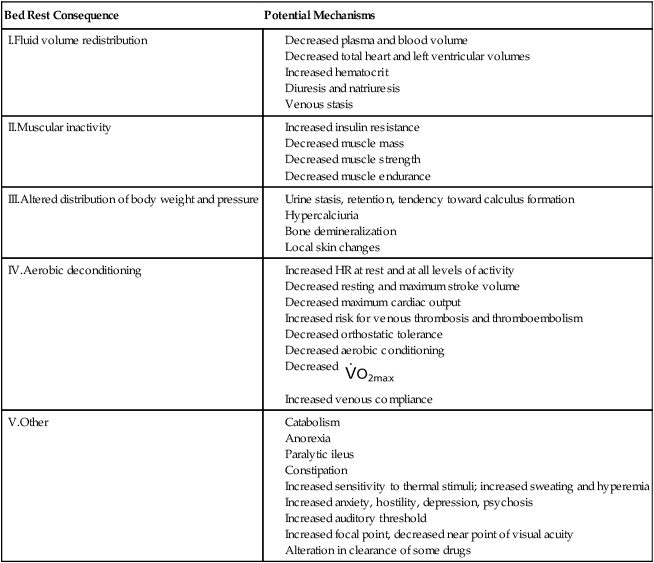
Cardiovascular and Pulmonary Effects
Musculoskeletal Effects
Renal Effects
Central Nervous System Effects
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Mobilization and Exercise: Physiological Basis for Assessment, Evaluation, and Training

 ). Oxygen consumption is dictated by fluctuating metabolic requirements: demand is at its lowest point when the body is rest but increases to intermediate levels during submaximal activity and reaches a peak at the maximal level of exercise an individual can volitionally tolerate. Metabolic cost increases with illness or injury as a result of healing and repair. Two abbreviations frequently appear in the exercise physiology literature to denote oxygen consumption:
). Oxygen consumption is dictated by fluctuating metabolic requirements: demand is at its lowest point when the body is rest but increases to intermediate levels during submaximal activity and reaches a peak at the maximal level of exercise an individual can volitionally tolerate. Metabolic cost increases with illness or injury as a result of healing and repair. Two abbreviations frequently appear in the exercise physiology literature to denote oxygen consumption:  and
and  . Although often used interchangeably, these terms are technically distinct.
. Although often used interchangeably, these terms are technically distinct. Versus
Versus 
 .
. , however, is that most exercise activities, including exercise tests, are selective in their focus and tend to work just the legs or the arms, or work the legs in different ways (i.e., cycling a lower-extremity ergometer versus walking on a treadmill).
, however, is that most exercise activities, including exercise tests, are selective in their focus and tend to work just the legs or the arms, or work the legs in different ways (i.e., cycling a lower-extremity ergometer versus walking on a treadmill).  , then, measures oxygen consumption in the context of the exercise: where
, then, measures oxygen consumption in the context of the exercise: where  is then a theoretical value,
is then a theoretical value,  is a practical one.
is a practical one. than maximal effort resulting from arm work; further, maximal effort resulting from treadmill walking or running generates a greater
than maximal effort resulting from arm work; further, maximal effort resulting from treadmill walking or running generates a greater  than maximal leg work on a cycle ergometer (about 10% more). This greater
than maximal leg work on a cycle ergometer (about 10% more). This greater  may be explained by the larger muscle mass of the legs than the arms in the first situation, and the arm work and requirement for increased postural stabilization in the second situation. The more a patient’s muscle groups work simultaneously, the closer
may be explained by the larger muscle mass of the legs than the arms in the first situation, and the arm work and requirement for increased postural stabilization in the second situation. The more a patient’s muscle groups work simultaneously, the closer  approximates true
approximates true  .
. can be achieved is an academic question. Maximal effort exerted during Nordic (cross-country) skiing approximates theoretical
can be achieved is an academic question. Maximal effort exerted during Nordic (cross-country) skiing approximates theoretical  most closely in that the activity requires strenuous arm and leg work coupled with marked postural stabilization. In the laboratory,
most closely in that the activity requires strenuous arm and leg work coupled with marked postural stabilization. In the laboratory,  is obtained based on a maximal exercise test in which metabolic evaluation is performed. Such evaluation indicates when the individual’s maximal level of physiological capacity is reached, including the attainment of age-predicted maximal heart rate. The evaluation may also include a plateau of or decrement in
is obtained based on a maximal exercise test in which metabolic evaluation is performed. Such evaluation indicates when the individual’s maximal level of physiological capacity is reached, including the attainment of age-predicted maximal heart rate. The evaluation may also include a plateau of or decrement in  with increasing work rate.
with increasing work rate. , when describing the
, when describing the  achieved by an individual when performing a maximal effort during a specified exercise testing condition.
achieved by an individual when performing a maximal effort during a specified exercise testing condition. represents the maximal rate of aerobic glycolysis (or maximal aerobic power). Though aerobic capacity is often used to describe
represents the maximal rate of aerobic glycolysis (or maximal aerobic power). Though aerobic capacity is often used to describe  , aerobic capacity actually refers to the total amount of energy produced aerobically and better reflects aerobic endurance than
, aerobic capacity actually refers to the total amount of energy produced aerobically and better reflects aerobic endurance than  . The term maximal aerobic power is more appropriate to describe
. The term maximal aerobic power is more appropriate to describe  .
. , and
, and  , as well as subjective responses of exertion and fatigue, are all aspects of this study. An understanding of these responses has enabled physical therapists to use exercise as a tool in the assessment, evaluation, and training of patients.
, as well as subjective responses of exertion and fatigue, are all aspects of this study. An understanding of these responses has enabled physical therapists to use exercise as a tool in the assessment, evaluation, and training of patients.











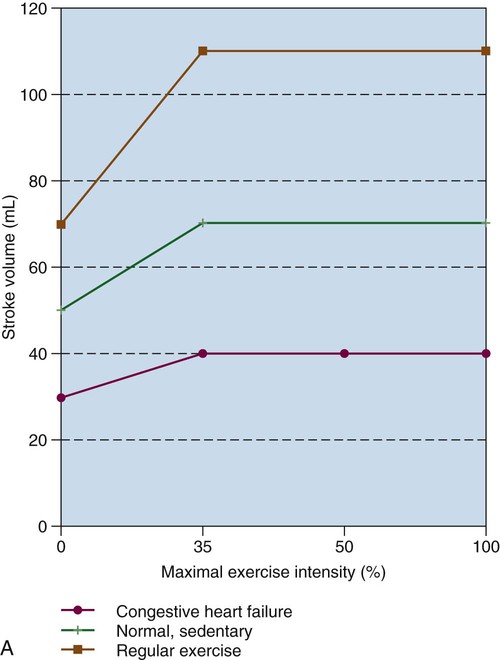
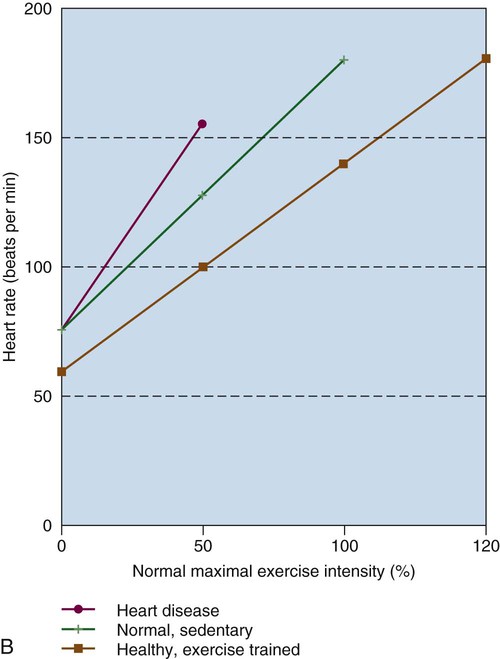
 ) corresponding to exercise intensity; left vertical axis is stroke volume (dashed lines); right vertical axis represents heart rate (solid lines). Light lines, Before aerobic training; dark lines, after aerobic training.
) corresponding to exercise intensity; left vertical axis is stroke volume (dashed lines); right vertical axis represents heart rate (solid lines). Light lines, Before aerobic training; dark lines, after aerobic training.