Miscellaneous Thymomas
Borislav A. Alexiev, M.D.
Anja C. Roden, M.D.
Fabio R. Tavora, M.D., Ph.D.
Metaplastic Thymoma (Biphasic Thymoma, Thymoma with Pseudosarcomatous Stroma)
Terminology
Incidence and Clinical
Metaplastic thymoma is a rare tumor that occurs in adult patients of both genders. The age at manifestation ranges from 28 to 71 years (mean, 50.9 years), and the tumor tends to prevail in men.4,6
The tumors manifest by local symptoms or can be asymptomatic and are found incidentally upon x-ray, CT, or MRI examination. The majority of patients have no myasthenia gravis or other paraneoplastic syndromes.5 A recent report describes symptoms of myasthenia gravis with positive serum titer for antiacetylcholine receptor antibody in a patient with metaplastic thymoma.1
Gross Pathology
Microscopic Pathology
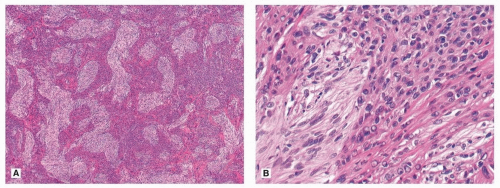
Microscopically, metaplastic thymoma is characterized by a biphasic pattern composed of epithelial components and spindle cells, sometimes with a narrow rim of residual thymic tissue incorporated in its peripheral portion (Fig. 105.1).1,2,3,4,5,6 Occasional cases can show invasion of the surrounding tissues. In contrast to conventional
thymomas, metaplastic thymoma does not show a lobulated growth pattern. The epithelial areas consist of anastomosing cords and islands or broad trabeculae of cohesive neoplastic cells. Focal epithelial areas may exhibit whorled squamoid configuration or abortive formation of Hassall corpuscles. The epithelial cells are polygonal, ovoid, or round, with oval nuclei and fairly abundant eosinophilic cytoplasm. Some epithelial cells show the presence of prominent nuclear grooves or nuclear pseudoinclusions. In some areas, the epithelial cells display overt cytologic atypia with large vesicular nuclei, large hyperchromatic nuclei, and multinucleation. Despite the nuclear atypia, mitotic figures are rare. The spindle cell components demonstrate a short fascicular or storiform growth pattern. They are always bland appearing and often mitotically inactive, with fine nuclear chromatin and slender bipolar cell processes. The spindle cell components may show sharp delineation or gradual merging with the epithelial islands. While both the epithelial and spindle cell components are readily recognizable in most cases, some cases show marked predominance of one component to the exclusion of the other in some or most areas. A diagnosis of such cases can be difficult without extensive sampling to identify the typical biphasic pattern. Lymphocytes are usually sparse, but some cases can exhibit a light infiltrate of small lymphocytes and plasma cells. There can be scattered foci of stromal calcification.
thymomas, metaplastic thymoma does not show a lobulated growth pattern. The epithelial areas consist of anastomosing cords and islands or broad trabeculae of cohesive neoplastic cells. Focal epithelial areas may exhibit whorled squamoid configuration or abortive formation of Hassall corpuscles. The epithelial cells are polygonal, ovoid, or round, with oval nuclei and fairly abundant eosinophilic cytoplasm. Some epithelial cells show the presence of prominent nuclear grooves or nuclear pseudoinclusions. In some areas, the epithelial cells display overt cytologic atypia with large vesicular nuclei, large hyperchromatic nuclei, and multinucleation. Despite the nuclear atypia, mitotic figures are rare. The spindle cell components demonstrate a short fascicular or storiform growth pattern. They are always bland appearing and often mitotically inactive, with fine nuclear chromatin and slender bipolar cell processes. The spindle cell components may show sharp delineation or gradual merging with the epithelial islands. While both the epithelial and spindle cell components are readily recognizable in most cases, some cases show marked predominance of one component to the exclusion of the other in some or most areas. A diagnosis of such cases can be difficult without extensive sampling to identify the typical biphasic pattern. Lymphocytes are usually sparse, but some cases can exhibit a light infiltrate of small lymphocytes and plasma cells. There can be scattered foci of stromal calcification.
Special Studies
Immunohistochemically, the epithelial cells show strong staining for cytokeratin and p63 and variable staining for Epithelial membrane antigen (EMA), and they do not show cell membrane staining for CD5.1,2,4,5,6 The spindle cells lack expression of cytokeratin and E-cadherin but show expression of mesenchymal markers (vimentin).2 CD20 is negative in tumor cells. Proliferative fraction (Ki-67 index) is low (<5%). The T lymphocytes within the tumor proper usually exhibit a mature immunophenotype.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree