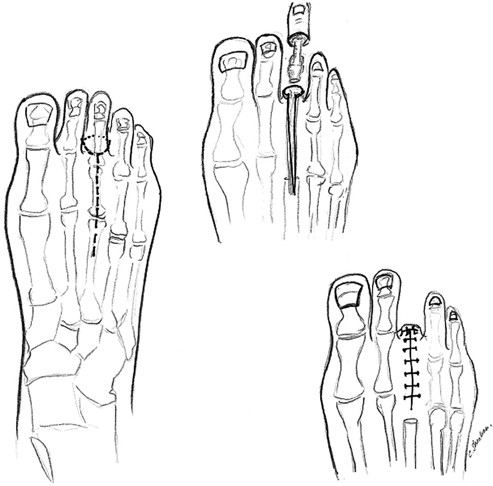
Malachi G. Sheahan, Claudie M. Sheahan and Frank B. Pomposelli The foot and leg are prepped and draped to the knee using sterile technique. The incision is made at the level of the mid-proximal phalanx down to the level of the bone. The incision should be circumferential rather than fish-mouth when possible to avoid compromising blood supply to the flap. Trimming the phalynx back to allow tension-free closure is an important principle. In the case of the first toe, the approach may be altered to include a plantar flap if possible (Figure 1). The foot and leg are prepped to the thigh and draped using sterile technique. A racquet-type longitudinal incision is made on the dorsum of the foot parallel to the metatarsal bone extending on each side of the toe as a semielliptical incision converging on the plantar surface of the foot (Figure 2). A circular incision should be avoided if primary closure is to be attempted, because there is less tension in the closure of an elliptical incision and therefore greater chance of wound healing. A ratio of incision length to width of at least 3:1 will aid primary closure. If ulceration is present on the plantar surface at the level of the metatarsal head, this may be included in the excision as well. Preoperative assurance of adequate circulation is critical to the healing of this amputation type.
Minor Amputations
Surgical Technique
Transphalangeal Toe Amputation
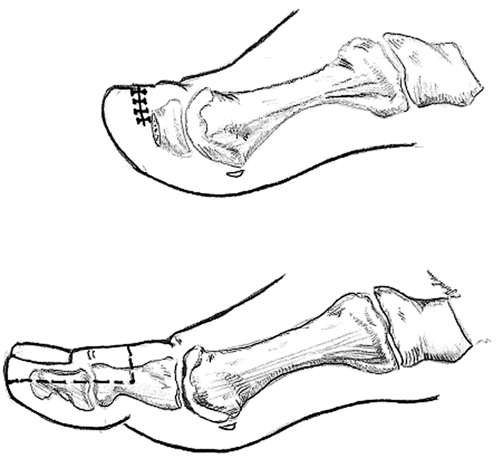
Transmetatarsal (Ray) Toe Amputation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Minor Amputations