Middle Compartment Mass
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Lymphadenopathy
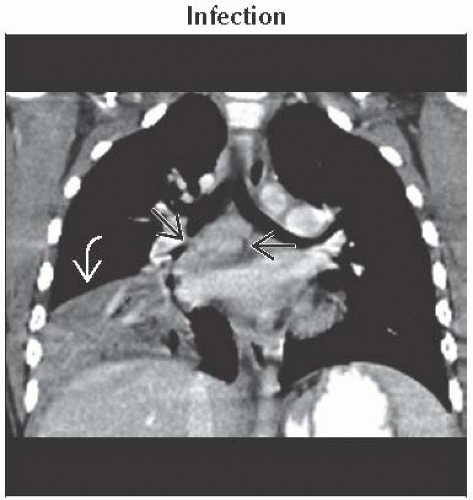
Infection
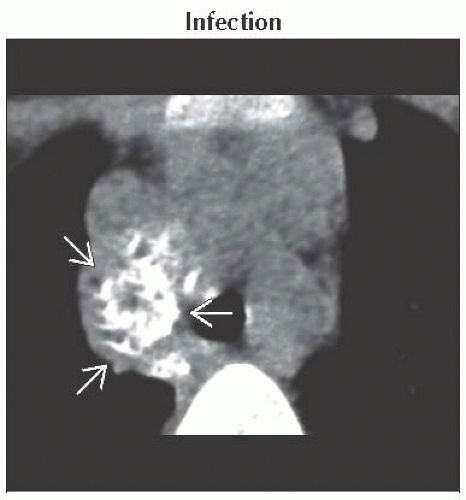
Sarcoidosis
Lymphoma
Lung Carcinoma and Extrathoracic Metastases
Foregut Duplication Cysts
Hiatal Hernia
Less Common
Aortic Aneurysm
Lipomatosis
Mediastinal Goiter
Rare but Important
Esophageal Masses
Mediastinitis
Mediastinal Hemorrhage
Tracheal Neoplasms
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Anatomic boundaries of middle mediastinum on lateral radiograph
Anterior boundary
Line drawn along anterior tracheal wall and posterior heart border
Posterior boundary
Line drawn 1 cm behind anterior margin of vertebral bodies
Contents include trachea, superior vena cava, mid aortic arch, lymph nodes, and esophagus
Middle mediastinal mass deviates these normal radiographic lines and measurements
Right paratracheal stripe ≤ 4 mm
Concave interface in aortopulmonary window
Reverse S contour of azygoesophageal recess
Posterior tracheal stripe ≤ 6 mm on lateral radiograph
Components to consider in differential diagnosis
Density of lesion (fat, calcium, soft tissue, fluid)
Number of lesions
Clinical history
Helpful Clues for Common Diagnoses
Lymphadenopathy
Right paratracheal stripe thickening usually indicates lymphadenopathy
Subcarinal lymphadenopathy
Convexity in superior azygoesophageal recess
Calcified nodes
Dense calcification usually from prior granulomatous infection
Rim calcification, “eggshell” appearance with sarcoidosis, silicosis, and treated lymphoma
Necrotic or low-density nodes
Tuberculosis and histoplasmosis
Lymphoma, thymoma, metastases, and lung carcinoma
Enhancing lymphadenopathy
Vascular metastases (renal, thyroid, and melanoma)
Tuberculosis
Castleman disease
Foregut Duplication Cysts
Round and well circumscribed
Highly variable Hounsfield units depending on fluid content
Bronchogenic cysts commonly subcarinal in location
Less commonly peripheral, hilar
Esophageal duplication cyst location
Paraesophageal or within esophageal wall
Hiatal Hernia
Convexity of lower azygoesophageal recess
Easily diagnosed on CT by protrusion of stomach through esophageal hiatus
Helpful Clues for Less Common Diagnoses
Aortic Aneurysm
Definitions
Dilated ≥ 4 cm
Aneurysmal ≥ 5 cm
High risk of rupture ≥ 6 cm
Saccular are focal outpouchings and are associated with trauma or infection
Fusiform is circumferential
Annuloaortic ectasia is a dilated aortic root and associated with Marfan syndrome
CT or MR are diagnostic
Lipomatosis
Causes include
Obesity, long-term steroid therapy, Cushing disease
Radiographs show smooth mediastinal widening without compression of trachea
CT shows homogeneous fat causing bulging of mediastinal contours
Mediastinal Goiter
Radiographs reveal upper mediastinal mass with deviation of trachea
CT demonstrates connection to thyroid
Coronal images very helpful
Enhance avidly with contrast and are high in density on pre-contrast exams
Helpful Clues for Rare Diagnoses
Esophageal Masses
Varices are secondary to portal hypertension
Abnormal convexity of lower azygoesophageal recess or paravertebral widening
CT with contrast is diagnostic and easily differentiates from hiatal hernia or tumor
Mediastinitis
Associated with sternotomy, esophageal perforation, or spread of infection
Radiographs show widened mediastinum
CT findings include
Diffuse fat stranding replacing normal mediastinal fat
Pneumomediastinum
Fluid collections
Difficult to differentiate normal postoperative appearance from mediastinitis
Resolution of expected fluid collections occurs within 2-3 weeks after surgery
Mediastinal Hemorrhage
Causes include
Acute aortic injury or venous bleeding secondary to severe blunt or penetrating trauma
Aneurysm or dissection rupture
Radiographs show nonspecific mediastinal widening
High-attenuation (blood density) fluid within mediastinum
Hematoma not adjacent to aorta is secondary to venous bleeding
Retrosternal hematoma in anterior compartment
Tracheal Neoplasms
Usually secondary to primary squamous cell carcinoma or adenoid cystic carcinoma
Uncommonly single or multiple metastases from
Melanoma, breast carcinoma, colon carcinoma, or adjacent tumor extension
CT features include
Polypoid, sessile, or circumferential lesion
Adenoid cystic carcinoma usually originates from posterolateral wall
Important to define extraluminal extent of disease for surgical planning
Image Gallery
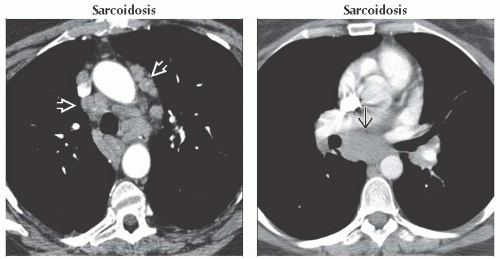 (Left) Axial CECT shows features of adenopathy in sarcoidosis. There is diffuse mediastinal adenopathy
 in the prevascular and paratracheal spaces. Lower sections revealed bilateral symmetric hilar lymphadenopathy. (Right) Axial CECT shows subcarinal lymphadenopathy in the prevascular and paratracheal spaces. Lower sections revealed bilateral symmetric hilar lymphadenopathy. (Right) Axial CECT shows subcarinal lymphadenopathy  in this asymptomatic patient. The symmetry of lymphadenopathy and age of the patient are important differential considerations to make the correct diagnosis. in this asymptomatic patient. The symmetry of lymphadenopathy and age of the patient are important differential considerations to make the correct diagnosis.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|