Apixaban is a novel oral anticoagulant which is approved for the management of atrial fibrillation and venous thromboembolism prophylaxis. There have been concerns regarding bleeding risks with apixaban in patients with renal impairment. We performed a systematic review and meta-analysis to evaluate the risk of bleeding with apixaban in these patients. Relevant studies were identified through electronic literature searches of MEDLINE, EMBASE, Cochrane library, and clinicaltrials.gov (from inception to February 24, 2014). Phase III randomized controlled trials that compared apixaban with conventional agents (vitamin K antagonist and/or warfarin, low molecular weight heparin, aspirin, and placebo) were included. We defined mild renal impairment as creatinine clearance of 50 to 80 ml/min and moderate to severe renal impairment as creatinine clearance <50 ml/min. Study-specific risk ratios were calculated, and between-study heterogeneity was assessed using the I 2 statistics. In 6 trials involving 40,145 patients, the risk of bleeding with apixaban in patients with mild renal impairment was significantly less (risk ratio 0.80, 95% confidence interval 0.66 to 0.96, I 2 = 13%) compared with conventional anticoagulants. In patients with moderate to severe renal impairment, the risk of bleeding with was found to be similar (risk ratio 1.01, 95% confidence interval 0.49 to 2.10, I 2 = 72%). In conclusion, compared with the conventional agents, bleeding risk with apixaban in patients with mild and moderate to severe renal insufficiency is lower and similar, respectively.
Apixaban, an oral direct factor Xa inhibitor, is one of the newer oral anticoagulants that have been recently approved for the prevention and treatment of venous thromboembolism (VTE) as well as for the prevention of stroke and systemic thromboembolism in atrial fibrillation (AF). It has been proven to be of similar or superior efficacy compared with the conventional anticoagulants in large randomized controlled trials (RCTs). It is gaining increasing popularity over vitamin K antagonists (VKAs) owing to its rapid onset of action, shorter half-life, absence of food interactions, and the lack of need for regular laboratory monitoring. Although only 25% to 30% of apixaban is renally eliminated, there is still a potential for increased risk of bleeding events in patients with worsening renal impairment due to accumulating blood levels. The currently used doses of apixaban in patients with AF with varying degrees of renal impairment are derived from the trials which essentially excluded patients with severe chronic kidney disease (CKD). Increasing use of apixaban coupled with lack of specific antidote raises concern for severe bleeding events, especially, in high-risk groups such as patients with CKD. Because it is still early for “real world data” on this topic, we sought to perform a systematic review and meta-analysis to explore whether apixaban is superior to conventional agents with regard to bleeding complications in the subset of patients with renal impairment from the available trial data.
Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses framework guidelines. RCTs assessing the use of apixaban versus placebo or standard of care for the prophylaxis or treatment of VTE or for prophylaxis of stroke and thromboembolism in AF were included in our systematic review. Protocol for this meta-analysis was prospectively devised that details the background, objectives and eligibility criteria of studies, outcomes, and statistical methods. This is available for review on request to investigators.
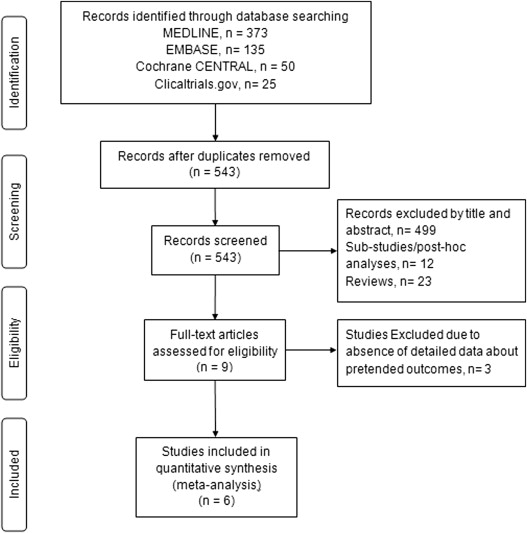
Preferred Reporting Items for Systematic Reviews and Meta-analyses statement for reporting systematic reviews recommended by the Cochrane Collaboration was followed for conducting this meta-analysis ( Figure 1 ). Systematized search of MEDLINE (through PubMed), EMBASE, Cochrane library, and clinicaltrials.gov (inception to February 24, 2014) was carried out to identify eligible RCTs. PubMed, EMBASE, clinicaltrials.gov , and Cochrane Library databases were searched using 4 broad search themes: “Apixaban,” “Venous Thrombosis,” “Pulmonary Embolism,” and “Atrial Fibrillation.” These were combined using Boolean operator “AND.” No language restriction was used. Bibliographies belonging to included papers, known reviews, and relevant articles were looked into for additional trials. To minimize data duplication as a result of multiple reporting, we compared papers from the same author. Two authors (RP and PK) screened and retrieved reports and excluded irrelevant studies. Relevant data were extracted by 2 authors (RP and PK) and checked by another (MRA). Additional investigators (AP, SG, and DRP) participated in the review process when uncertainty about eligibility criteria arose.
Phase III RCTs comparing apixaban against any control group (placebo, no-treatment or standard of care, nonpharmacological interventions, or any drug) for AF or VTE. Only phase III RCTs were included to avoid bias in risk estimation because of statistical effects of rare events and the impact of small studies on meta-analysis results. All RCTs which reported data on the degree of renal impairment were considered for inclusion irrespective of patients’ underlying conditions, co-morbidities, background therapy, dose of apixaban, or duration of follow-up.
Data from the studies were compared and interpreted using RevMan version 5.3 (Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark, 2014). Summary risk ratio and 95% confidence interval were estimated using Mantel-Haenszel random-effect method to account for heterogeneity. Percentage of heterogeneity was calculated using I 2 statistics. I 2 <30% was considered as low, 30% to 60% as moderate, and >60% as high heterogeneity. A p value of 0.05 was used as the level of significance.
The overall risk of bias among the included studies was low ( Supplementary Figure 1 ). All the studies described generation of the randomization sequence and details about allocation concealment. All of them reported blinding of participants and investigators. Safety events were monitored and recorded for all included studies, and definitions were provided a priori. Withdrawal rates for all studies were <20%. All the studies were industry sponsored (Bristol Myers Squibb and Pfizer).
Visual inspection of the funnel plots showed that all included studies were large trials with both positive as well as negative results for the outcome of interest ( Supplementary Figure 2 ).
Results
A total of 583 citations met the initial search criteria. After exclusion of 40 duplicate entries, 543 citations were evaluated, of which 9 were reviewed in detail. We excluded 3 RCTs as they did not meet eligibility criteria or did not have detailed data about renal impairment and bleeding events. Six eligible RCTs were identified and included in this review ( Figure 1 ).
Table 1 summarizes the characteristics of the included studies and participants. Of the 6 included studies, 2 compared apixaban with enoxaparin, each of the remaining studies compared apixaban with aspirin, apixaban with placebo, apixaban with VKAs, and apixaban with enoxaparin followed by VKAs. Four trials studied apixaban for VTE and 2 studied apixaban for AF. The dosing regimen for apixaban varied among the clinical trials. All the trials excluded patients with a history of severe renal impairment (defined by the Cockcroft-Gault equation creatinine clearance [CrCl] <25 ml/min in 3 trials and <30 ml/min in 2 trials ). All studies included frequent safety assessments for bleeding and reported predefined safety outcomes.
| Study | Year | N | Study population | Intervention | Patients in Renal subgroups per CrCl (n) | Exclusion Criteria | Age (y) | F/u (y) |
|---|---|---|---|---|---|---|---|---|
| AMPLIFY | 2013 | 5,395 | Acute VTE | A ∗ vs E, f/b W | CrCl≥81: 3478; 50-80: 1093; ≤50: 338; M: 486 | Cr >221 or CrCl<25 | 57 | 0.5 |
| AMPLIFY-EXT | 2013 | 2,486 | VTE with 6-12 mo AC | A (2.5 or 5mg BID) vs P | CrCl≥81: 1739; 50-80: 536; ≤50: 138; M: 69 | CrCl<25 | 57 | 1 |
| AVERROES | 2011 | 5,599 | AF unsuitable to W | A (5 mg BID) v ASA | CrCl ≥80: 2021; 50-79: 2374; <50: 1198 | Cr>221or CrCl<25 | 70 | 1.1 |
| ARISTOTLE | 2011 | 18,201 | AF | A (5 mg BID) vs W | CrCl≥81: 7518; 50-80: 7587; ≤50: 3017 | Cr >221 or CrCl<25 | 70 | 1.8 |
| ADVANCE-2 | 2010 | 3,057 | TKR | A (2.5 mg) vs E (40 mg) | N/A | CrCl < 30 | 67 | 0.17 |
| ADVANCE-3 | 2010 | 5,407 | TKR | A (2.5 mg) vs E (40 mg) | N/A | CrCl < 30 | 61 | 0.17 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


