Outcomes of percutaneous coronary intervention (PCI) versus medical therapy (MT) in the management of stable ischemic heart disease (SIHD) remain controversial, with some but not all studies showing improved results in patients with ischemia. We sought to elucidate whether PCI improves mortality compared to MT in patients with objective evidence of ischemia (assessed using noninvasive imaging or its invasive equivalent). We performed a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing PCI to MT in patients with SIHD. To maintain a high degree of specificity for ischemia, studies were only included if ischemia was defined on the basis of noninvasive stress imaging or abnormal fractional flow reserve. The primary outcome was all-cause mortality. We identified 3 RCTs (Effects of Percutaneous Coronary Interventions in Silent Ischemia After Myocardial Infarction II, Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2, and a substudy of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation trial) enrolling a total of 1,557 patients followed for an average of 3.0 years. When compared with MT in this population of patients with objective ischemia, PCI was associated with lower mortality (hazard ratio 0.52, 95% confidence interval 0.30 to 0.92, p = 0.02). There was no evidence of study heterogeneity or bias among included trials. In this meta-analysis of published RCTs, PCI was shown to have a mortality benefit over MT in patients with SIHD and objective assessment of ischemia using noninvasive imaging or its invasive equivalent. In conclusion, this study provides insight into the management of a higher-risk SIHD population that is the focus of the ongoing International Study of Comparative Health Effectiveness with Medical and Invasive Approaches trial.
Randomized controlled trials (RCTs), including the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) and the Revascularization Investigation 2 Diabetes trials, have called into question whether percutaneous coronary intervention (PCI) reduces death or myocardial infarction (MI) in patients with stable ischemic heart disease (SIHD) relative to medical therapy (MT) alone. However, these trials randomized a broad population both with and without objective evidence of ischemia. In this regard, most previous studies have reported that objective evidence of myocardial ischemia bears both a qualitative and quantitative relation with subsequent clinical outcomes including death and nonfatal MI. To address this issue, the ongoing National Heart, Lung and Blood Institute–funded International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial (Identifier NCT01471522 ) is being conducted to evaluate ischemia-based revascularization for patients with moderate or severe ischemia. Pending these results, we performed a meta-analysis of existing RCTs comparing PCI with MT in patients with documented myocardial ischemia to elucidate whether objective ischemia may determine who may benefit from PCI versus MT alone.
Methods
The present study prespecified 2 important inclusion criteria: Given the low diagnostic accuracy of exercise treadmill testing (ETT) with solely symptom-based or electrocardiographic assessment of ischemia, we required ischemia to be documented by either noninvasive stress imaging or abnormal fractional flow reserve (FFR). Moreover, previous studies have most often focused on a primary end point of death or MI. As the definition of MI in these studies varies considerably between trials and as periprocedural and spontaneous MIs may have very different prognostic implications, all-cause mortality was chosen as the principal end point for the present analysis, which should reduce definitional and ascertainment bias of MI.
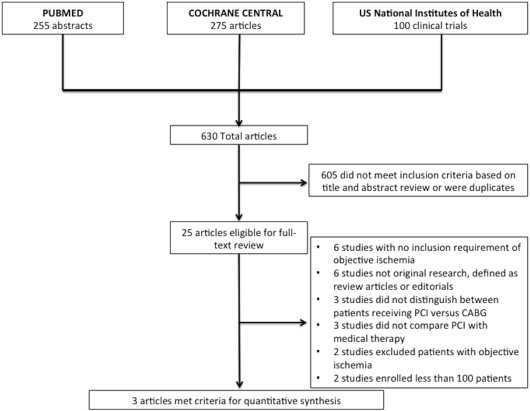
We searched for RCTs published from January 1980 to May 2013 that compared MT with PCI to MT alone in patients with coronary artery disease and objective findings of ischemia on noninvasive stress imaging or abnormal FFR. Trials were eligible if they enrolled ≥100 patients, reported all-cause mortality, reported outcomes at a specified time point in both arms, and did not use a control group from another study already included in the meta-analysis. Trials that relied solely on symptoms, electrocardiographic criteria, or ETT without imaging to qualify ischemia were excluded, as were trials that included coronary artery bypass grafting (CABG).
The results of the searches and study eligibility were independently assessed by 2 reviewers (HG and AJK) and screened for adequacy of follow-up and other study design characteristics including adequate randomization, intent-to-treat analyses, and end point reporting. Data extracted included the study characteristics, patient characteristics, details regarding the intervention and comparison groups, and outcome measures. Hazard ratios (HRs), where provided, and raw count data were ascertained for the PCI and MT groups for the primary end point of all-cause mortality.
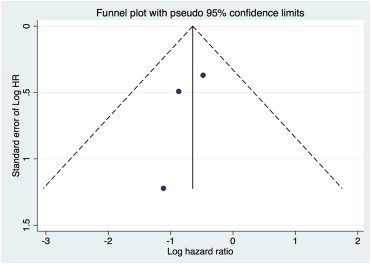
All analyses were performed using Stata/SE version 13.1 (StataCorp, College Station, Texas). Effect estimates with HRs and 95% confidence intervals were calculated for each study and assessed by both fixed and random effects (DerSimonian and Laird) models. The I 2 statistic was calculated to assess heterogeneity. Of note, the results of the fixed and random effects analyses were identical. Bias was estimated visually by Begg’s funnel plot and the Egger-weighted linear regression test. This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.
Results
Of 630 screened studies, we identified 3 RCTs that fulfilled the delineated inclusion criteria ( Figure 1 ). These included the COURAGE Nuclear Substudy 0, the Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2) Trial, and the Effects of Percutaneous Coronary Interventions in Silent Ischemia After Myocardial Infarction (SWISSI) II Trial. In aggregate, these trials enrolled 1,557 patients followed for a mean of 3.0 years (range 7 months to 10.2 years). The study characteristics of the included trials and baseline patient characteristics are presented in Tables 1 and 2 . The method of PCI differed in each study, with balloon angioplasty alone performed in SWISSI II, predominantly bare metal stents or balloon angioplasty in COURAGE and predominantly second-generation drug-eluting stents in FAME 2.
| Trial | Ischemia Testing; Primary Endpoint | Median Time to Follow-up |
|---|---|---|
| COURAGE Nuclear Substudy 0 | Moderate-to-severe defined as ≥3 ischemic segments on nuclear imaging; Composite of death from any cause or MI | 4.6 years |
| FAME 2 | Fractional flow reserve of ≤0.80; Composite of death from any cause, nonfatal MI, or urgent revascularization | 7 months |
| SWISSI II | Symptom-limited ETT with ST depression and confirming stress imaging; Cardiac death, nonfatal MI, and/or revascularization | 10.2 years |
| Variable | COURAGE Nuclear Substudy 0 | FAME 2 | SWISSI II | |||
|---|---|---|---|---|---|---|
| PCI + MT | MT | PCI + MT | MT | PCI + MT | MT | |
| Participants (n) | 223 | 245 | 447 | 441 | 96 | 105 |
| Age (mean, years) | 62 | 62 | 64 | 64 | 54 | 56 |
| Women | 14% | 13% | 20% | 23% | 12% | 13% |
| Cardiac risk factors | ||||||
| Hyperlipidemia | 44% | 49% | 74% | 79% | 75% | 58% |
| Hypertension | 69% | 71% | 78% | 78% | 45% | 45% |
| Diabetes | 32% | 39% | 28% | 27% | 9% | 13% |
| Current smoker | 29% | 24% | 20% | 20% | 73% | 74% |
| Prior MI | 40% | 39% | 37% | 38% | NR | NR |
| Prior PCI | 13% | 14% | 18% | 17% | NR | NR |
| CCS class | ||||||
| 0 | 15% | 13% | 12% | 11% | NR | NR |
| I | 28% | 34% | 18% | 22% | NR | NR |
| II | 35% | 36% | 46% | 45% | NR | NR |
| III | 22% | 17% | 18% | 15% | NR | NR |
| Medications | ||||||
| Antiplatelet | 93% | 91% | 87% | 90% | NR | NR |
| Anti-lipid | 75% | 69% | 83% | 82% | NR | NR |
| Beta-blocker | 72% | 68% | 76% | 78% | NR | NR |
| ACE-inhibitor or ARB | 54% | 57% | 69% | 70% | NR | NR |
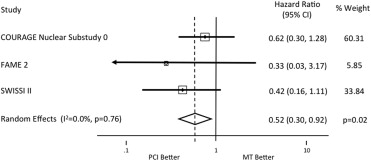
On the basis of raw counts, 3.0% (23 of 766) of the PCI plus MT strategy patients died versus 5.9% (47 of 791) of the MT alone strategy patients. In the analysis of pooled HRs, a statistically significant reduction in all-cause mortality was present with PCI plus MT versus MT alone (HR 0.52, 95% confidence interval 0.30 to 0.92, p = 0.02; Figure 2 ). The point estimate of the HR for mortality favoring PCI plus MT versus MT alone in each trial varied from 0.33 to 0.62, with no heterogeneity between studies ( I 2 = 0%) and no evidence of bias ( Figure 3 ; p = 0.46 by the Egger test).
Results
Of 630 screened studies, we identified 3 RCTs that fulfilled the delineated inclusion criteria ( Figure 1 ). These included the COURAGE Nuclear Substudy 0, the Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME 2) Trial, and the Effects of Percutaneous Coronary Interventions in Silent Ischemia After Myocardial Infarction (SWISSI) II Trial. In aggregate, these trials enrolled 1,557 patients followed for a mean of 3.0 years (range 7 months to 10.2 years). The study characteristics of the included trials and baseline patient characteristics are presented in Tables 1 and 2 . The method of PCI differed in each study, with balloon angioplasty alone performed in SWISSI II, predominantly bare metal stents or balloon angioplasty in COURAGE and predominantly second-generation drug-eluting stents in FAME 2.