Evidence regarding the safety and feasibility of transcatheter aortic valve implantation without balloon predilation (BP) is scarce. A literature search of PubMed, EMBASE, CENTRAL, and major conference proceedings was performed from January 2002 to July 2015. There were 18 studies incorporating 2,443 patients included in the present study. No differences were observed in the baseline characteristics between patients without BP (no-BP) and with BP. Compared with BP, no-BP had a shorter procedure time (no-BP vs BP, 124.2 vs 138.8 minutes, p = 0.008), used less-contrast medium (no-BP vs BP, 126.3 vs 156.3 ml, p = 0.0005) and had a higher success rate (odds ratio [OR] 2.24, 95% CI 1.40 to −3.58). In addition, no-BP was associated with lower incidences of permanent pacemaker implantation (OR 0.45, 95% CI 0.3 to 0.67), grade 2 or greater paravalvular leakage (OR 0.55, 95% CI 0.37 to 0.83), and stroke (OR 0.57, 95% CI 0.32 to 1.0). Furthermore, no-BP was associated with a 0.6-fold decreased risk for 30-day all-cause mortality (OR 0.60, 95% CI 0.39 to 0.92). However, the difference in the risk for permanent pacemaker implantation, grade 2, or higher aortic regurgitation, stroke was noted to be significant only in the subgroup of the CoreValve-dominating studies. In conclusion, no-BP before transcatheter aortic valve implantation was not only safe and feasible but was also associated with fewer complications and short-term mortality in selected patients especially using self-expandable valve.
Transcatheter aortic valve implantation (TAVI) is equivalent to surgical aortic valve implantation for the treatment of symptomatic aortic stenosis deemed to be higher surgical risk. Balloon predilation (BP) before TAVI has been considered a mandatory step that may ensure a final measurement of aortic annulus, facilitate the deployment of prosthesis, and rule out coronary occlusion. Furthermore, prepared BP may reduce the radial counterforce. Thus, optimal expansion of the deployed transcatheter heart valve would be achieved. However, BP is also a double-edged sword that may increase the incidence of distal embolization and permanent pacemaker implantation (PPM). Therefore, elucidating whether TAVI can be performed without previous BP is essential. Only a limited number of studies exist that report the safety and feasibility of TAVI without BP. Thus, the purpose of the present study was to investigate the benefits and risks of TAVI without BP by pooling all relevant studies regarding the comparison between TAVI with and without BP.
Methods
A literature search of PubMed, EAMBASE, CENTRAL, and major conference proceeding was performed using the following search strategy: (TAVI OR TAVR OR transcatheter valve OR transcatheter aortic valve OR transcatheter heart valve OR percutaneous valve OR percutaneous aortic valve) and (pre-dilation OR balloon aortic valvuloplasty OR BAV OR predilation). The time interval of the search was limited to January 2002 to July 2015.
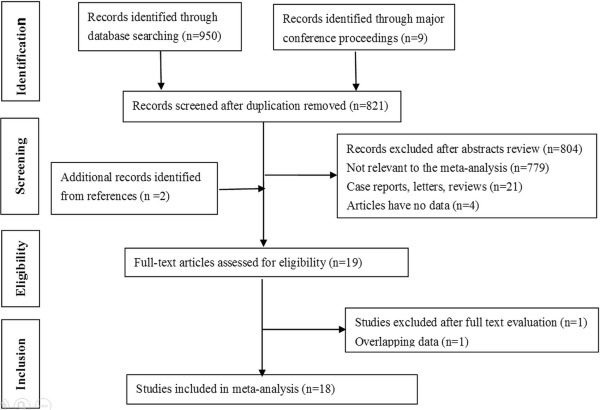
The inclusion criteria included studies and conference proceedings reporting a discrepancy in the outcome between no-BP and BP. Studies were excluded if they were a letter, review, case report, or editorial. Only studies published in English were included. In addition, studies that only reported the outcome of no-BP without comparing the outcome to BP were also ruled out. The study selections process is illustrated in Figure 1 .
Two investigators (LYB and MY) independently extracted the relevant data including investigators, published years, number, baseline characteristics, procedure characteristics, post-TAVI complications, and mortality ( Supplementary Table 1 ). Consensus was achieved on all items afterward.
Categorical variables are presented as n (%), whereas continuous variables are presented as the mean ± SD or median (25th to 75th inter quartile range) according to the variable distribution. Data synthesis and analysis were performed using RevMan software version 5. The mean difference and odds ratio (OR) were acquired to evaluate the safety and feasibility of TAVI without BP. Heterogeneity was assessed by calculating the I 2 statistic and its p value. If the I 2 statistic was >50% and its p value was <0.1, a random-effects model was used to obtain the combined effect estimates. Two-sided p values of 0.05 were considered statistically significant.
Subgroup analysis was performed according to valve type to investigate the influence of valve type on the results. Publication bias was evaluated by visual inspection of symmetry of the funnel plot. If the number of pooled studies was small, publication bias was not performed.
The present systematic review and meta-analysis was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses group.
Results
The process of literature search and study selection is illustrated in Figure 1 . A total of 950 citations and 9 conference proceedings were retrieved, and 821 relevant citations remained after removing duplicate citations. Only 19 studies were eligible for full-text evaluation after title and abstract screening. Finally, 18 studies were included in the present meta-analysis after excluding a study with overlapping data ( Figure 1 ).
Characteristics of the included studies are presented in Supplementary Table 1 . Although there were 18 studies reporting discrepancies between no-BP and BP, only 8 studies detailed baseline characteristics. No significant differences were found in the baseline characteristics between no-BP and BP ( Table 1 ).
| Characteristics | N of study | N of patients | Statistical method | Model | Estimate effect | I2 (%) |
|---|---|---|---|---|---|---|
| Age (Years) | 7 | 767 | MD | Fixed | 0.27 (-11.75, 12.29) | 0 |
| Men | 8 | 803 | OR | Fixed | 1.00 (0.74, 1.35) | 0 |
| Body mass index | 4 | 232 | MD | Fixed | -0.04 (-1.17, 1.08) | 23 |
| Diabetes mellitus | 6 | 518 | OR | Fixed | 1.00 (0.68, 1.47) | 5 |
| Coronary artery disease | 7 | 598 | OR | Fixed | 0.95 (0.67, 1.35) | 0 |
| Previous myocardial infarction | 5 | 494 | OR | Random | 1.42 (0.49, 4.14) | 65 |
| Previous stroke | 5 | 312 | OR | Fixed | 1.00 (0.52, 1.90) | 0 |
| Peripheral artery disease | 3 | 266 | OR | Fixed | 1.44 (0.78, 2.68) | 37 |
| Estimate glomerular filtration fraction | 2 | 156 | MD | Fixed | -5.67 (-13.04, 1.71) | 0 |
| Chronic obstructive pulmonary disease | 6 | 498 | OR | Fixed | 0.89 (0.57, 1.38) | 0 |
| Pulmonary hypertension | 4 | 362 | OR | Fixed | 0.88 (0.52, 1.49) | 0 |
| NYHA class III/IV | 6 | 498 | OR | Fixed | 1.43 (0.86, 2.40) | 0 |
| Left ventricular ejection function | 3 | 405 | MD | Fixed | -1.44 (-4.13, 1.24) | 41 |
| Logitic EuroSCORE (%) | 7 | 767 | MD | Fixed | 0.89 (-0.80, 2.58) | 0 |
| Annulus diameter (mm) | 3 | 357 | MD | Fixed | 0.46 (-0.02, 0.94) | 0 |
| Aortic valve area (mm 2 ) | 6 | 667 | MD | Random | 0.01 (-0.07, 0.09) | 78 |
| Mean transaortic gradient (mmHg) | 6 | 466 | MD | Random | -4.30 (-8.73, 0.12) | 52 |
| Peak transaortic gradient (mmHg) | 5 | 525 | MD | Fixed | -2.61 (-6.90, 1.68) | 6 |
In addition, only 4 studies that compared the calcification of native aortic valve between 2 strategies were listed ( Table 2 ). Three studies reported no significant difference in severity of calcium, whereas one study reported that no-BP was performed when patients did not have a grade 2 or more calcified aortic valve, calcium nodules, and left ventricular outflow tract calcification.
| Author | Year | BAV | Valve calcification |
|---|---|---|---|
| Fiorina | 2014 | 0 | The total amount of calcification in the device landing zone: grade 1-2: 10 (18%); grade 3-4: 45 (82%) |
| + | The total amount of calcification in the device landing zone: grade 1-2: 9 (20%); grade 3-4: 36 (80%) | ||
| Mollmann | 2014 | 0 | Calcium score of the aortic valve: 2464 (1480-3466) |
| + | Calcium score of the aortic valve: 2531 (1645-3277) | ||
| Islas | 2015 | 0 | Central orifice; calcification ≤ grade 2; no LVOT calcification; absence of calcium nodules |
| + | Eccentric and/or irregular; calcification > grade 2; LVOT calcification; calcium modules | ||
| Kempfert | 2015 | 0 | After calcium score of the aortic valve matching, no predilation had a lower rate of transient ischemic attack in comparison with that have prior predilation |
| + |
Compared with BP before TAVI, no-BP had a shorter procedure time, fluoroscopic time, and less amount of contrast medium ( Supplementary Table 2 ). Moreover, no-BP was associated with a 2.24-fold higher success rate (OR 2.24, p = 0.0008, Figure 2 ).
Compared with those patients with BP, no-BP had lower incidence of PPM (OR 0.45, p <0.0001, Figure 3 ), grade 2 or higher aortic regurgitation (OR 0.55, p = 0.004, Figure 4 ), and stroke (OR 0.47, p = 0.05, Figure 5 ). Besides, no-BP was associated with a numerically lower incidence of acute kidney injury (AKI) compare with BP (OR 0.66, p = 0.08). All the pooled results had no significant heterogeneity ( Supplementary Table 2 ).
A total of 9 studies and 7 studies including 1,261 and 568 patients, respectively, reported the mean transaortic gradient and aortic valve area after TAVI. There were no significant differences in the mean transaortic gradient and aortic valve area after TAVI between no-BP and BP ( Supplementary Table 2 ).
In 13 studies incorporating 2,097 patients, we found that no-BP had a lower 30-day all-cause mortality (OR 0.60, p = 0.02, Figure 6 ), whereas no-BP was associated with no significant difference in 1-year all-cause mortality. No significant heterogeneity was noted in the pooled results ( Supplementary Table 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


