Atrial fibrillation (AF) is 1 of the most clinically diagnosed cardiac disturbances but little is known about its risk factors. Previous epidemiologic studies have reported on the association between diabetes mellitus (DM) and subsequent risk of AF, with inconsistent results. The aim of this study was to conduct a meta-analysis of published studies to reliably determine the direction and magnitude of any association between DM and AF. A systematic review and meta-analysis was conducted. PubMed and EMBASE were searched to identify prospective cohort and case–control studies that had reported on the association between DM and other measurements of glucose homeostasis with incident AF by April 2010. Studies conducted in primarily high-risk populations and participants in randomized controlled trials were excluded. Seven prospective cohort studies and 4 case–control studies with information on 108,703 cases of AF in 1,686,097 subjects contributed to this analysis. The summary estimate indicated that patients with DM had an approximate 40% greater risk of AF compared to unaffected patients (relative risk [RR] 1.39, 95% confidence interval [CI] 1.10 to 1.75, p for heterogeneity <0.001). After correcting for publication bias, the RR was 1.34 (1.07 to 1.68). Studies that had adjusted for multiple risk factors reported a smaller effect estimate compared to age-adjusted studies (RR 1.24, 95% CI 1.06 to 1.44, vs 1.70, 1.29 to 2.22, p for heterogeneity = 0.053). The population-attributable fraction of AF owing to DM was 2.5% (95% CI 0.1 to 3.9). In conclusion, DM is associated with an increased risk of subsequent AF but the mechanisms that may underpin the relation between DM and AF remain speculative.
Aside from age, established risk factors for atrial fibrillation (AF) include heart failure and valvular heart disease and some cardiovascular risk factors such as increased blood pressure, obesity, and smoking. In addition to these risk factors, observational studies have reported on the association between diabetes mellitus (DM) and AF, but with equivocal results. The discrepancies in study findings may be due in part to methodologic challenges such as limited power and small effect size. Thus, the aim of this article was to quantify the magnitude and direction of the reported association between DM and AF by conducting a systematic review and meta-analysis of published cohort and case–control studies.
Methods
We performed a systematic review of the available literature according to Meta-Analysis Of Observational Studies in Epidemiology (MOOSE) guidelines for the conduct of meta-analyses of observational studies. Relevant studies were identified by computerized searches from the following data sources: MEDLINE via Ovid (from 1950 through April 2010) and EMBASE (from 1966 through May 2010) using relevant text words and medical subject headings that included all spellings of “type 2 diabetes” or “diabetes mellitus” or “glucose intolerance” or “impaired fasting glucose” and “atrial fibrillation.” The search was limited to prospective cohort and case–control studies in predominantly healthy adult populations without language restriction. Studies of high-risk populations and reports from randomized controlled trials were excluded ( Figure 1 ).
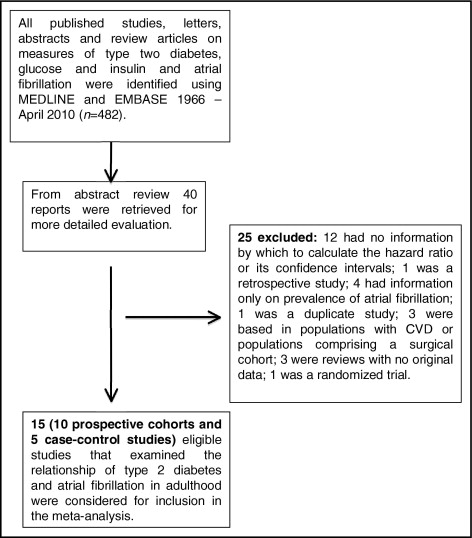
All cohort studies and case–control studies that had reported on the association between DM and AF were eligible for inclusion. Studies of populations that comprised patients who had undergone cardiac surgery or those with established cardiac disease were excluded.
Quantitative estimates (hazard ratio, relative risk [RR], or odds ratio [OR]) and 95% confidence intervals (CIs; or another measurement of variance) of the association between DM and AF were extracted from each study. Where possible the age-adjusted estimate (and where appropriate, age- and gender-adjusted estimate) and multiple adjusted risk estimate (and corresponding 95% CI) were extracted from individual studies. Additional information on patient characteristics at study baseline (e.g., mean age, gender distribution, and race) was also extracted from the published reports. Information on variables included in the multivariable model was also recorded, as was method of case ascertainment and study exposure.
Summary estimates were obtained using a random-effects model to account for between-study heterogeneity. Overall and cohort estimates are presented as RRs with 95% CIs, and case–control estimates are presented as ORs with 95% CIs. For those studies that had reported the 2 multiple risk estimates, only the most adjusted estimated contributed to the summary estimates. Percent variability across studies attributable to heterogeneity beyond chance was estimated using the I 2 statistic. To examine the influence of study-level covariates on the effect of DM on risk of AF, 2 meta-regression models on the log(RR) scale were constructed. The first examined the impact of study design (i.e., cohort vs case–control), and the second investigated the impact of level of adjustment. For the latter model, studies were classified into “least adjusted” if they had adjusted for only age and gender and “most adjusted” if they had adjusted for additional variables ( Tables 1 and 2 ), and a corresponding indicator variable was included in the model. Publication bias was assessed using the Egger test and trim-and-fill analyses were used to adjust RRs for presence of publication bias. A p value <0.05 was considered statistically significant for all analyses. All statistical analyses were performed with STATA 11.1 (STATA Corporation, College Station, Texas).
| Study (year) | Date of enrollment | Country | Subjects (percentage of women) | Mean Age (years) | Mean Follow-Up (years) | Incident Cases of AF (%) | IR (per 1,000 person-years) | DM Diagnosis | AF Diagnosis | Covariates in Model |
|---|---|---|---|---|---|---|---|---|---|---|
| Krahn et al (1995) | 1948 | Canada | 3,983 (0%) | 72 | 44 | 299 (7.5%) | 0.5 <50 years, 2.3 at 60 years, 16.9 at 85 years | NA | ECG | age, cardiac conditions, alcohol, smoking, obesity |
| Benjamin et al (1998) | 1948 | United States | 4,731 (56%) | 55–94 | 38 | 562 (11.9%) | 6.2 (55–64 years, men), 3.8 (55–64 years, women) | FBG/diabetes medication | ECG | age, smoking, ECG, hypertension, MI, CHF, valve disease |
| Watanabe et al (2008) | 1996–1998 | Japan | 28,449 (66%) | 59 | 4.5 | 265 (9.3%) | 4.1 (men, 1.3 (women) | IGT/ ⁎ diabetes medication | ECG | age, gender |
| Ruigómez et al (2002) | 1996 | United Kingdom | 703,340 | 40–89 | NA | 1,035 (0.1%) | 1.7 | MRs | ECG | age, gender, CVD morbidity |
| Frost et al (2005) | 1993–2001 | Denmark | 47,589 | 50–64 | 5.7 | 553 (1.2%) | 2.9 (men), 1.2 (women) | NA | ECG | BMI, age, height, education, smoking, alcohol, IHD, CHF, hypertension |
| Rosengren e al (2009) | 1970–1973 | Sweden | 6,903 (0%) | 51 | 34 (maximum) | 1,253 (18.2%) | 7.5 (nondiabetics), 7.1 (diabetics) | SR | ECG | age |
| Smith et al (2010) | 1991–1996 | Sweden | 30,447 (60%) | 44–73 | 11.2 | 1,430 (4.7%) | 6.3 (men), 3.1 (women) | SR/diabetes medication | ECG | age, BMI, smoking, BP, previous cardiac disease |
⁎ This study reported on relation between impaired glucose tolerance according to National Cholesterol Education Program Adult Treatment Panel III guidelines and risk of atrial fibrillation.
| Study | Date of Study | Country | Subjects | Prevalent AF | Mean Age (years) | DM Diagnosis | AF Diagnosis | Covariates in Model |
|---|---|---|---|---|---|---|---|---|
| Nichols et al (2009) | 1999–2004 | United States | 17,372 diabetics, 17,373 controls | 626 cases (3.6%), 434 (2.5%) | 58 | inpatient/outpatient diagnosis | MRs | age, gender, ethnicity, smoking, obesity, hypertension, CAD |
| Dublin et al (2010) | 2001–2004 | United States | 1,410 with AF, 2,203 controls | NA | 55–94 | MRs | MRs | adjusted for age, gender, calendar year, treated hypertension, BMI |
| Movahed et al (2005) | 1990–2000 | United States | 293,124 diabetics, 552,624 controls | 43,674 cases (14.9%), 57,077 controls (10.3%) | 65 | MRs | MRs | CHF, CAD, LVH |
| Johansen et al (2008) | NA | Norway | 46 with AF, 108 controls | NA | 75 | OGTT | ECG | none |
To ascertain what proportion of the burden of AF might theoretically be avoided if DM could be entirely eliminated from the population, we used the following population-attributable fraction formula : PAF = PD([RR − 1])/RR, where PAF is the population-attributable fraction and PD is the prevalence of DM among AF cases. This prevalence was estimated using the average prevalence of the case series of included case–control studies.
Results
Six prospective cohort studies relating DM to subsequent risk of AF involving 5,436 incident cases of AF in 801,837 patients were identified. An additional cohort including 265 incident cases of AF in 28,449 patients reported on the association between impaired glucose tolerance and risk of AF ( Table 1 ). Three of the 7 cohort studies provided gender-specific estimates adjusted at least for age of the association between DM and AF; thus, 10 separate estimates of the relation contributed to this analysis. All but 1 of the studies were from populations in North America (n = 2) or Europe (n = 4), with the remaining study from Japan.
Characteristics of cohort study participants are presented in Table 1 . Four case–control studies including information on 103,267 cases of prevalent AF in 884,260 patients are included in this review ( Table 2 ). One of the 4 case–control studies provided gender-specific estimates; hence, there were 5 separate estimates from these 4 studies that contributed to this analysis. The following analyses are therefore based on 108,703 cases of AF in 1,686,097 patients.
Three prospective cohort studies involving 1,104 incident cases of AF in 20,871 patients and 1 case–control study involving 42 patients with AF and 549 control subjects were unable to contribute to the meta-analysis. Although these studies had commented on the direction of the association between DM (or serum blood glucose) and AF, no quantitative estimate was reported ( Table 3 ). In 3 of these studies, there was no association between DM or blood sugar level and risk of AF. In the remaining study, there was a positive association between glucose level and risk of AF (RR 1.10, 95% CI 1.04 to 1.17) per millimoles per liter of glucose but it did not provide a quantitative estimate for the DM–AF relation.
| Study | Date of Study | Country | Subjects | Mean Age (years) | Mean Follow-Up (years) | Incident Cases of AF (%) | IR (per 1,000 person-years) | Direction of Association of Exposure With AF | Covariates in Model |
|---|---|---|---|---|---|---|---|---|---|
| Psaty et al (1997) | 1989–1993 | United States | 4,844 | >65 | 3.3 | 304 (6.3%) | 17.6 (65–74 years, men), 10.1 (65–74 years, women) | positive 1.10 (95% CI 1.04–1.17) per mmol/L glucose | alcohol, SBP, age, height, TC, ethnicity, β blockers, diuretics |
| Wilhelmsen et al (2001) | 1970–1973 | Sweden | 7,495 | 47–55 | 25.2 | 754 (10.1%) | NA | no significant association; no data given | NA |
| Stewart et al (2002) | 1972–1976 | Scotland | 8,532 | 45–64 | 4.1 | 46 (0.5%) | 0.54 | no significant association with blood glucose | NA |
| Agmon et al (2001) | NA | United States | 42 with AF, 539 controls | 82 (patients), 66 (controls) | — | — | — | no association (p = 0.27) | none |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


