The aim of this study was to compare the safety and efficacy of coronary artery bypass grafting (CABG) with percutaneous coronary intervention (PCI) using drug-eluting stents (DES) in patients with unprotected left main coronary artery (ULMCA) disease. The current American College of Cardiology and American Heart Association guidelines recommend CABG for the treatment of patients with ULMCA disease on the basis of clinical trials demonstrating a survival benefit with CABG compared to medical therapy. DES reduce the rate of target vessel revascularization compared with bare-metal stents in ULMCA PCI and may be a safe alternative to CABG. A meta-analysis was conducted of clinical studies comparing CABG and PCI with DES for ULMCA disease with respect to death; the composite of death, myocardial infarction, or stroke; and target vessel revascularization at 1 year follow-up. The analysis included 2,905 patients from 8 clinical studies (2 randomized trials and 6 nonrandomized studies). At 1-year follow-up, there was no significant difference between the CABG and DES groups in the risk for death (odds ratio [OR] 1.12, 95% confidence interval [CI] 0.80 to 1.56) or the composite end point of death, myocardial infarction, or stroke (OR 1.25, 95% CI 0.86 to 1.82). The risk for target vessel revascularization was significantly lower in the CABG group compared to the PCI group (OR 0.44, 95% CI 0.32 to 0.59). In conclusion, PCI with DES is safe and could represent a good alternative to CABG for selected cases in patients with ULMCA disease.
The current American College of Cardiology, American Heart Association, and Society for Cardiovascular Angiography and Interventions guidelines recommend coronary artery bypass grafting (CABG) for the treatment of patients with unprotected left main coronary artery (ULMCA) disease on the basis of clinical trials demonstrating a survival benefit with CABG compared with medical therapy. One of the main limitations of ULMCA percutaneous coronary intervention (PCI) is in-stent restenosis and the need for repeat revascularization. According to the American College of Cardiology and American Heart Association guidelines and the European Society of Cardiology guidelines, ULMCA PCI should be reserved for those who are poor candidates for CABG. Drug-eluting stents (DES) are the preferred type of stents on the basis of superior intermediate-term outcomes with ULMCA PCI with DES compared with bare-metal stents. We performed a meta-analysis to compare CABG to PCI with DES for the treatment of ULMCA disease.
Methods
We conducted a computerized search of Medline, EMBASE, the Cochrane databases, and presentations of data sets at the major meetings of the American Heart Association, American College of Cardiology, and Transcatheter Cardiovascular Therapeutics from January 2000 to June 2009 for clinical studies using the Medical Subject Heading terms “coronary artery bypass graft surgery,” “drug-eluting stent,” “sirolimus-eluting stent,” “paclitaxel-eluting stent,” and “unprotected left main disease.” We used the Science Citation Index to cross-reference for further studies that met our criteria.
The studies included in this meta-analysis were based on predetermined criteria: (1) clinical trials published in peer-reviewed journals with full available text or presentations at major cardiology meetings in English, (2) comparison of the efficacy of CABG to that of DES in patients with ULMCA disease, and (3) follow-up of ≥12 months. Studies using only bare-metal stents or mixtures of bare-metal stents and DES in the PCI group were excluded from this study.
The end points of this meta-analysis were (1) mortality; (2) the composite of death, myocardial infarction, or stroke; (3) target vessel revascularization; and (4) myocardial infarction. Target vessel revascularization was defined as repeat revascularization of the treated vessel, including any segments of the left anterior descending and/or left circumflex coronary artery. Revascularization was performed according to study protocol or a clinical indication. Two independent reviewers (TY and JD) extracted the data, including the first author of the study, baseline demographics, sample size, clinical events, and length of follow-up.
The meta-analysis was completed using Comprehensive Meta-Analysis version 2 (Biostat Inc., Englewood, New Jersey). A fixed-effect model of meta-analysis was used to aggregate the study-level data. Forest plots were generated for graphical presentations for clinical outcomes, and Q statistics were computed to assess heterogeneity across the different studies. For each study in the analysis, odds ratios (ORs) as well as 95% confidence intervals (CIs) were calculated on the basis of rates comparing CABG to DES for each of the extracted data points. All p values were 2 tailed, with statistical significance at 0.05. The baseline characteristics were analyzed with weighted means and SDs for continuous variables and weighted proportions for binary variables. Microsoft Excel (Microsoft Corporation, Redmond, Washington) was used as ancillary software to calculate p values comparing the 2 groups’ baseline covariates using 2-sample Student’s t tests for continuous data and chi-square tests for categorical data.
Results
Eight studies met our criteria for inclusion in the meta-analysis ( Table 1 ). A total of 2,905 patients were included in the analysis, with 1,669 patients who underwent CABG and 1,236 patients who underwent PCI with DES. Two of the 8 studies were randomized controlled trials. The trial by Boudriot et al, which used sirolimus-eluting stents, and Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX), which used paclitaxel-eluting stents, were multicenter trials that randomized patients with ULMCA disease to CABG or DES. The other 6 studies in this meta-analysis were observational studies with matched cohorts or consecutive patients. Wave 2 patients (those with DES) from the Revitalization for Unprotected Left Main Coronary Artery Stenosis: Comparison of Percutaneous Coronary Angioplasty Versus Surgical Revascularization (MAIN-COMPARE) registry were used in our analysis.
| Study | Patients (n) | Follow-Up (months) | Age (years) | Men (%) | Hypertension (%) | DM (%) | Hyperlipidemia (%) | Current Smoking (%) | Previous MI (%) | Previous PCI (%) | Previous CVA (%) | UA (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lee et al | 123/50 | 12 | 70/72 | 76/50 | 81/88 | 31/36 | 72/74 | 19/12 | NR/NR | NR/NR | 10/8 | 25/46 |
| Chieffo et al | 142/107 | 12 | 68/64 | NR/NR | 76/59 | 23/19 | 69/70 | 59/50 | NR/NR | NR/NR | NR/NR | 22/32 |
| MAIN-COMPARE | 396/396 | 12 | 66/66 | 72/72 | 37/36 | 37/36 | 34/33 | 26/26 | 9/9 | 15/15 | 7/8 | 58/58 |
| SYNTAX | 302/312 | 12 | 66/65 | 76/72 | 77/71 | 22/22 | 75/81 | 24/18 | 25/29 | NR/NR | NR/NR | 29/31 |
| Palmerini et al | 161/98 | 12 | 78/81 | 66/54 | 73/77 | 26/31 | NR/NR | 39/39 | NR/NR | NR/NR | 2/5 | NR/NR |
| Sanmartín et al | 245/96 | 12 | 66/66 | 87/81 | 60/44 | 32/19 | 46/42 | 46/39 | NR/NR | 9/15 | NR/NR | NR/NR |
| Boudriot et al | 84/83 | 12 | 69/66 | 77/71 | 82/81 | 25/43 | 64/70 | 25/34 | NR/NR | NR/NR | NR/NR | NR/NR |
| Cheng et al | 216/94 | 12 | 67/68 | 76/75 | 73/73 | 51/35 | 46/72 | 31/20 | 29/19 | 23/39 | 15/12 | 67/60 |
The CABG group had significantly higher percentages of men (76% vs 69%, p = 0.0025), hypertension (66% vs 61%, p = 0.015), and previous myocardial infarctions (16% vs 11%, p = 0.01).
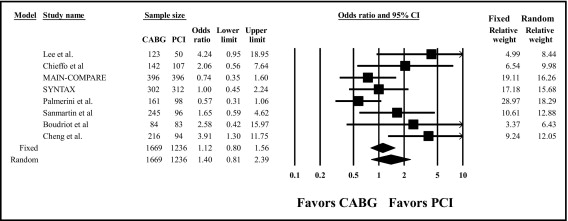
The risk for death at 1 year did not differ significantly between the CABG and DES groups (OR 1.12, 95% CI 0.80 to 1.56; Figure 1 ). The chi-square test of all studies under a common treatment effect was significant (p = 0.03), and the observed Q statistic of 15.85 versus the expected Q statistic of 7 indicated significant heterogeneity among the studies. A random-effects model was therefore used to analyze the heterogeneity, and the result was found to be consistent (OR 1.40, 95% CI 0.81 to 2.39).
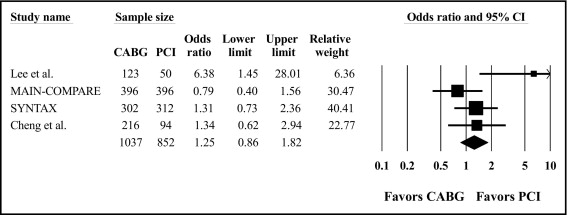
The risk for the composite of death, myocardial infarction, or stroke did not significantly differ between the CABG and DES groups (OR 1.25, 95% CI 0.86 to 1.82; Figure 2 ). There was no significant heterogeneity among the studies (p = 0.09).
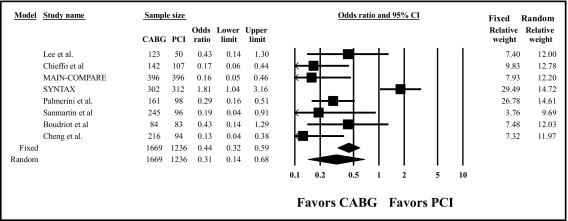
The risk for target vessel revascularization was significantly lower in the CABG group compared to the DES group (OR 0.44, 95% CI 0.32 to 0.59; Figure 3 ). The chi-square test of homogeneity (all studies under a common treatment effect) was significant (p <0.001, the observed Q statistic of 40.29 vs the expected Q statistic of 7) indicating significant heterogeneity among the studies. A random-effects model was therefore used to analyze the heterogeneity, and the result was found to be consistent (OR 0.31, 95% CI 0.14 to 0.68). The rate of target vessel revascularization was not reported in all the studies. Any repeat revascularization rate was reported and used in place of target vessel revascularization in the SYNTAX trial and the studies by Sanmartín et al and Boudriot et al. The studies by Palmerini et al and Cheng et al reported target lesion revascularization, and this was used in place of target vessel revascularization in our analysis.
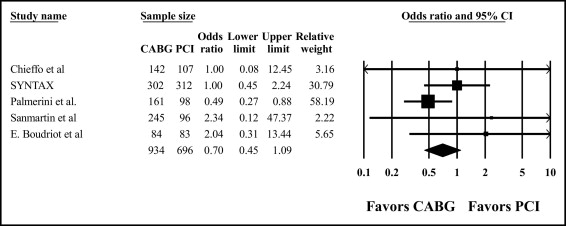
The risk for myocardial infarction did not significantly differ between the CABG and DES groups (OR 0.70, 95% CI 0.45 to 1.09; Figure 4 ). There was no significant heterogeneity among the studies (p = 0.39).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


