The purpose of the present study was to determine the prognostic value of N-terminal pro-brain natriuretic peptide (NT-pro-BNP), among other serum biomarkers, on cardiac magnetic resonance (CMR) imaging parameters of cardiac function and infarct size in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. We measured NT-pro-BNP, cardiac troponin T, creatinine kinase-MB fraction, high-sensitivity C-reactive protein, and creatinine on the patients’ arrival at the catheterization laboratory in 206 patients with ST-segment elevation myocardial infarction. The NT-pro-BNP levels were divided into quartiles and correlated with left ventricular function and infarct size measured by CMR imaging at 4 to 6 months. Compared to the lower quartiles, patients with nonanterior wall myocardial infarction in the highest quartile of NT-pro-BNP (≥260 pg/ml) more often had a greater left ventricular end-systolic volume (68 vs 39 ml/m 2 , p <0.001), a lower left ventricular ejection fraction (42% vs 54%, p <0.001), a larger infarct size (9 vs 4 g/m 2 , p = 0.002), and a larger number of transmural segments (11% of segments vs 3% of segments, p <0.001). Multivariate analysis revealed that a NT-pro-BNP level of ≥260 pg/ml was the strongest independent predictor of left ventricular ejection fraction in patients with nonanterior wall myocardial infarction compared to the other serum biomarkers (β = −5.8; p = 0.019). In conclusion, in patients with nonanterior wall myocardial infarction undergoing primary percutaneous coronary intervention, an admission NT-pro-BNP level of ≥260 pg/ml was a strong, independent predictor of left ventricular function assessed by CMR imaging at follow-up. Our findings suggest that NT-pro-BNP, a widely available biomarker, might be helpful in the early risk stratification of patients with nonanterior wall myocardial infarction.
Cardiovascular magnetic resonance (CMR) imaging is now the reference standard for determining left ventricular (LV) function and infarct size (late gadolinium enhancement) in patients with ST-segment elevation myocardial infarction. We sought to evaluate whether the plasma levels of admission N-terminal pro-brain natriuretic peptide (NT-pro-BNP) relates to left ventricular (LV) function and infarct size measured by CMR imaging during follow-up and compared the NT-pro-BNP values with those of other serum biomarkers associated with prognosis, including cardiac troponin T, creatinine clearance rate, and C-reactive protein (CRP).
Methods
All patients included in the present study were participants in the PRoximal Embolic Protection in Acute myocardial infarction and Resolution of ST-Elevation (PREPARE) trial. In this 2-center, randomized, open trial, patients with ST-segment elevation myocardial infarction were randomized to primary percutaneous coronary intervention (PCI) with combined proximal embolic protection and thrombus aspiration (n = 141) or primary PCI alone (n = 143). The results from that randomized trial have been previously published. In brief, the patients were eligible for inclusion in the PREPARE trial if they had experienced an onset of symptoms of myocardial infarction <6 hours before presentation and had electrocardiographic evidence of persistent ST-segment elevation of ≥200 μV in ≥2 contiguous leads and Thrombolysis In Myocardial Infarction flow grade 0 to 1 on diagnostic angiography. The exclusion criteria were age <18 years, any contraindications to the use of glycoprotein IIb/IIIa receptor antagonists, coexistent conditions associated with a limited life expectancy, previous coronary artery bypass grafting or lytics, and recurrence of myocardial infarction in the same myocardial area. The primary end point of the PREPARE study was ST-segment resolution at 60 minutes after the last contrast injection, as determined using continuous ST-Holter monitoring and analyzed at an independent core laboratory. All reported clinical end points have been previously defined. The clinical end points included death, spontaneous or procedural myocardial infarction, stroke, and percutaneous or surgical target vessel revascularization. The present analysis included patients with an admission blood sample and CMR imaging parameters.
Blood samples were collected in 4.5-ml, gel/lithium heparin-coated tubes through the arterial sheath at the start of the procedure, centrifuged without undue delay, and stored at −70°C until further analysis. NT-pro-BNP was measured off-line (Hitachi Modular E-170, Roche Diagnostics GmbH, Mannheim, Germany). The coefficient of variation was 2.7% at 125 pg/ml, 1.8% at 177 pg/ml, and 2.4% 355 pg/ml, respectively. The functional detection limit was 50.0 pg/ml, and linearity was ≤70,000 pg/ml. Serum cardiac troponin T was determined using a Hitachi modular E-170 analyzer (Roche Diagnostics). Cardiac troponin T elevation was determined as ≥0.03 μg/L for the detection of myocardial infarction. The lower detection limit of this assay is ≤0.01 μg/L with a recommended diagnostic threshold of ≤0.03 μg/L. Creatine kinase-myocardial band (CK-MB) mass levels were measured at admission and after 5, 7, 10, 12, 18, and 24 hours for determination of the infarct size, using an immunoassay (Hitachi Modular E-170, Roche Diagnostics). The upper limit of normal of the CK-MB mass was ≤7.0 μg/L. Creatinine and CRP were measured on the Hitachi Modular P-unit (Roche Diagnostics). The lower and upper limit of normal for creatinine was 65 and 95 μmol/L for women and 75 and 110 μmol/L for men, respectively. The upper limit of normal for CRP was ≤3.0 mg/L. For values less than the limit of detection of cardiac troponin T and CRP, the upper limit of normal was used for statistical analysis. The estimated creatinine clearance rate was calculated according to the Cockcroft and Gault formula and defined as abnormal if ≤90 ml/min, as reported previously. All testing was performed by personnel unaware of the patients’ baseline characteristics and clinical outcomes.
As a part of an ancillary study, the patients underwent CMR imaging at 4 to 6 months after the index procedure. CMR imaging was performed with a 1.5-T clinical scanner (Sonato/Avanto, Siemens, Erlangen, Germany). Functional assessment was studied with a standard cine steady-state free precession sequence, and late gadolinium enhancement images were acquired after administration of gadolinium-based contrast agent (0.2 mmol/kg, Magnevist, Schering AG, Berlin, Germany). All functional and late gadolinium enhancement images were analyzed, as described previously. The CMR data were analyzed by a single experienced physician (JDEH) who was unaware of the clinical data using the MASS software, version 5.1 (MEDIS Medical Imaging Systems, Leiden, The Netherlands).
The patients were divided according to highest (≥260 pg/ml) and lower (<260 pg/ml) quartiles of NT-pro-BNP levels. The continuous baseline variables are expressed as the mean ± SD or median (interquartile range) and compared using the unpaired Student t test or Mann-Whitney U test, as appropriate. Categorical baseline variables were compared using Fisher’s exact test or chi-square statistic, as appropriate. The association between an admission NT-pro-BNP level of ≥260 pg/ml and LVEF (percentage) and infarct size (g/m 2 ) was investigated using a multivariate linear regression model adjusted for the other serum biomarkers in predicting LVEF or infarct size (admission CK-MB mass ≥7.0 μg/L, admission troponin T ≥0.03 μg/L, admission CRP ≥3 mg/L, and admission creatinine clearance rate of ≤90 ml/min). All serum biomarkers were entered en bloc. Patients who died during the study period received imputed values equal to the worst cardiac CMR parameters in our study population. Analysis of variance was used to test the significance of the interaction between infarct location and the effect of the admission NT-pro-BNP level on LVEF. Statistical analysis was performed using the Statistical Package for Social Sciences software, version 16.0, for Windows (SPSS, Chicago, Illinois). A p value <0.05 was considered statistically significant.
Results
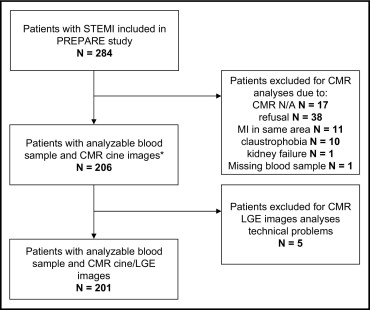
A total of 206 patients from the PREPARE study were included in the present analysis. The flow chart of the patients is shown in Figure 1 . As listed in Table 1 , more patients with an admission NT-pro-BNP level of ≥260 pg/ml had diabetes mellitus, but the overall incidence of diabetes was low. On univariate analysis, an admission NT-pro-BNP level of ≥260 pg/ml was associated with higher admission levels of CK-MB mass, cardiac troponin T, and high-sensitivity CRP. Patients with an admission NT-pro-BNP level of ≥260 pg/ml more often had anterior wall myocardial infarction compared to patients with an admission NT-pro-BNP level of <260 pg/ml.
| Variable | NT-pro-BNP ≥260 | NT-pro-BNP <260 | p Value |
|---|---|---|---|
| NT-pro-BNP on admission (pg/ml) | 688 (377–1,550) | 58 (14–108) | |
| Age (years) | 62 ± 11 | 58 ± 11 | 0.65 |
| Body surface area (m 2 ) | 2.0 ± 0.2 | 2.0 ± 0.2 | 0.95 |
| Men | 42 (81%) | 131 (85%) | 0.47 |
| History | |||
| Diabetes mellitus | 7 (14%) | 8 (5%) | 0.05 |
| Hypertension ⁎ | 12 (23%) | 34 (22%) | 0.88 |
| Hypercholesterolemia ⁎ | 6 (12%) | 20 (13%) | 0.79 |
| Myocardial infarction | 3 (6%) | 6 (4%) | 0.57 |
| Percutaneous coronary intervention | 1 (2%) | 7 (5%) | 0.40 |
| Cerebrovascular disease | 2 (4%) | 4 (3%) | 0.64 |
| Cardiovascular disease in family | 16 (31%) | 63 (41%) | 0.19 |
| Current smoker | 28 (54%) | 98 (64%) | 0.21 |
| Symptom onset to balloon (min) | 177 (131–270) | 156 (127–211) | 0.18 |
| Systolic blood pressure (mm Hg) | 137 ± 32 | 132 ± 26 | 0.59 |
| Diastolic blood pressure (mm Hg) | 79 ± 20 | 78 ± 16 | 0.52 |
| Heart rate (beats/min) | 77 ± 21 | 74 ± 20 | 0.32 |
| Infarct-related coronary artery | 0.001 | ||
| Left anterior descending | 27 (52%) | 33 (21%) | |
| Left circumflex | 7 (14%) | 16 (10%) | |
| Right | 18 (35%) | 105 (68%) | |
| Preprocedural TIMI flow | 0.64 | ||
| 0 | 47 (90%) | 144 (94%) | |
| 1 | 4 (8%) | 8 (5%) | |
| 2 | 1 (2%) | 2 (1%) | |
| Creatine kinase-MB on admission (μg/L) | 11.5 (5.6–20.5) | 4.5 (3.3–6.8) | <0.001 |
| Serum creatinine on admission (μmol/L) | 81 (63–92) | 74 (65–84) | 0.17 |
| Creatine clearance rate (ml/min) | 106 (77–133) | 108 (87–137) | 0.28 |
| Troponin T on admission (μg/L) | 0.12 (0.02–0.23) | 0.02 (0.02–0.036) | <0.001 |
| C-reactive protein on admission (mg/L) | 3.7 (1.9–8.4) | 2 (1.2–4.1) | 0.001 |
⁎ Hypertension and hypercholesterolemia defined as requiring prescription medication.
The CMR outcome data stratified by the admission NT-pro-BNP levels are listed in Table 2 . Patients with an admission NT-pro-BNP level of ≥260 pg/ml more often had a greater LV end-diastolic volume, a greater LV end-systolic volume, a lower LVEF, a larger infarct size, and a larger number of transmural segments. Because the test for interaction between infarct location and the effect of admission NT-pro-BNP on LVEF was significant (p <0.0001), we separately analyzed the effect of an admission NT-pro-BNP level of ≥260 pg/ml on LVEF in patients with anterior and nonanterior wall myocardial infarction. Overall, anterior wall myocardial infarctions were larger, with a larger number of transmural segments. No effect was found of an admission NT-pro-BNP level of ≥260 pg/ml on LVEF in patients with anterior wall myocardial infarction (absolute difference −3%, 95% confidence interval −11% to 5%; p = 0.32). However, in patients with nonanterior wall myocardial infarction and an admission NT-pro-BNP level of ≥260 pg/ml, the LVEF was 12% lower than in the patients with an admission NT-pro-BNP level of <260 pg/ml (95% confidence interval −20% to −4%; p <0.001). As listed in Table 3 , multivariate analysis revealed that an admission NT-pro-BNP level of ≥260 pg/ml was the strongest independent predictor of a lower LVEF among the serum biomarkers in patients with nonanterior wall myocardial infarction.
| Variable | All Patients | Anterior Wall Myocardial Infarction | Nonanterior Wall Myocardial Infarction | ||||||
|---|---|---|---|---|---|---|---|---|---|
| NT-pro-BNP ≥260 pg/ml (n = 52) | NT-pro-BNP <260 pg/ml (n = 154) | p Value | NT-pro-BNP ≥260 pg/ml (n = 27) | NT-pro-BNP <260 pg/ml (n = 33) | p Value | NT-pro-BNP ≥260 pg/ml (n = 25) | NT-pro-BNP <260 pg/ml (n = 121) | p Value | |
| N-terminal pro-brain natriuretic peptide (pg/ml) | 1,406 ± 2,413 | 71 ± 63 | <0.001 | 1,490 ± 1,832 | 79 ± 71 | <0.001 | 1,316 ± 2,954 | 68 ± 61 | <0.001 |
| Functional | |||||||||
| End-diastolic left ventricular mass (g/m 2 ) | 52 ± 13 | 45 ± 9 | 0.001 | 51 ± 12 | 47 ± 10 | 0.25 | 53 ± 14 | 45 ± 9 | 0.005 |
| Left ventricular end-diastolic volume (ml/m 2 ) | 110 ± 34 | 87 ± 21 | <0.001 | 110 ± 29 | 96 ± 29 | 0.04 | 110 ± 40 | 85 ± 17 | 0.001 |
| Left ventricular end-systolic volume (ml/m 2 ) | 66 ± 35 | 42 ± 18 | <0.001 | 65 ± 29 | 54 ± 23 | 0.11 | 68 ± 41 | 39 ± 15 | <0.001 |
| Left ventricular ejection fraction (%) | 43 ± 13 | 52 ± 9 | <0.001 | 43 ± 13 | 46 ± 8 | 0.32 | 42 ± 15 | 54 ± 9 | <0.001 |
| Late gadolinium enhancement | n = 50 | n = 151 | n = 27 | n = 33 | n = 23 | n = 118 | |||
| Infarct size (g/m 2 ) | 10 ± 8 | 5 ± 5 | <0.001 | 10 ± 7 | 9 ± 6 | 0.71 | 9 ± 8 | 4 ± 5 | 0.001 |
| No. of transmural segments (%) | 15 ± 14 | 6 ± 10 | <0.001 | 18 ± 14 | 17 ± 13 | 0.75 | 11 ± 13 | 3 ± 6 | 0.005 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


