Successful percutaneous coronary intervention (PCI) for chronic total occlusions (CTOs) has been associated with clinical benefit. There are no randomized controlled trials on long-term clinical outcomes after CTO PCI, limiting the available evidence to observational cohort studies. We sought to perform a weighted meta-analysis of the long-term outcomes of successful versus failed CTO PCI. A total of 25 studies, published from 1990 to 2014, with 28,486 patients (29,315 CTO PCI procedures) were included. We analyzed data on mortality, subsequent coronary artery bypass grafting (CABG), myocardial infarction, major adverse cardiac events, angina pectoris, stroke, and target vessel revascularization using random-effects models. Procedural success was 71% (range 51% to 87%). During a weighted mean follow-up of 3.11 years, compared with unsuccessful, successful CTO PCI was associated with lower mortality (odds ratio [OR] 0.52, 95% confidence interval [CI] 0.43 to 0.63), less residual angina (OR 0.38, 95% CI 0.24 to 0.60), lower risk for stroke (OR 0.72, 95% CI 0.60 to 0.88), less need for subsequent coronary artery bypass grafting (OR 0.18, 95% CI 0.14 to 0.22), and lower risk for major adverse cardiac events (0.59, 95% CI 0.44 to 0.79). There was no difference in the incidence of target vessel revascularization (OR 0.66, 95% CI 0.36 to 1.23) or myocardial infarction (OR 0.73, 95% CI 0.52 to 1.03). Outcomes were similar in patients who underwent balloon angioplasty only or stenting with bare metal or drug-eluting stents. Compared with failed procedures, successful CTO PCIs are associated with a lower risk of death, stroke, and coronary artery bypass grafting and less recurrent angina pectoris.
Although not proved in randomized controlled clinical trials, successful percutaneous coronary intervention (PCI) of chronic total occlusions (CTOs) can provide significant clinical benefit, such as reduction in angina pectoris, reduced need for coronary artery bypass grafting (CABG), improvement of left ventricular function, and possibly decreased risk for arrhythmias. The immediate procedural outcomes of CTO PCI have been improving: a meta-analysis including 18,061 patients from 65 studies demonstrated increasing success and decreasing complication rates over time. Recent studies report >90% success rates, even among challenging patients and lesion subgroups. The evidence on the clinical benefits of CTO PCI is limited to observational studies. The long-term outcomes of CTO PCI have been evaluated in 5 meta-analyses that demonstrated improved outcomes with successful versus failed procedures. However, these meta-analyses had important limitations, such as limited evaluation of the impact of various revascularization techniques, assessment of few clinical outcomes (mainly mortality), and noninclusion of some of the latest and largest studies. The goal of the present study was to perform a systematic review and weighted meta-analysis of all published studies on successful versus failed CTO PCI to better characterize the associated clinical outcomes.
Methods
We performed a comprehensive search of the Pubmed and Cochrane Library databases for manuscripts on coronary CTOs using the following keywords: “chronic total occlusion,” “percutaneous coronary intervention,” “stent,” “drug-eluting stents,” and “angioplasty.” Initially, no language or time limitations were applied; however, only studies in English and French were included in our meta-analysis. The references of those studies were checked for additional relevant studies as were subsequent articles citing each publication (cited reference search was performed using Web of Science, Thompson Reuters, New York, New York).
Human studies published from 1990 to August 2014 were included if they reported >6-month postprocedural outcomes in both successful and failed CTO PCI and included >40 patients. Procedural success was defined as successful CTO recanalization by any method (either retrograde and or antegrade) with achievement of ≤30% residual diameter stenosis within the treated segment and restoration of Thrombolysis In Myocardial Infarction grade 3 flow without the occurrence of a major adverse cardiac event (MACE).
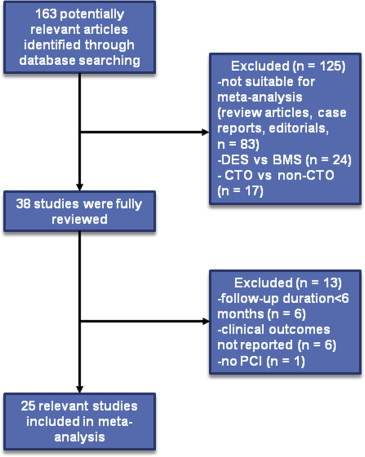
We did not apply any restrictions on CTO PCI techniques (e.g., retrograde approach) or on stent use; both stent and nonstent studies were included. The primary end point was all-cause death, but we also included several secondary end points: myocardial infarction (MI), CABG, target vessel revascularization (TVR), stroke, MACE (defined as composite of death, MI, and TVR), and residual/recurrent angina. Studies reporting only cardiac mortality and duplicate studies were excluded ( Figure 1 ).
Data collection, study selection, analysis of the data, and reporting of the results were performed according to the accepted principles on systematic reviews and meta-analyses.
Retrieved studies were reviewed by 2 investigators (GC and EB) using a standardized data collection form. In case of disagreement, a consensus was reached using a third reviewer (SB). Particular attention was given to study design, inclusion criteria, duration of follow-up, and primary and secondary end points. In studies reporting >6-month clinical outcomes, outcomes during the longest follow-up time were included in the analysis.
Extracted data included age, gender, number of patients, number of lesions, patient co-morbidities, including hypertension, diabetes, hyperlipidemia, smoking, previous CABG, PCI, and MI, CTO duration, target vessel, number and type of stents, procedural success, in-hospital complications, and the incidence of adverse clinical events during follow-up. The country of origin, the author, and the enrollment periods were reviewed to identify and exclude duplicate publications of the same CTO PCI cohort.
The absolute number of events was extracted from each study for each outcome of interest. If absolute numbers were not reported, the percentages of events were collected (from graphs in some studies) and converted to absolute number of events. Automatic “zero-cell” correction was used for studies with no events for a particular outcome. The pooled number of events for each outcome of interest was analyzed using a random-effects model. To assess heterogeneity across trials for each outcome, we used the Cochrane Q statistic (a p value <0.1 was considered significant) and the I 2 statistic (with ≤25% demonstrating low, >25% and <50% demonstrating moderate, and ≥75% demonstrating high heterogeneity). For all outcomes, odds ratios (ORs) with 95% confidence intervals (CIs) were reported. Publication bias was assessed through visual inspection of funnel plots (Begg’s method). All analyses were performed using Stats Direct (StatsDirect Ltd, Altrincham, United Kingdom).
Results
Of 163 publications retrieved through electronic search and reference checking, 25 observational studies were included in the final pooled analysis ( Table 1 , Figure 2 ). A total of 28,486 patients underwent 29,315 CTO PCI procedures: 20,778 were successful and 8,537 were unsuccessful, with no significant between-group differences in baseline demographics and risk factor profile. No randomized controlled trials were identified.
| Year | Author | Journal | Procedure dates | Type of intervention | Stents (DES,BMS) | DES (%) | BMS (%) | Number of patients | Follow-up duration | Procedural success |
|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | Finci | Am J Cardiol | n/a | PTCA | 0 | 0 | 0 | 200 | 2 | – |
| 1990 | Warren | Am Heart J | 1983 – 1988 | PTCA | 0 | 0 | 0 | 44 | 2.6 | – |
| 1992 | Ivanhoe | Circulation | 1980 – 1988 | PTCA | 0 | 0 | 0 | 480 | 4 | 69.2% |
| 1995 | Angioi | Arch Mal Coeur Vaiss | 1983 – 1991 | PTCA | 0 | 0 | 0 | 201 | 3.6 | 51% |
| 2000 | Noguchi | Cath Cardiovasc Interv | 1986 – 1996 | PTCA | 0 | 0 | 0 | 226 | 4.3 | 59.2% |
| 2001 | Suero | J Am Coll Cardiol | 1980 – 1999 | PTCA or BMS | 7 | 0 | 100% | 2007 | 7.6 | 69.9% |
| 2003 | Olivari | J Am Coll Cardiol | 1999 – 2000 | BMS | 89.70% | 0 | 100% | 376 | 1 | 73.3% |
| 2005 | Hoye | Eur Heart J | 1992 – 2002 | PTCA or BMS | 81% | 0 | 100% | 874 | 4.5 | 65.1% |
| 2006 | Drozd | Kardiol Pol | 1996 – 2003 | PTCA or BMS | NA | 0 | 100% | 459 | 2.5 | 64.9% |
| 2006 | Arslan | Int Heart J | 1999 – 2003 | PTCA or BMS | 91.50% | 0 | 100% | 304 | 2.6 | 68% |
| 2007 | Aziz | Cath Cardiovasc Interv | 2000 – 2004 | PTCA, BMS or DES | 97.70% | 17.3% | 82.7% | 543 | 1.7 | – |
| 2008 | Valenti | Eur Heart J | 2003 – 2006 | DES | 100% | 100% | 0 | 486 | 2 | 71% |
| 2008 | Labriolle | Am J Cardiol | 2003 – 2005 | PTCA, BMS or DES | 93.70% | 84% | 16% | 172 | 2 | – |
| 2009 | Chen | Chin Med J (Engl) | 2004 – 2005 | DES | 95.50% | 100% | 0 | 152 | 3 | 86.8% |
| 2011 | Lee | Cath Cardiovasc Interv | 2003 – 2006 | DES | 100% | 100% | 0 | 333 | 3.6 | 75.4% |
| 2011 | Mehran | JACC Cardiovasc Interv | 1998 – 2007 | PTCA or BMS or DES | 94.6% | 66% | 34% | 1791 | 2.9 | 68% |
| 2011 | Jolicoeur | Cath Cardiovasc Interv | 1999 – 2008 | PTCA or BMS or DES | 99.60% | 51.6% | 50.7% | 346 | 5.6 | 61.6% |
| 2011 | Yang | Int J Cardiol | 2005 – 2008 | DES | 100% | 100% | 0 | 136 | 2 | 64% |
| 2011 | Borgia | Int J Cardiol | 2003 – 2009 | DES | 100% | 98,2% | 1.8% | 302 | 4 | 78% |
| 2012 | Niccoli | Am J Cardiol | 2005 – 2009 | DES | 100% | 100% | 0 | 317 | 3 | 53.9% |
| 2012 | Jones | JACC Cardiovasc Interv | 2003 – 2010 | PTCA or BMS or DES | 97% | 76% | 24% | 836 | 3.8 | 69.6% |
| 2013 | George S | J Am Coll Cardiol | 2005 – 2009 | DES,BMS | 95.9% | 82.2% | 13.7% | 13443 | 2.65 | 70.6% |
| 2013 | Yamamoto | Am J Cardiol | 2005 – 2007 | PTCA,DES,BMS | – | 78% | 22% | 1524 | 3 | 78.2% |
| 2013 | Ciećwierz | Kardiol Pol | 2005 – 2007 | DES,BMS | 100% | – | – | 276 | 2 | – |
| 2014 | Kim | J Interv Cardiol | 2007 – 2009 | DES | 100% | 100 | 0 | 2658 | 2 | 79.6% |
The baseline demographic and angiographic characteristics of the study populations are summarized in Tables 1 and 2 . The most common CTO target vessel was the right coronary artery, followed by the left anterior descending and the left circumflex artery.
| Variable | Number of studies reporting factor | Successful CTO PCI n (%) | Failed CTO PCI n (%) |
|---|---|---|---|
| Total Patients | 24/25 | 10,579 (71.1%) | 4,297 (28.9) |
| Total CTO Lesions | 25/25 | 20,778 | 8,537 |
| Age (years, mean) | 25/25 | 60.4 | 61.9 |
| Men | 25/25 | 16,201/20,778 (78%) | 6,827/8,537 (80%) |
| Hypertension ∗ | 23/25 | 11,230/20,778 (54.1%) | 4,536/8,537 (53.1%) |
| Hyperlipidemia † | 21/25 | 10,660/20,778 (51.3%) | 4,537/8,537 (53.2%) |
| Smoking | 18/25 | 8,185/20,778 (39.4%) | 3,822/8,537 (44.8%) |
| Diabetes mellitus | 23/25 | 4,597/20,778 (22.1%) | 1,905/8,537 (22.3%) |
| Previous myocardial infarction | 24/25 | 7,845/20,778 (37.8%) | 3,723/8,537 (43.6%) |
| Previous PCI | 13/25 | 4,050/20,778 (19.5%) | 1,998/8,537 (23.4%) |
| Previous coronary bypass | 14/25 | 1,717/20,778 (8.3%) | 1,031/8,537 (12.1%) |
| CTO Target coronary artery (n=3,048) | |||
| Left anterior descending | 23/25 | 5,846/16,073 (36.4%) | 2,165/7,144 (30.3%) |
| Left circumflex | 22/25 | 3,352/16,073 (20.8%) | 1,335/7,144 (18.7%) |
| Right coronary | 22/25 | 6,875/16,073 (42.8%) | 3,638/7,144 (50.9%) |
| CTO duration (months) | |||
| Less than 3 | 7/25 | – | – |
| Greater than 3 | 14/25 | – | – |
| Unknown Duration | 4/25 | – | – |
| Major in-hospital complications | |||
| Death | 14/25 | 48/6,142 (0.8%) | 46/2,482 (1.9%) |
| Q-wave myocardial infarction | 13/25 | 64/5,757 (1.1%) | 28/2,284 (1.2%) |
| Emergent coronary bypass | 11/25 | 27/4,134 (0.7%) | 48/1,740 (2.8%) |
∗ Defined as blood pressure of >140/90 mm Hg or >130/80 mm Hg in patients with diabetes mellitus or use of antihypertensive medications.
† Hyperlipidemia was defined as low density cholesterol >100 mg/ml or use of antilipidemic medications.
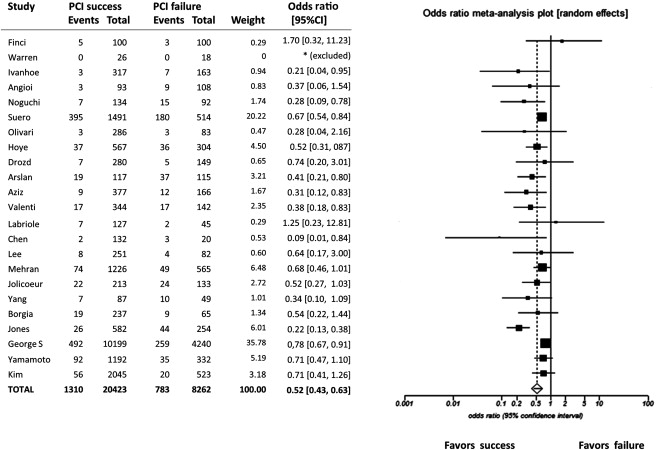
Mean follow-up time was 3.11 years (range 6 months to 12 years). Mortality was reported in 23 of 25 studies. As shown in Figure 2 , compared with failed CTO-PCI, successful procedures were associated with lower mortality (OR 0.52, 95% CI 0.43 to 0.63, chi-square = 42.85, p <0.0001; I 2 = 54.6%, 95% CI 17.7 to 70.9).
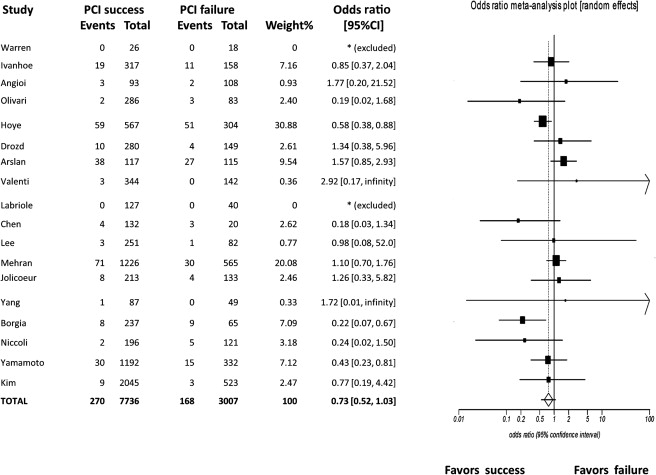
Myocardial infarction was reported in 18 studies. As shown in Figure 3 , compared with failed CTO-PCI, successful procedures reduced the risk of MI (OR 0.73, 95% CI 0.52 to 1.03; chi-square = 3.17, p = 0.08; I 2 = 47.7%, 95% CI 0 to 69.4; Figure 3 ).
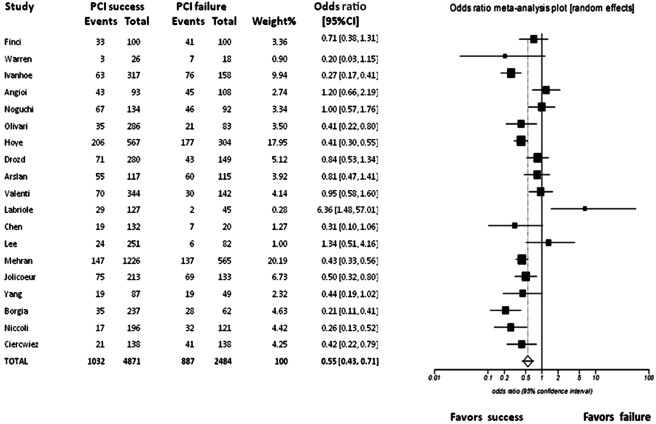
The incidence of MACE was reported in 19 studies. As shown in Figure 4 , successful CTO-PCI reduced the risk of MACE compared with failed procedures (OR 0.55, 95% CI 0.43 to 0.71; chi-square = 21.06, p <0.0001; I 2 = 76%, 95% CI 60.9 to 83.6, consistent with high heterogeneity; Figure 4 ).
Long-term angina status was reported in 9 studies. As shown in Figure 5 , successful CTO-PCI reduced the risk of residual angina (OR 0.38, 95% CI 0.24 to 0.60; chi-square = 17.10, p <0.0001; I 2 = 81.4%, 95% CI 62.8 to 88.6; Figure 5 ).
The subsequent need for coronary artery bypass grafting (CABG) was reported in 19 studies. As shown in Figure 6 , successful CTO-PCI was associated with a significantly lower risk of CABG (OR 0.18, 95% CI 0.14 to 0.22; chi-square = 239.02, p <0.0001; I 2 = 38.9%, 95% CI 0.0 to 63.6; Figure 6 ).
Stroke was reported in 5 studies. As shown in Figure 7 , successful CTO-PCI was associated with a significantly lower risk of stroke (OR 0.72, 95% CI 0.60 to 0.88; chi-square = 10.83, p = 0.001; I 2 = 0%, 95% CI 0.0 to 64.1; Figure 7 ).
TVR was reported in 5 studies, without significant difference between successful and failed procedures (OR 0.66; 95% CI 0.36 to 1.23; chi-square = 1.72, p = 0.190; I 2 = 57.2%, 95% CI 0.0 to 82.0; Figure 8 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


