Studies in victims of sudden cardiac death and those surviving a cardiac arrest have confirmed that extent of coronary artery disease is similar in those with and without angina, suggesting that it is the presence of myocardial ischemia rather than associated symptoms that determine the prognosis. Experimental models show that hypoxic myocardial tissue results in production of extra B-type natriuretic peptide (BNP), suggesting that BNP could potentially serve as a biomarker of myocardial ischemia. We performed a meta-analysis of the studies that link BNP to inducible myocardial ischemia as indicated by noninvasive stress tests. Values of true positive, false positive, true negative, and false negative were calculated from the reported sensitivity, specificity, disease prevalence, and total number of patients studied. Sixteen studies reporting data on 2,784 patients across 14 study populations were included in the final analysis. Mean age of participants was 55 to 69 years and 55% to 90% were men. Pooled sensitivity and specificity of BNP for detection of stress-induced myocardial ischemia were 71% (95% confidence interval [CI] 68 to 74) and 52% (95% CI 52 to 54), respectively. Pooled diagnostic odds ratio was 3.5 (95% CI 2.46 to 5.04) and summary receiver operating characteristic curve revealed an area under the curve of 0.71 ± 0.02 (mean ± SE). In conclusion, this meta-analysis suggests that an increased BNP level can identify inducible ischemia as detected by standard noninvasive stress tests. This raises the possibility of a whole new role for BNP in the diagnosis and management of myocardial ischemia.
B-type natriuretic peptide (BNP) has been studied extensively in the diagnosis and exclusion of left ventricular (LV) systolic dysfunction (SD). The high negative predictive value of BNP in this particular scenario has led to it being used in day-to-day clinical practice as a “rule-out test” to exclude the presence of LVSD. However, BNP also has the potential to be useful in other patient populations that do not have heart failure or LVSD, albeit at much lower levels than those used to identify LVSD. Increased BNP values (typically 100 ≥pg/ml) are used to detect LVSD but BNP values in the lower range (10 to 20 pg/mL) are of independent prognostic value over and above a wide range of echocardiographic abnormalities including LV dysfunction and LV hypertrophy. The question that naturally arises is why BNP identifies a poor prognosis in so many populations irrespective of LV function and other echocardiographic abnormalities. One possible answer is that BNP identifies myocardial ischemia itself. Studies have shown that transcription and release of BNP are affected by oxygen tension, and hypoxia as a trigger for the release of BNP has been demonstrated in experimental models. Thus, it seems that repeated episodes of ischemia, silent or symptomatic, may stimulate BNP formation and that BNP can be used to identify those patients who have underlying myocardial ischemia. Indeed, many small clinical studies have suggested that this is true. To examine this question, we therefore performed a meta-analysis of the studies that link BNP to inducible myocardial ischemia as indicated by noninvasive stress tests.
Methods
We conducted a meta-analysis based on a prespecified protocol that was devised according to guidelines of the Cochrane Collaboration. Studies were eligible if they compared BNP or N-terminal pro-BNP (NT–pro-BNP) to evidence of inducible ischemia from a noninvasive stress test (stress echocardiography or myocardial perfusion imaging with single-photon emission computed tomography) in patients with known or suspected coronary artery disease (CAD). The other minimum requirement to be included in our meta-analysis was the availability of enough information to complete a 2 × 2 contingency table. Studies using BNP as a prognostic rather than a diagnostic marker, those testing BNP in acute coronary syndromes, and studies where the reference test was not a noninvasive stress test for myocardial ischemia were excluded. We did not include studies where treadmill electrocardiography alone was used as a reference standard because of its known poor sensitivity and specificity to diagnose inducible myocardial ischemia. On occasions when several published studies reported data from a single patient group, we selected the most complete or most recent version. When a study reported numerous cutoffs, we used the one with best combination of the reported sensitivity and specificity.
We searched MEDLINE, EMBASE, the Cochrane Database, and CINAHL from the earliest date in 1966 to September 2009. Gray literature was sought using the Google search engine. In addition, we hand-searched references listed in the original studies and previous review articles to identify other potentially eligible studies. No language restrictions were imposed. Search terms used included “natriuretic peptides,” “BNP,” “amino terminal pro brain natriuretic peptide” and “NT–pro-BNP” combined with “myocardial ischemia/ischemia,” “coronary artery disease,” and “ischemic/ischemic heart disease.” When necessary we also attempted to contact study authors for further information to complete data abstraction from the potentially eligible studies. Two reviewers (M.A.N. and M.D.W.) independently examined titles and abstracts of all potentially relevant studies. Full articles were obtained from all citations meeting prespecified selection criteria. Data were abstracted by 2 reviewers (M.A.N. and B.R.S.) independently using a standard ProForma and discrepancies were resolved by consensus. We abstracted data on study characteristics, methods, and final results from each selected article. Study characteristics included study settings and type of population examined (including age, gender, and reported disease prevalence in study population), year of publication, assay type and cutoff of index test, reference test standards, and source of funding (industry vs nonindustry). Quality was assessed by the QUADAS tool with particular emphasis on blinding procedures during interpretation of index and reference tests for each study. QUADAS is an evidence-based tool used for quality assessment of diagnostic accuracy studies. It consists of 14 items phrased as questions, each of which should be scored a “yes”, “no,” or “unclear,” that examine bias in a study. Published data suggest that a study with a score 7 to ≥10 is considered high quality. For this analysis we used a minimum score of 10 as an indicator of good quality.
For all studies included in the review a 2 × 2 contingency table was constructed. Values of true positives, false positives, true negatives, and false negatives were deduced from reported sensitivity, specificity, disease prevalence, and total number of patients studied. Where the published information was insufficient or unclear to construct a 2 × 2 table we requested missing data from the respective corresponding author. We used Meta-Disc 1.4 (Clinical Biostatistics, Ramón y Cajal Hospital, Madrid, Spain) to perform all statistical analyses. This is a publically accessible statistical software package designed purposefully for meta-analysis of diagnostic accuracy and has previously been used in several meta-analyses. Pooled sensitivities, specificities, positive and negative likelihood ratios, and diagnostic odds ratios were calculated using the DerSimonian-Liard method. We calculated the I 2 statistic to assess heterogeneity between studies. An I 2 value >25% was considered to represent significant heterogeneity. Although random and fixed effect models were used, owing to significant heterogeneity we reported only results from random effect models. A summary receiver operating characteristic curve was constructed from pooled data for studies included in the final analysis. Subgroup analyses were performed to explore the significant heterogeneity observed. First, we compared studies with BNP to those with NT–pro-BNP. Second, we reanalyzed the data by including results from studies that explicitly excluded patients with decreased ejection fraction or known heart failure. Third, we pooled data separately for studies using BNP levels after stress. Random effects meta-regression (inverse variance weights) was used to explore sources of variation. Mean age of study population, disease prevalence, exclusion of heart failure, timing of BNP measurement, and blinding of test results were considered variables. We also investigated whether type of reference test and type (BNP or NT–pro-BNP) and timing (before or after stress) of NP measured influenced the results.
Results
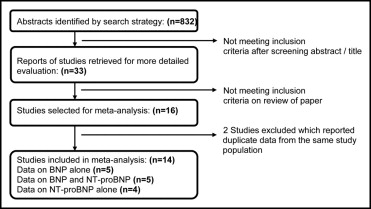
The initial search strategy identified 832 citations. Examination of titles and abstracts of these citations identified 33 articles for detailed evaluation. After detailed evaluation 20 studies met inclusion criteria ( Figure 1 ). Reasons for exclusion included no reference test or the reference test not being a stress test. Where not enough information was available to complete 2 × 2 tables, a request was made to the corresponding study author to provide the missing data. We were unable to obtain further data on 4 studies and hence could not include these in the final analysis. Sixteen studies reporting data on 2,784 patients across 14 study populations were included in the final analysis. Table 1 presents key characteristics of the included studies. All studies reported a prospective design and all studies except 1 declared blind interpretation of test results. All but 4 studies reported consecutive enrollment. The reference test was applied equally in all study participants. In 11 studies myocardial perfusion imaging with single-photon emission computed tomography (using exercise or dipyridamole as the stressor) was the reference test to confirm stress-induced ischemia, whereas in 3 studies stress echocardiography (using exercise or dobutamine as the stressor) provided the reference standard. The QUADAS score was 10 to 14 (mean score 11). All studies scored ≥10 indicating that all studies included in the meta-analysis were of good quality.
| Study | Year Published | Study Population | Total Number of Subjects | Mean Age | Men (%) | Prevalence of Ischemia (%) |
|---|---|---|---|---|---|---|
| Sabatine et al | 2004 | patients undergoing exercise MPI-SPECT for evaluation of chest pain or ischemia | 112 | 63 | 78% | 50% |
| Palumbo et al | 2004 | patients with known CAD referred for exercise MPI-SPECT in tertiary center for evaluation of ischemia | 100 | 59 | 80% | 70% |
| Foote et al | 2004 | patients with known CAD referred for exercise MPI-SPECT in tertiary center | 74 | 59 | 85% | 54% |
| Asada et al | 2004 | patients undergoing dobutamine echocardiography for evaluation of ischemia | 317 | 68 | 55% | 9% |
| Win et al | 2005 | patient undergoing exercise MPI-SPECT for evaluation of chest pain or ischemia | 60 | 58 | 80% | 16% |
| Zaid et al | 2006 | patient undergoing exercise MPI-SPECT for evaluation of chest pain | 203 | 59 | 66% | 62% |
| Conen et al | 2006 | consecutive patients referred for exercise echocardiography with rapid access to angiography | 62 | 67 | 100% | 24% |
| Staub et al | 2006 | consecutive patients referred for exercise MPI-SPECT for evaluation of chest pain or ischemia | 260 | 63 | 70% | 48% |
| Wong et al | 2006 | asymptomatic patients with stroke who underwent dipyridamole MPI-SPECT | 56 | 68 | 69% | 55% |
| Vanzetto et al | 2007 | patients with known CAD referred for exercise MPI-SPECT in tertiary center | 102 | 61 | 88% | 55% |
| Karabinos et al | 2007 | patient undergoing dobutamine echocardiography | 128 | 55 | 72% | 28% |
| Kurz et al | 2007 | patients undergoing exercise or dipyridamole MPI-SPECT | 86 | 68 | 58% | 28% |
| Cosson et al | 2009 | asymptomatic diabetics undergoing exercise or dipyridamole MPI-SPECT | 323 | 59 | 57% | 33% |
| Heart and Soul Study | 2009 | patients with stable CAD undergoing exercise echocardiography for evaluation of ischemia | 901 | 69 | 90% | 25% |
Study populations and settings were heterogenous ( Table 1 ). Although most studies included patients with and without known CAD, 4 studies restricted recruitment to patients with known CAD only. Two studies were performed in asymptomatic but high-risk patients (stroke survivors and patients with diabetes and ≥1 other cardiovascular risk factor ). Mean age of participants was 55 to 69 years; 55% to 100% of study subjects were men. Prevalence of inducible myocardial ischemia was 9% to 70%. Five studies reported data on BNP alone, whereas 4 studies measured NT–pro-BNP only. In 5 studies data on BNP and NT–pro-BNP were available. Timing of measurement varied at baseline, peak stress, and after stress. Similarly, a wide range of threshold levels was reported ( Table 2 ).
| Study | Assay Manufacturer | Thresholds (pg/ml) | ||
|---|---|---|---|---|
| Timing | BNP | NT-pro-BNP | ||
| Sabatine et al | Biosite Diagnostics, Elecys, Roche Diagnostics | baseline | — | — |
| after stress | 80 | — | ||
| change ⁎ | 10 | — | ||
| Palumbo et al | Shionoria-BNP, CIS Bio International-Shering | baseline | 15 | — |
| after stress | — | — | ||
| change | — | — | ||
| Foote et al | Biosite Diagnostics, Elecys, Roche Diagnostics | baseline | — | — |
| after stress | — | — | ||
| change | 12 | 8 | ||
| Asada et al | Shionoria-BNP, Shionogi and Co. | baseline | 18 | — |
| after stress | — | — | ||
| change | — | — | ||
| Win et al | Biosite Diagnostics | baseline | — | — |
| after stress | — | — | ||
| change | 10% | — | ||
| Zaid et al | AxSYM, Axis Shield Diagnostics | baseline | 36 | — |
| after stress | 48 | — | ||
| change | 7 | — | ||
| Conen et al | Biosite Diagnostics, Elecys, Roche Diagnostics | baseline | 18 | 59 |
| after stress | 26 | 66 | ||
| change | — | — | ||
| Staub et al | AxSYM, Abbot Laboratories, Elecys, Roche Diagnostics | baseline | 90 | 229 |
| after stress | 110 | 247 | ||
| change | 22 | 19 | ||
| Wong et al | RIA, Bachem, Ltd. | baseline | 11 | — |
| after stress | — | — | ||
| change | — | — | ||
| Vanzetto et al | Elecys, Roche Diagnostics | baseline | — | 104 |
| after stress | — | — | ||
| change | — | — | ||
| Karabinos et al | Elecys, Roche Diagnostics | baseline | — | 153 |
| after stress | — | 172 | ||
| change | — | — | ||
| Kurz et al | Elecys, Roche Diagnostics | baseline | — | — |
| after stress | — | 125 | ||
| change | — | — | ||
| Cosson et al | Dade Behring | baseline | 15 | — |
| after stress | — | — | ||
| change | — | — | ||
| Heart and Soul Study | Biosite Diagnostics, Elecys, Roche Diagnostics | baseline | 18 | 100 |
| after stress | — | — | ||
| change | — | — | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


