Mesothelioma of the Pleura
Allen P. Burke, M.D.
Terminology
The majority of mesothelial neoplasms of the pleura are malignant mesotheliomas. To distinguish the typical diffuse form from the rare localized form, the modifier “diffuse” is often placed before “malignant mesothelioma.” Low-grade or benign mesothelial neoplasms, which are relatively more common in the peritoneum and exceedingly rare in the pleura, include “well-differentiated papillary” and “multicystic mesotheliomas” and are considered separately.
The most important prognostic pathologic feature is the presence of sarcomatoid differentiation. For this reason, the diagnosis should always include the amount of sarcomatoid change or specifically indicate its absence.
Diffuse Malignant Mesothelioma
Epidemiology
Although they may occur in children, the vast majority of pleural mesotheliomas are seen in adults, usually over 60 years at the time of diagnosis. There is a male predominance of about 4:1. In North America, the rate in men is 23 cases per million per year. Mesotheliomas account for only 1% of malignant pleural effusions.1
Asbestos Exposure
In North America, up to 80% to 90% of mesotheliomas in men are related to asbestos exposure. The link between asbestosis and mesothelioma is weaker in women, who account for a relatively small proportion of cases.2
Of the types of asbestos, amphibole asbestos (amosite and crocidolite) is two to three orders of magnitude more carcinogenic than is chrysotile asbestos. It has been proposed that contamination of chrysotile by the amphibole fiber tremolite accounts for its carcinogenicity.3
The most common thoracic manifestation of asbestos exposure is the pleural plaque, which increases the risk for the development of mesothelioma by nine times over the general population (See Chapter 56).4
Erionite Exposure
Erionite is a type of zeolite, a nonasbestos fiber that has similar commercial properties as amphibole asbestos. In the Cappadocia region of Turkey, where there is nonindustrial exposure to erionite-containing rock, the incidence of mesothelioma is extraordinarily high.3
Other Risk Factors
Other risk factors for the development of pleural mesotheliomas include radiation and genetics (BAP1 germline mutations).
Clinical Findings
The manifestations of pleural mesotheliomas are usually related to pleural effusions. Systemic symptoms such as weight loss and fever are common. Because the tumors are initially relatively slow growing, patients can be asymptomatic for a prolonged period, and effusions may be initially diagnosed as negative, because of the low sensitivity of cytologic diagnosis.5
Radiologic Findings
Mesotheliomas manifest on imaging as pleural effusions, often with nodules or plaques.
Computed tomography effectively demonstrates the extent of primary tumor, intrathoracic lymphadenopathy, and extrathoracic spread. Thoracic magnetic resonance imaging is particularly useful for identifying invasion of the chest wall, mediastinum, and diaphragm. Positron emission tomography can accurately demonstrate intrathoracic and extrathoracic lymphadenopathy and metastatic disease.6
Spread of Disease
The initial spread of mesothelioma is over the parietal pleural surfaces, the typical site of pleural plaques, with direct extension to the visceral pleura, interlobar fissures, and subsequently the chest wall, lung parenchyma, and surrounding structures. Lymphatic dissemination is unusual, and more common in the epithelioid histologic type.
Approximately 10% of pleural mesotheliomas are associated with peritoneal mesotheliomas.
Distant hematogenous metastases are common in late-stage disease, including unusual sites such as soft tissue of the extremities and even gingiva.7,8 Autopsies of patients dying with pleural mesothelioma show extrapleural dissemination in almost 90% patients, with tumor spread to lymph nodes in 53%, followed by liver (32%), spleen (11%), thyroid (7%), and brain (3%).9
Pathologic Staging
Accurate pathologic staging can be difficult on video-assisted thoracic biopsies. Pathologic T1 stage indicates ipsilateral parietal involvement with (1b) or without (1a) visceral involvement. Pathologic stage T2 adds confluent visceral pleural tumor including fissure, diaphragm, or lung parenchyma. Pathologic stage T3 involves endothoracic fascia, mediastinal fat, chest wall, or nontransmural pericardium. Pathologic stage T4 indicates any of the following: multifocal soft tissue spread, rib involvement, transmural diaphragmatic spread, transmural pericardial involvement or heart involvement, positive pericardial cytology, esophageal invasion, contralateral pleura involvement, spinal involvement, or invasion of the brachial plexus.
Gross Findings
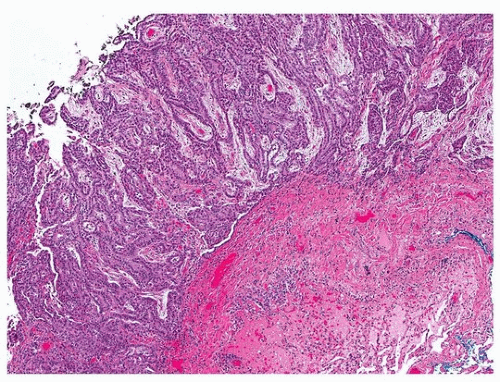
Pleural mesotheliomas cause confluent nodules and masses on the parietal and visceral surfaces, usually obliterating the pleural space and interlobar fissures, eventually encasing the lung (Fig. 97.1). In late stages, the pleura may be several centimeters thick. The consistency
varies according to histologic type; epithelioid tumors are gray-white and soft, often with softer cystic areas containing mucoid-like material. Sarcomatoid tumors are more likely firm, with the appearance of fibromatosis or sarcoma.
varies according to histologic type; epithelioid tumors are gray-white and soft, often with softer cystic areas containing mucoid-like material. Sarcomatoid tumors are more likely firm, with the appearance of fibromatosis or sarcoma.
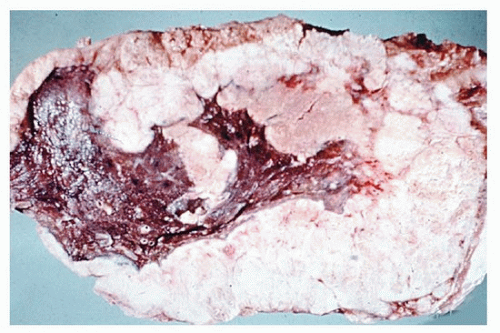 FIGURE 97.1 ▲ Pleural diffuse malignant mesothelioma, gross findings. There is an irregular white-tan tumor encasing the lung. |
Malignant mesothelioma is rarely entirely intraparenchymal, forming miliary nodules.10
Epithelioid Mesothelioma, Histologic Findings
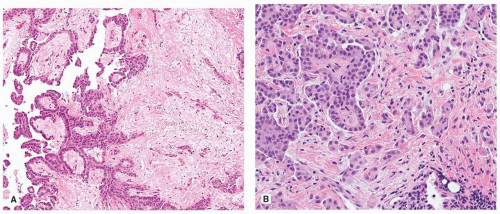
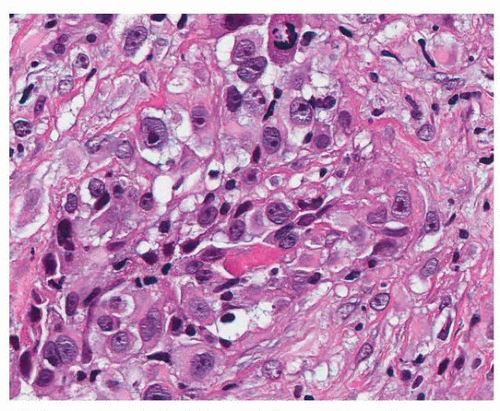
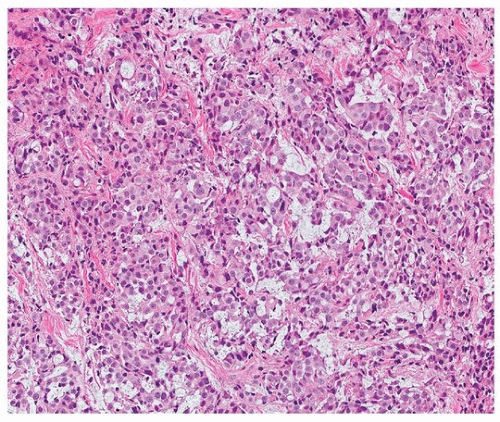
The common pattern of growth is tubulopapillary, with anastomosing papillary projects on the pleural surface that form tubules in the stroma (Figs. 97.2 and 97.3). There are frequently solid areas that are associated with nuclear pleomorphism and mitotic activity (Fig. 97.4). Tumor infiltrating into stroma, fat, fascia, muscle, and lung parenchyma represents progressive invasive growth (Fig. 97.5).
A large variety of growth patterns, in addition to tubulopapillary and solid, have been described, but there is little impact on immunohistochemical results, and they are usually intermixed with more typical mesothelioma. These include trabecular, micropapillary, nested, adenomatoid (microcystic), clear cell, and signet ring patterns.11,12,13,14 The trabecular or nested growth patterns can often have an “endocrine” appearance.
It is not uncommon to have, in the solid growth pattern, areas of tumor with abundant pink cytoplasm resembling decidua; there are no strict criteria for this designation, however.15 Similar to the deciduoid growth pattern are tumor cells with rhabdoid features.11
Malignant mesothelioma with a heavy lymphoid infiltrate obscuring the polygonal neoplastic cells can mimic malignant lymphoma or lymphoepithelioma-like carcinoma and is sometimes designated “lymphohistiocytoid mesothelioma.”16 A clear distinction from more typical mesotheliomas that have a lymphocytic response is not always possible.
A myxoid background is common in the papillary structures and is conspicuous in 5% to 10% of cases (Fig. 97.6A). Rarely, tumor nests or papillae may be seen floating in a myxoid matrix, simulating mucinous carcinoma, with nests of cytologically bland, often vacuolated epithelioid cells (Fig. 97.6B).
One subset of mesotheliomas is intermediate between epithelioid and sarcomatoid mesothelioma. So-called pleomorphic mesotheliomas resemble sarcomas, with large, discohesive cells that vary in size and shape, have abundant cytoplasm and irregular nuclei, usually have prominent nucleoli, and have all characteristics of “sarcomatoid” mesothelioma except cellular spindling. Most often, these tumors show areas of sarcomatoid differentiation and are thus designated biphasic, although rare examples of pure “pleomorphic” types have been described, in the absence of significant cellular elongation. It is likely that these tumors should be best considered sarcomatoid, because the prognosis is similar.17
Biphasic and Sarcomatoid Mesothelioma, Histologic Findings
Diffuse biphasic malignant mesothelioma is a mesothelioma showing at least 10% each of epithelioid and sarcomatoid patterns. Because there may be areas of pleomorphism without cellular and nuclear spindling, the distinction is not always precise.
Sarcomatoid mesotheliomas account for <10%, biphasic for 10% to 15%, and desmoplastic for <2% of all mesotheliomas in most series.3 In the United Kingdom, a rate of nearly double that has been reported for biphasic and sarcomatoid mesotheliomas.18
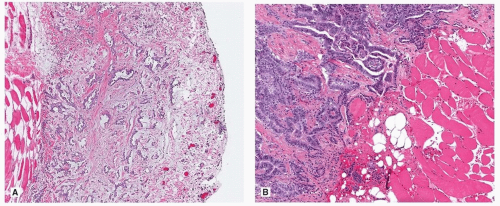
Spindled cells arranged in fascicles or haphazard arrays characterize sarcomatoid mesotheliomas (Fig. 97.7). They often are higher-stage tumors, involving the adipose tissue of the parietal pleura, or extend into the adjacent lung parenchyma.
Mesothelioma with heterologous elements is rare. Types of sarcoma are most often osteosarcoma, followed by chondrosarcoma (often mixed with osteosarcoma) and rhabdomyosarcoma.19
Desmoplastic Mesothelioma
A subset of sarcomatoid is the “desmoplastic” mesothelioma, which is characterized by dense collagenized tissue with few interspersed malignant cells. The term is used if more than one-half of the tumor is composed of the desmoplastic pattern. The collagen background lacks the loose fibrosis that is typical of a “desmoplastic reaction,” which can occur in otherwise typical mesotheliomas and which occurs frequently in carcinomas.
The importance to the recognition of desmoplastic mesothelioma, which has a poor prognosis similar to that of other sarcomatoid mesotheliomas, lies in the difficulty making the diagnosis, especially in small biopsies. Invasion into fat is the only reliable criterion for diagnosis; other helpful criteria include bland necrosis and areas of typical sarcomatoid mesothelioma (Fig. 97.8).
Mucin Stains
The mucin that is elaborated by mesothelioma is positive for Alcian blue and sensitive to hyaluronidase. Neutral mucin is not usually present, as evidenced by mucicarmine stain of periodic acid-Schiff with diastase, but exceptions make these stains of little general use in the differential diagnosis between mesothelioma and carcinoma.
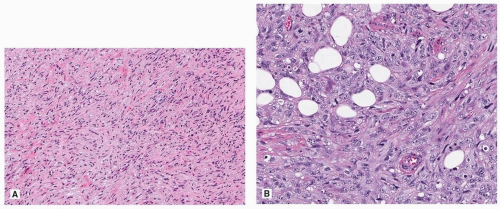 FIGURE 97.7 ▲ Sarcomatoid mesothelioma. A. The tumors are spindled, with relatively mild pleomorphism. B. In this example, there is more pleomorphism and less spindling (overlap with pleomorphic mesothelioma).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|