Chapter 154
Mesenteric Vascular Disease
Venous Thrombosis
Stefan Acosta, Martin Björck
Splanchnic venous thrombosis can occur within the portal, superior and inferior mesenteric, and splenic veins. Mesenteric venous thrombosis (MVT) is defined as thrombosis within the superior mesenteric vein with or without extension to the portal or splenic vein. Recovery following resection of infarcted intestine secondary to mesenteric vessel occlusion was first reported by Elliot in 1895.1 MVT was recognized as an entity distinct from mesenteric arterial occlusion by Warren and Eberhard in 1935.2
Epidemiology
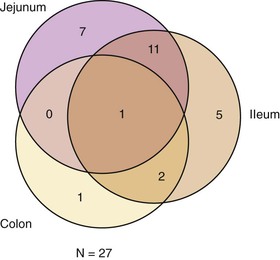
MVT is most commonly encountered in middle-aged and older adult patients, with an equal gender distribution.3,4 In a population-based study with an average autopsy rate of 87%, MVT was found to be present in 63 of 402 patients (16%) with acute mesenteric ischemia (Fig. 154-1).5,6 Additionally, the overall incidence of MVT with transmural intestinal infarction was estimated to be 1.8 per 100,000 person-years in Malmö, Sweden, between 1970 and 1982, and the cause-specific mortality ratio was 0.9 per 1000 autopsies.5 The overall incidence of MVT increased to 2.7 per 100,000 person-years in the same city between 2000 and 2006.4 An important factor contributing to a decrease in the incidence estimate was the declining autopsy rate, from 87% to 10%, between the two periods. In contrast, factors increasing the incidence estimate over time were the growing proportion of older adults in the population and the greater diagnostic activity and quality. Patients with MVT were diagnosed at autopsy, at operation, or with computed tomography (CT) in 12% (6 of 51), 19% (10 of 51), and 69% (35 of 51) of cases, respectively,4 during the latter period.
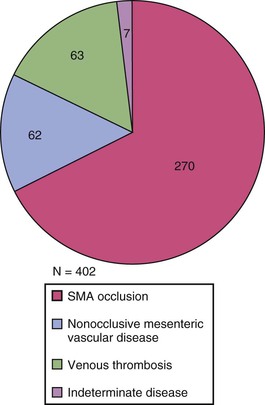
Figure 154-1 Acute mesenteric ischemia: distribution of etiologies in 402 patients in Malmö, Sweden, between 1970 and 1982.4,5 MVT, acute SMA occlusion (embolus/thrombus ratio = 1.4), and nonocclusive mesenteric ischemia were found in 16%, 68% and 16%, respectively. SMA, Superior mesenteric artery.
Pathogenesis
Etiology
Primary MVT is defined as spontaneous, idiopathic thrombosis of the mesenteric veins not associated with any other disease or etiologic factor. Patients with any condition known to predispose to MVT (Box 154-1) are considered to have secondary MVT.7 Approximately 90% of MVTs are secondary.8
Risk Factors
Several conditions are associated with MVT (see Box 154-1), and these can be divided into three main categories: direct injury, local venous congestion or stasis, and thrombophilia. Splenectomy is a risk factor for the development of thrombus propagation from the ligated splenic vein to the portomesenteric venous system.9 Inflammatory states such as inflammatory bowel disease may lead to peripheral vein thrombosis in the mesentery propagating to central parts of the SMV,10 and severe acute pancreatitis may lead to MVT but more frequently to splenic vein thrombosis due to its very close proximity to the inflamed pancreas.11,12 Obesity was found to be a risk factor in case-control study.5 Inherited thrombophilia13–16 has been reported in 42% (13 of 31)3 to 55% (16 of 29)4 of patients with MVT. Factor V Leiden mutation (activated protein C resistance) was present in 45% of the patients with MVT in Malmö, Sweden,4 which was considerably higher than the known prevalence rate of 7% in the background population.17 Although factor V Leiden mutation is a genetic defect, peripheral venous thrombotic manifestations are frequently delayed until adulthood, even in homozygotes.17,18 MVT has been reported to be a common first clinical manifestation of patients with newly diagnosed myeloproliferative disorders such as polycythemia vera or essential thrombocytosis and often occurs before a rise in peripheral blood counts. The JAK2 V617F (Janus-activated kinase gain-of-function substitute of valine to phenylalanine at position 617) mutation is diagnostic of myeloproliferative disorders.19 Primary cytomegalovirus infection has also been associated with MVT.20,21 Neither liver cirrhosis nor abdominal cancer was a risk factor in a population-based case-control study based on autopsies.5 Synchronous venous thromboembolism in the systemic circulation occurs frequently in patients with MVT, especially pulmonary embolism.5 There may be an increased risk of MVT following laparoscopic surgery because of venous stasis from increased intra-abdominal pressure, especially in obese patients undergoing Roux-en-Y bypasses, or when there is a more extensive intraoperative mobilization of the mesenteric, portal or splenic vein, and together with the presence of any systemic thrombophilic state, development of MVT seems to be more likely.22,23
Natural History
It is difficult to pinpoint the natural history of MVT. The disease is uncommon, patients often have diffuse symptoms, and the condition is not always detected, even with contemporary diagnostic routines. Thus we have no absolute knowledge of the total number of patients with symptomatic and asymptomatic disease. However, in a population-based study with a high autopsy rate (87%), it was found that 35 of 31,015 patients (0.1%) examined postmortem had MVT.5 The majority of patients with MVT at autopsy (27 of 35, or 77%) had a transmural intestinal infarction, judged to be the cause of death. The patients diagnosed at exploratory laparotomy all had transmural intestinal infarction and required bowel resection for survival. The mortality rate among those undergoing exploratory laparotomy was 30% (12/40). Portal venous thrombosis (PVT) was studied in the same cohort, and there were some interesting differences: PVT was 10 times more common than MVT at autopsy, patients with PVT more often had asymptomatic disease, and PVT was seldom considered the cause of death.24 Two studies25,26 suggest that superior MVT, in contrast to isolated PVT, is associated with symptoms in the overwhelmingly majority (92%25) of cases and also often results in bowel gangrene (33%26-45%25) depending on diagnostic and therapeutic activity. CT imaging, in comparison with autopsy and exploratory laparotomy, diagnosed most patients (69%)4 with MVT between 2000 and 2006.
Pathology and Manifestations
The degree of intestinal ischemia that develops depends on the extent of venous thrombosis within the splanchnic venous circulation and whether there is occlusion and collateral flow. Patients with isolated PVT without peripheral propagation to the superior mesenteric vein are asymptomatic in the majority of cases (61%25) and almost never experience intestinal infarction (0%25-10%26).24,26 In 270 patients with portomesenteric venous thrombosis found at autopsy, 29 of 31 (94%) patients with MVT had intestinal infarction and 0 of 239 (0%) with isolated PVT had intestinal infarction.26
At operation, MVT is characterized by a limited segment of intestinal ischemia, with edema, swelling, and reddish discoloration of the affected small bowel and its adjacent mesentery and a palpable pulse in the superior mesenteric artery (SMA) and its branches.27 In contrast, intestinal ischemia due to arterial occlusive or nonocclusive disease is often characterized by extensive ischemia that includes the jejunum, ileum, and colon,28 with patchy cyanosis, reddish black discoloration, and no palpable pulsations. MVT can be confirmed during surgery if an infarcted bowel segment is removed. Division of a small part of the adjacent mesentery, without previous vessel ligation, reveals thrombosis within the veins, whereas a pulsatile hemorrhage arises from the arteries. The extent of intestinal infarction is often limited to the jejunum or the ileum (Fig. 154-2).5
Diagnosis
Patients with symptoms of less than 4 weeks of duration are classified as having acute MVT. Those with symptoms lasting longer than 4 weeks but without bowel infarction, or those with clinically insignificant MVT diagnosed incidentally on abdominal imaging, are classified as having chronic MVT. The majority of patients—71% and 74% in two large clinical series4,7—have acute MVT.
Recognition by History and Physical Examination
Acute and particularly chronic MVT is a difficult diagnosis among patients presenting with acute or subacute abdominal pain. Awareness of the disease, a careful risk factor evaluation, and positive findings at physical examination should lead the clinician to the diagnosis. The onset of acute MVT is often insidious, and diffuse abdominal pain may be present for days or weeks. Abdominal pain is often,7,8 but not always, present at admission. The second-most common symptom is nausea/vomiting, whereas diarrhea and lower gastrointestinal bleeding are only present in less than 20% of cases.29,30 Typically, a middle-aged patient with a personal or a family history of deep venous thrombosis presents with abdominal pain of a few days’ duration, vomiting, and abdominal distention, as well as a clearly raised C-reactive protein level. The patient may develop localized peritonitis. With progression to transmural intestinal infarction, peristalsis ceases, and signs of generalized peritonitis occur.
Laboratory Testing
There are no accurate plasma biomarkers for diagnosing intestinal ischemia. D-dimer has been reported to be a sensitive but not a specific marker of acute thromboembolic occlusion of the SMA.31 From a theoretical point of view, we have reason to believe that a normal D-dimer level may be useful to exclude MVT as well. This view is supported by experience from a small series of patients.4
Further, because inherited thrombophilic factors are common in MVT, it is recommended that all patients with MVT should be screened for the following inherited disorders: factor V Leiden mutation, prothrombin gene mutation, protein C deficiency, protein S deficiency, JAK2 V617F mutation,19 and antithrombin deficiency. Simultaneously, the patient should be checked for acquired disorders such as lupus anticoagulant and cardiolipin antibodies.
Noninvasive and Invasive Testing
Multidetector computed tomography of the abdomen, with intravenous contrast injection and imaging in the portal venous phase, is the most important and accurate diagnostic tool.32–34 The protocol for acute CT of the abdomen varies with the clinical history provided by the referring physician who requests the examination. However, MVT is seldom suspected by the clinician before ordering CT; in fact, the diagnosis is often first made by the radiologist.35 In one series, MVT or intestinal ischemia was suspected before CT in only one patient with congenital portal vein occlusion out of 20 with verified MVT.35
The vascular and intestinal findings of MVT on multidetector computed tomography (Figs. 154-3 to 154-5) are summarized in Table 154-1.35 Multidetector computed tomography often demonstrates extensive thrombosis of the portomesenteric system, with extension of thrombosis to at least the extrahepatic portal and splenic veins. Intestinal findings are less common and more subtle. Hence the radiologist should always examine the mesenteric vessels in cases of an acute or unclear abdomen. MVT can be diagnosed using routine multidetector computed tomography techniques not optimized for MVT. However, a more dedicated CT protocol for the follow-up of patients with MVT, to assess both thrombotic status within the portomesenteric venous circulation and intestinal ischemia, is warranted (Table 154-2).35 This protocol can also be useful in MVT patients in whom the discontinuation of oral vitamin K antagonist (VKA) treatment is being considered or when patients on anticoagulation treatment are suffering from abdominal pain or experiencing a general deterioration in their condition.
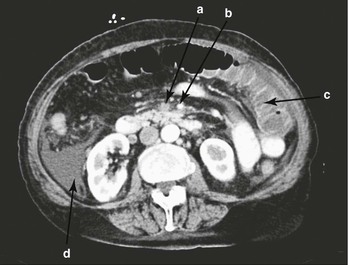
Figure 154-3 Multidetector computed tomography of the abdomen in the portal venous phase, in the axial projection, shows thrombosis of the superior mesenteric vein (a), an open superior mesenteric artery (b), dilatated and edematous small bowel loops (c), and ascites (d).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree