Chapter 24 Medical and Endovascular Treatment of Renal Artery Disease
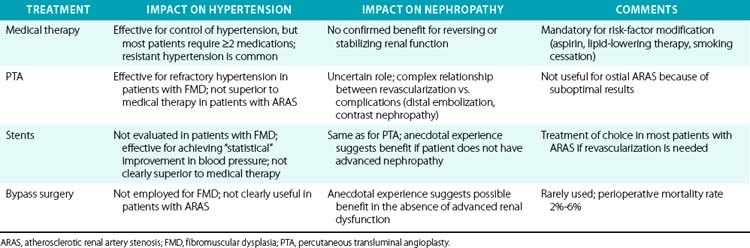
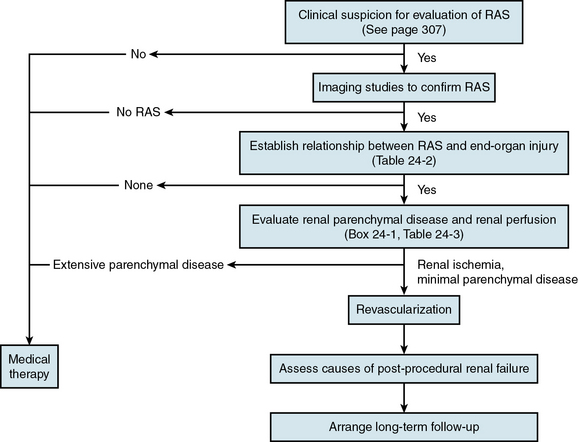
The clinical diagnosis of renal artery stenosis (RAS) relies on a high index of suspicion and confirmation by noninvasive and invasive imaging modalities (see Chapter 23). There are interrelated syndromes associated with RAS, including renovascular (renin-dependent) hypertension, essential hypertension, reversible ischemic renal dysfunction, and irreversible ischemic nephropathy. Clinical features that heighten suspicion for RAS include abrupt-onset or accelerated hypertension at any age, unexplained acute or chronic azotemia, azotemia induced by angiotensin-converting enzyme inhibitors (ACEIs), asymmetrical renal dimensions, and sudden pulmonary edema in the setting of normal left ventricular (LV) systolic function. Therapeutic considerations, alone or in combination, include medical therapy, percutaneous revascularization with angioplasty (PTA) or stenting, and surgical revascularization with bypass surgery or endarterectomy (Table 24-1). Revascularization of RAS with the goal of improving renal function and blood pressure remains controversial, so patient selection is extremely important (Fig. 24-1).
General Considerations for Treatment
Atherosclerosis accounts for more than 90% of cases of RAS, whereas the remaining 10% are associated with fibromuscular dysplasia (FMD) or inflammatory diseases of the renal arterial circulation. Whereas FMD is typically a disease of young and middle-aged females and usually involves the distal two thirds of the renal artery and its branches, atherosclerotic RAS (ARAS) is a disease of the elderly, particularly those with diabetes, aortoiliac occlusive disease, coronary artery disease (CAD), and hypertension. Atherosclerotic RAS usually involves the ostium and proximal one third of the renal artery, and it is a common manifestation of progressive atherosclerosis.1
Despite the prevalence and progressive nature of ARAS, it is likely many cases are never detected. Most patients with ARAS are identified during evaluation for refractory hypertension or progressive renal failure, or fortuitously as part of angiographic evaluation for aneurysmal or occlusive diseases of the aorta and lower-extremity arterial circulation. In general, decisions about treatment of patients with ARAS are usually based on blood pressure control, preservation of renal excretory function, and modification of risk factors for atherosclerosis.2
Identification of Renovascular Syndromes
There are five interrelated renovascular syndromes associated with RAS that can be broadly classified as anatomical RAS, renin-dependent hypertension, essential hypertension, reversible renal ischemic dysfunction, and irreversible ischemic nephropathy. These syndromes may occur alone or in combination with each other and with other nonvascular renal diseases. Furthermore, although the type of RAS (FMD, ARAS) is influenced by age, gender, and other patient-related risk factors for atherosclerosis, clinical manifestations (regarding effects on the kidney, heart, and brain) may be similar. Renin-dependent hypertension is much more likely to be caused by FMD in young patients, whereas ARAS in elderly patients is more likely to be associated with essential hypertension. Although both FMD and ARAS can be associated with similar manifestations of injury to the kidneys, heart, and brain (Table 24-2), renal revascularization is more likely to cure hypertension in FMD patients, whereas ARAS patients are likely to require lifelong antihypertensive medical therapy, despite revascularization. The key point is that patients with anatomical RAS without other clinical manifestations may be treated conservatively without revascularization. Prior to revascularization, patients with RAS and other clinical manifestations should undergo assessment of renal perfusion and the extent of parenchymal disease to determine the likelihood of clinical benefit.2
Table 24-2 Vital Organ Injury That May Be Caused by Hemodynamically Significant Renal Artery Stenosis
| Organ System | Injury |
|---|---|
| Renal | Ischemia/hypoperfusion |
| Cardiovascular | Hypertensive crisis ACS Unexplained pulmonary edema Aortic dissection |
| Cerebrovascular | Hypertensive crisis TIA Stroke ICH Severe retinopathy |
ACS, acute coronary syndrome; ICH, intracerebral hemorrhage; TIA, transient ischemic attack.
Evaluation of Renal Perfusion
As is true in the coronary circulation, there is poor correlation between angiographic RAS severity and hemodynamic significance, even when quantitative angiography is used.3 As a result, angiography alone is insufficient to establish the presence of renal hypoperfusion, regardless of stenosis severity. Several noninvasive and invasive methods are available to assess the physiological impact of ARAS and identify renal hypoperfusion (Box 24-1; also see Chapter 23). Nuclear scintigraphy and direct glomerular filtration rate (GFR) measurements can assess single- and total-kidney blood flow; diminished renal blood flow ipsilateral to a stenotic renal artery provides reliable evidence of renal hypoperfusion.4–6 Invasively, renal hypoperfusion can be identified with fractional flow reserve or translesional pressure gradients.3,7,8
![]() Box 24-1 Clinical Evaluation of Renal Artery Stenosis and Renal Hypoperfusion
Box 24-1 Clinical Evaluation of Renal Artery Stenosis and Renal Hypoperfusion
Invasive Assessment of Significance of Renal Artery Stenosis
Percent diameter stenosis by visual estimates or quantitative angiography
Translesional pressure gradient
Adapted from Safian RD, Madder RD: Refining the approach to renal artery revascularization. JACC Cardiovasc Interv 2:161–174, 2009.2
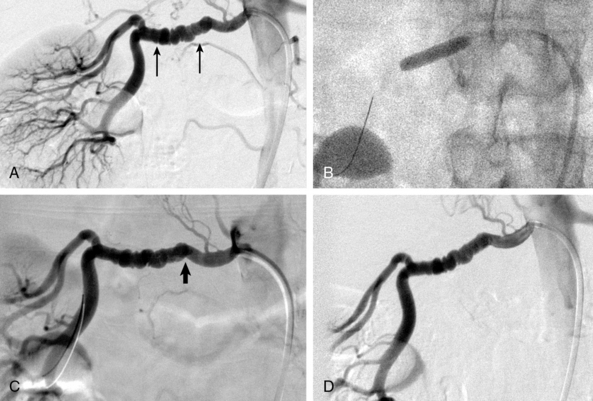
In patients with FMD, angiography alone is nearly useless for assessment of stenosis severity before or after revascularization, or for assessment of renal perfusion. In FMD patients, translesional pressure gradients are extremely useful for localizing the site of critical stenosis and assessing results after intervention (Fig. 24-2). Intravascular ultrasound (IVUS) can also be used to assess intraluminal and vessel dimensions, which are nearly impossible to assess by angiography alone.
Evaluation of Nephropathy
Assessment of baseline parenchymal disease is essential in selecting patients for renal revascularization (Table 24-3), since the presence of parenchymal disease prior to intervention is the most important predictor of adverse outcome. Even if renal hypoperfusion is present, identification of advanced parenchymal disease suggests that renal dysfunction maybe irreversible regardless of revascularization.9 The exception is the patient with advanced parenchymal disease, bilateral RAS, and recent dialysis, in whom a small increase in renal blood flow may permit separation from dialysis.2,10
Table 24-3 Clinical Evaluation of Renal Parenchymal Disease
| Factor | Comment |
|---|---|
| Serum Cr | Easy to measure and inexpensive. Relatively insensitive to degree of renal dysfunction and not reliable for differentiating nephropathy from renal ischemia. |
| Proteinuria | Easy to measure and inexpensive. Proteinuria ≥1 g/24 h is a good indication of nephropathy, but lesser degrees of proteinuria are less reliable. |
| Renal dimensions | Renal length 10-12 cm is generally favorable. Renal length ≤6 cm indicates irreversible renal injury (atrophic kidney). |
| RRI | RRI <70 is a good measure of reversibility. Although RRI >80 indicates parenchymal disease, it should not be used as the sole indicator of irreversible renal dysfunction. |
| Renal arteriogram | Preservation of cortical blood flow and absence of intrarenal arteriolar disease are indicators of reversible renal dysfunction. Poor cortical blood flow and severe diffuse intrarenal arteriolar disease are markers of advanced nephropathy. |
| Renal biopsy | Reliable for histological confirmation of nephropathy, but not practical for most patients. |
Cr, creatinine; RRI, renal resistive index.
Adapted from Safian RD, Madder RD: Refining the approach to renal artery revascularization. JACC Cardiovasc Interv 2:161–174, 2009.2
Initial clinical evaluation of parenchymal disease includes serum creatinine (Cr), urinalysis for proteinuria, and renal duplex ultrasound to measure renal resistive index (RRI) and kidney dimensions. When evaluating baseline renal function in patients with ARAS, it is important to realize that serum creatinine–based GFR estimates demonstrate good sensitivity but only modest specificity for identifying a measured GFR below 60 mL/min/1.73 m2 in individuals with ARAS.11 As a result, additional testing besides serum Cr should be performed to evaluate the presence of underlying nephropathy. Renal resistive index is obtained by averaging values obtained in the upper, middle, and lower intrarenal segmental arteries according to the formula 100 × [1 − (EDV/PSV)], where EDV and PSV are Doppler-derived end-diastolic and peak-systolic velocities, respectively. Compared to patients with RRI less than 80, those with RRI above 80 are older and have more extensive atherosclerosis and worse baseline renal function, consistent with more parenchymal disease. Additionally, baseline RRI greater than 80 is associated with inadequate blood pressure control, worsening Cr clearance, more frequent progression to dialysis, and higher mortality after renal revascularization.9 Several factors (renal dimensions, serum creatinine, presence of collaterals, and intact glomeruli by renal biopsy) have been proposed to suggest reversible renal failure, but the predictive value of these factors has not been validated, and renal biopsy is rarely employed for this purpose. Factors that identify irreversible dysfunction include severe diffuse intrarenal arteriopathy, proteinuria greater than 1 g/24 h (especially in a diabetic patient), and marked atrophy of the renal cortex.2
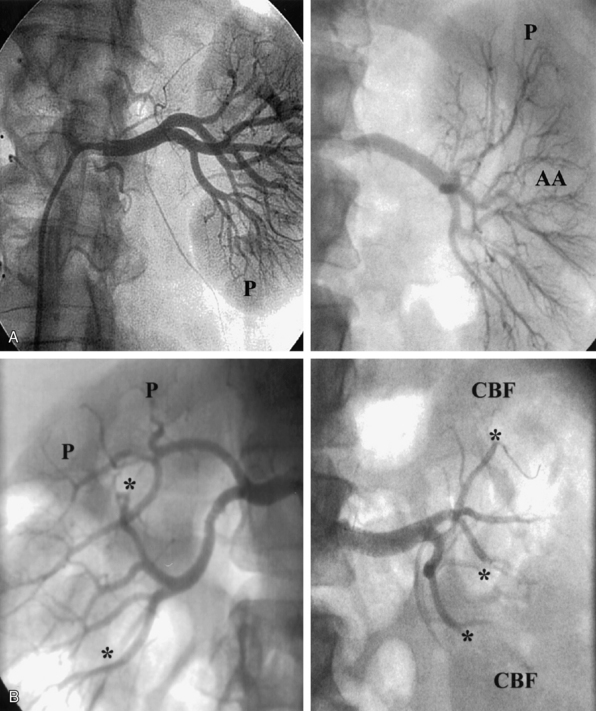
The nephrogram is often overlooked during selective renal arteriography, since many operators tend to focus on the renal artery itself. However, there are several arteriographic features that can indicate the presence of nephropathy, including intrarenal arteriolar narrowing, pruning (cut-off) of interlobar arterioles, and diminished cortical blood flow (Fig. 24-3). It is important to understand that it is best to use all the variables discussed to obtain a “nephropathy profile” because individual variables alone are not sufficiently reliable to assess the degree of nephropathy.2
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree