Figure 30.1
For this procedure, the patient is positioned supine with the arms tucked. A pillow or other support is placed behind the shoulders, allowing the neck to be extended and the chin to be mobilized out of the operative field. The surgical area is prepared widely to enable an emergency sternotomy in the unlikely event of an injury to a vascular structure. The radiographs should be reviewed and easily accessible for reference during the procedure. The first rib is identified beneath the head of the clavicle and the intercostal spaces, and subsequent ribs are counted caudally as the images are viewed through the series. With this method, the optimal location for the incision as it corresponds to the underlying pathology can be identified. The mediastinum may be accessed with or without resection of the costal cartilage. The need for resection should be determined before the skin incision is made; the incision will be located over the costal cartilage if the rib is going to be resected and over the intercostal space if it will be left intact. A 2- to 3-cm skin incision is made from the edge of the sternum out laterally. For aortopulmonary window pathology, ideal access is provided through the left second intercostal space, or the bed of the second rib; for other pathologies, the CT scan will dictate the side and level of the incision. The subcutaneous tissues, fascia, and pectoral muscles are divided with electrocautery
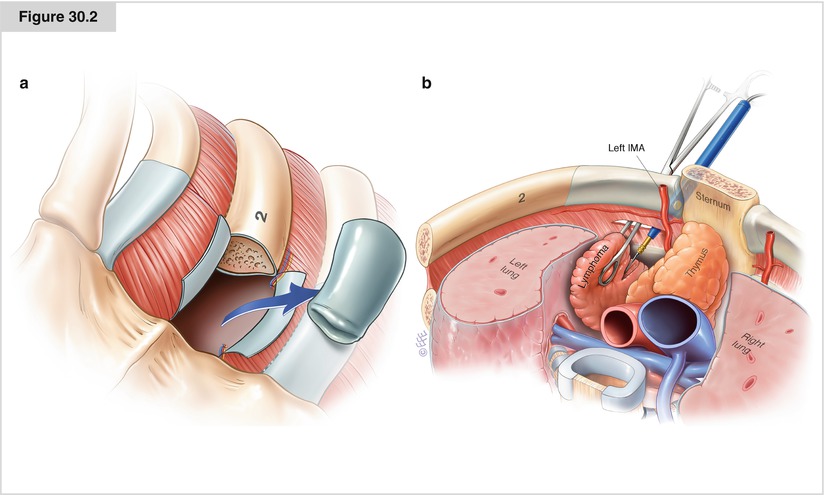
Figure 30.2




(a) The perichondrium overlying the costal cartilage is incised and dissected away from the cartilage with a periosteal elevator; care should be taken to avoid digging into the cartilage. The segment of cartilage usually is disarticulated from its insertion easily; if not, a periosteal elevator, knife, or rib cutting instrument may be used. The posterior perichondrium is then sharply divided, and the intercostal bundle is visualized; it may be ligated and divided. Depending on the patient’s body habitus and other details particular to the case, this may or may not be required. (b) If resection of the cartilage is not required, once the intercostal muscles are exposed, meticulous dissection is used to carefully divide the intercostal muscle fibers to avoid injuring the mammary vessels. If the required biopsy specimen is superficial, the surgeon can divide the posterior fascia and obtain tissue from either side of the vessels through the intercostal space using a biopsy forceps or multiple Tru-cut biopsies. For deeper biopsies, as in aortopulmonary pathology, the mediastinal pleura is swept away laterally to avoid entering the pleural space. The internal mammary vessels are best handled in a controlled fashion, as injury may lead to excessive bleeding. Once this is done, a finger may be inserted more readily for digital palpation. Once the capsule is penetrated, placing a ring forceps on the tissue and cutting around the grasped tissue with a knife or scissors facilitate adequate biopsy, particularly in the setting of a fibrosing or sclerosing lymphoma, in which diagnosis may be a challenge and a considerable amount diagnostic tissue is required
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


