Mediastinal Shift
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Pleural Effusion
Lobar Atelectasis
Pneumothorax
Less Common
Pneumonectomy
Radiation Fibrosis
Tuberculosis
Rare but Important
Hemothorax
Fibrothorax
Malignancy
Diaphragmatic Hernia
Scimitar Syndrome
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Direction of shift
Acuity of problem
Helpful Clues for Common Diagnoses
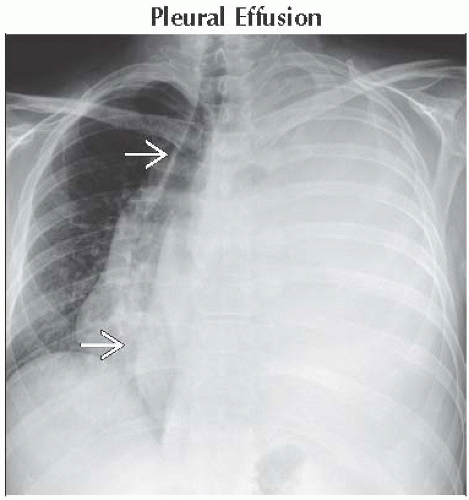
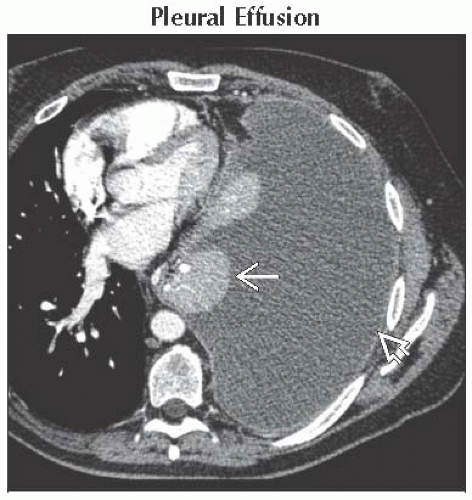
Pleural Effusion
Contralateral mediastinal shift
Opaque hemithorax
Pleural nodularity or thickening raises suspicion of malignancy
Causes of large unilateral fluid collections include
Infection, primary or metastatic malignancy, chyle, blood
Smoothly thickened and enhancing parietal pleura indicates exudative effusion
Chylous effusions are indistinguishable from transudative effusions
Secondary to obstruction by tumor, iatrogenic from surgery or trauma
Lobar Atelectasis
Ipsilateral mediastinal shift
Lobar collapse patterns
Obstructing neoplasm is more likely in outpatients
Mucus plug is more likely in inpatients
Pneumothorax
Convex pleural line paralleling chest wall
No vascular markings lateral to pleural line
Tension pneumothorax is clinical diagnosis with symptoms/signs including
Chest pain, hypoxia, circulatory collapse
Physical examination findings of pneumothorax
Suggestive/concerning radiographic findings of tension pneumothorax
Contralateral mediastinal shift
Flattening of diaphragm
Widening of rib interspaces
Complete collapse of lung
Helpful Clues for Less Common Diagnoses
Pneumonectomy
Small hemithorax with ipsilateral thoracotomy
Ipsilateral mediastinal shift
Opaque hemithorax secondary to fluid in pneumonectomy space
Radiation Fibrosis
Important threshold doses
Seldom visible ≤ 30 Gy
Nearly always visible ≥ 40 Gy
Incidence increases with 2nd course of therapy
Occurs 6-12 months after radiotherapy
No further progression 2 years after radiotherapy
Radiographic and CT findings
Ipsilateral mediastinal shift
Traction bronchiectasis, pleural thickening, and volume loss
Fibrosis does not obey lobar or segmental boundaries
Sharp and straight demarcation corresponding to radiation portals
Tuberculosis
Ipsilateral mediastinal volume loss with extensive post-primary tuberculosis
Activity difficult to determine without comparison radiographs
Common locations include
Upper lobes or superior segments of lower lobes
Radiographic or CT findings
Fibrosis
Traction bronchiectasis
Cavities
Adjacent emphysema
CT findings of active disease
Tree-in-bud opacities indicating endobronchial spread of infection
Cavitation
Consolidation
Rim-enhancing lymphadenopathy
Helpful Clues for Rare Diagnoses
Hemothorax
Most common cause is penetrating or blunt trauma
Less common associations include
Aortic dissection, rupture of aneurysm, or coagulopathy
Contralateral mediastinal shift
CT demonstrates high-density fluid (> 30 HU)
May see fluid-fluid level representing hematocrit effect
Organization may lead to fibrothorax
Fibrothorax
Marked unilateral pleural thickening ± calcification
Ipsilateral mediastinal shift
Causes include resolved
Hemothorax
Empyema
Tuberculosis effusion
Malignancy
Contralateral mediastinal shift often caused by tumors metastatic to mediastinum or lung
Causes include
Primary or metastatic germ cell tumors
Thymoma or thymic carcinoma
Mesothelioma
Endobronchial or extrabronchial mass causing lung collapse
Pleural metastases with large pleural effusions
Diaphragmatic Hernia
Diaphragmatic rupture with herniation of viscera into thorax
Secondary to high-energy blunt or penetrating trauma
Associated injuries can be many, including pneumo-/hemothorax, rib fractures, and pulmonary contusion
Bochdalek hernia
Bochdalek hernias are located “back and to the left”
Majority are small, contain fat, and are incidental
If containing bowel or kidney, may cause contralateral mediastinal shift
Large congenital hernias will usually be diagnosed prenatally by fetal ultrasound or MR
Morgagni hernia
Anterior and right-sided in location
Most contain omentum with small vessels
Most common viscera to herniate is colon
Scimitar Syndrome
Right lung hypoplasia with ipsilateral mediastinal shift
Anomalous pulmonary venous return of a portion or all of affected lung
Vein parallels right heart border
Decreased size of right pulmonary artery
Systemic to pulmonary collaterals to portions of right lung
Associated congenital heart disease in 25%
Image Gallery
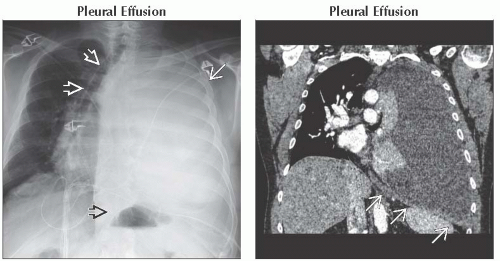 (Left) Frontal radiograph shows typical radiographic features of pleural effusion from mesothelioma. Note the complete opacification of the left hemithorax
 with mediastinal shift to the right with mediastinal shift to the right  . Stomach bubble is displaced inferiorly and medially . Stomach bubble is displaced inferiorly and medially  . (Right) Coronal CECT shows inversion of the left hemidiaphragm . (Right) Coronal CECT shows inversion of the left hemidiaphragm  and rightward mediastinal shift. and rightward mediastinal shift.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|