INDICATIONS/CONTRAINDICATIONS
Indications
It is well known that metastasis to hilar or mediastinal lymph node, the N factor, is one of the most important determinants of prognosis after lung cancer surgery. However, the role of lymphadenectomy in the staging and treatment of non–small cell lung cancer (NSCLC) remains controversial. Current surgical practice varies from visual inspection of the unopened mediastinum to systematic lymph node dissection (LND). Systematic mediastinal LND, as practiced by Japanese surgeons, is a much more extensive operation than that practiced by North American surgeons. Little et al. surveyed 729 hospitals to retrieve information on the patterns of surgical care provided to patients with NSCLC. The report included more than 11,000 patients with major pulmonary resections and showed that only 57.3% of patients had any mediastinal lymph nodes removed at the time of operation.
The purposes of hilar and mediastinal LND are accurate staging and the improvement of survival though better local control. The accurate staging is very important since several large-scale randomized trials have shown that postoperative adjuvant chemotherapy can improve the survival after surgery for NSCLC. There is no doubt that complete LND is the most accurate way to stage a patient’s disease and to determine which patients might benefit from adjuvant therapy. However, the extent of lymph node removal required and the impact of mediastinal lymph node removal on survival are still controversial.
Contraindications
Extensive pleural adhesion due to prior empyema, fibrosing mediastinitis, and calcified lymph nodes adherent to adjacent organs are contraindications for mediastinal LND due to technical difficulties. Mediastinal LND should not be performed for patients who would not tolerate with adjuvant therapy because of various reasons such as poor performance status, poor pulmonary function, other organ failure, and high age older than 80 years.
 SURGERY
SURGERY
Lymph Node Map
The first lymph node map was described by Naruke et al. in 1978. The American Thoracic Society developed ATS map in 1981, which was further revised by Mountain and Dresler in 1997 (MD-ATS map). There were several notable differences between the Naruke map and the MD-ATS map. The most significant discrepancy was that level 7 subcarinal lymph node in the MD-ATS map corresponded to levels 7 and 10 in the Naruke map. As a result, metastasis to the lymph nodes around the mainstem bronchus might be classified as N2, stage IIIA by the MD-ATS map or as N1, stage II by the Naruke map. As a consequence of the difficulties encountered in analyses of N descriptors, IASLC (the International Association for the Study of Lung Cancer) lymph node map was proposed in 2009.
The IASLC map has revised the anatomical definition of each lymph node level. The supraclavicular and sternal notch lymph nodes are described as level 1. The pleural reflection is no longer used as the boundary between mediastinal and hilar lymph nodes. The entire subcarinal group of lymph nodes is now defined as level 7 with precise anatomic borders. The boundary between the right- and left-sided level 2 and 4 lymph nodes has been reset to the left lateral wall of the trachea. Beside the level, the new concept of lymph node location, “zone” is proposed for future survival analysis.
Definitions of Surgical Lymph Node Assessment
Although nodal staging of NSCLC should be as accurate as possible, the surgical technique for lymph node assessment varies among countries and centers. It should be also noted that different terms are used to describe these surgical techniques. The definitions for various types of lymph node assessment were recently proposed by the council of the European Society for Thoracic Surgeons.
Lymph Node Biopsy
Only suspicious one or multiple lymph node(s) are biopsied to prove N1 or N2 disease. No systematic nodal dissection or biopsies are performed. The procedure is performed only to document lymph node metastasis when resection is not justified (Fig. 6.1A).
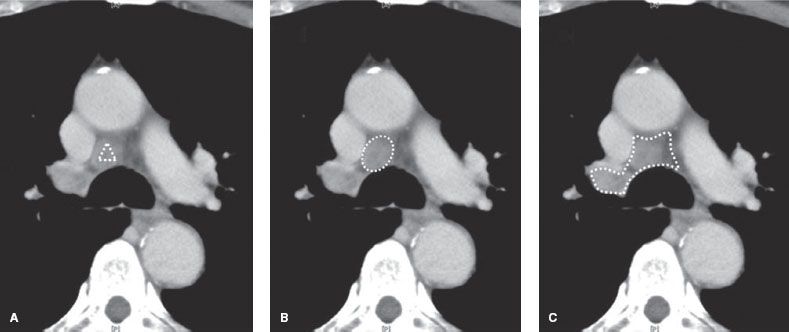
Figure 6.1 These three figures demonstrate the differences in the surgical technique for lymph node assessment. A: Lymph node biopsy. B: Lymph node sampling. C: Lymph node dissection.
Lymph Node Sampling
One or more lymph nodes are removed without any surrounding tissue, guided by preoperative or intraoperative findings that are thought to be representative (Fig. 6.1B). Systematic lymph node sampling (LNS) means that a predetermined sampling of the lymph node stations is performed.
Lymph Node Dissection
The mediastinal tissue containing lymph nodes is dissected and removed systematically within anatomical landmarks (Fig. 6.1C). In other words, all of the lymph nodes in the targeted compartment must be completely removed, as a block, together with surrounding adipose tissue. In general, following lobe-specific LND should be performed:
Right upper and middle lobe: 2R, 4R, and 7
Right lower lobe: 4R, 7, 8, and 9
Left upper lobe: 5, 6, and 7
Left lower lobe: 7, 8, and 9
Technique of Mediastinal Lymph Node Dissection
As described in the definition, all of the lymph nodes in the targeted compartment must be completely removed, as a block, together with surrounding adipose tissue. Attention should be given not to remove visible lymph nodes but rather to dissect landmark anatomies surrounding the lymph nodes. Although mediastinal LND is commonly performed after completion of the pulmonary resection, it can be done before lung removal under the drier operation field.
Open Approach
Right
Right mediastinal lymph nodes are exposed via either a posterolateral thoracotomy or muscle-sparing anterolateral thoracotomy. Entry into the fourth intercostal space provides excellent access to the superior mediastinal nodes. The fifth intercostal space provides better access to the inferior mediastinal nodes.
Right 2, 4. A longitudinal incision is made on the parietal pleura overlaying the level 2R/4R between the azygos vein and the right brachiocephalic artery. Another horizontal pleural incision is made at the level just above the azygos vein. The azygos vein is taped and retracted caudally. Some surgeons prefer to divide the azygos vein to have better access to 4R, but it is not necessary. The phrenic nerve is identified on the lateral border of the SVC. The vagus nerve, which traverses the superior mediastinum, is taped and retracted backward. Traction is placed on the pleural edge over the SVC and the superior mediastinal fat pad is dissected from the lateral aspect of the SVC. Small veins draining into the SVC are cauterized and served (Fig. 6.2). The mediastinal fat pad is retracted anteriorly and dissected from the anterior aspect of the trachea. Retracting the mediastinal fat pad caudally, the caudal border of the innominate artery is exposed by a cautery. The dissection is continued on the lateral aspect of the pericardium of the aortic arch. The azygos vein is elevated by a tape and the fat pad is passed through the azygos vein caudally (Fig. 6.3). The dissection is completed at the cephalic border of the right upper lobe bronchus. Care must be taken not to injure the pulmonary artery.
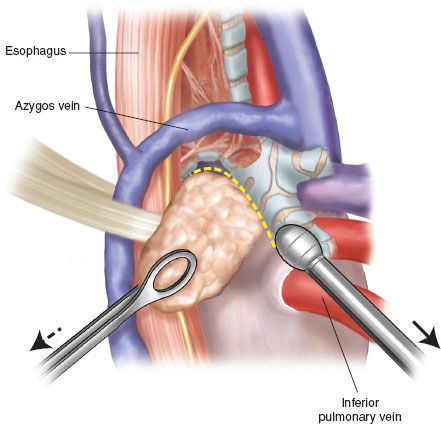
Right 7. A longitudinal incision is made on the posterior mediastinal pleura overlaying the level 7 between the right inferior pulmonary vein and the azygos vein. The vagus nerve is identified on the surface of the esophagus and then it is taped and retracted posteriorly. The small branches of the vagus nerve running into the lung are divided. The plane between the esophagus and the subcarinal fat pad can be dissected bluntly. To widen the subcarinal space, the esophagus is retracted posteriorly by a plain retractor and the right intermediate bronchus is retracted anteriorly by a peanut sponge. The subcarinal fat pad is grasped gently by a lymph node clamp and dissected from the left main bronchus (LMB) (Fig. 6.4). Small branches of the bronchial artery are cauterized or clopped. This part should be dissected first because this area is the deepest part of the chest cavity with a lateral decubitus position and will be obscured by bloody effusion later. Then, the dissection is carried out at the lower rim of the subcarinal fat pad by exposing the pericardium. The dissection is continued on the membranous portion of the intermediate bronchus toward the carina (Fig. 6.5). The prominent bronchial artery should be ligated or clipped.
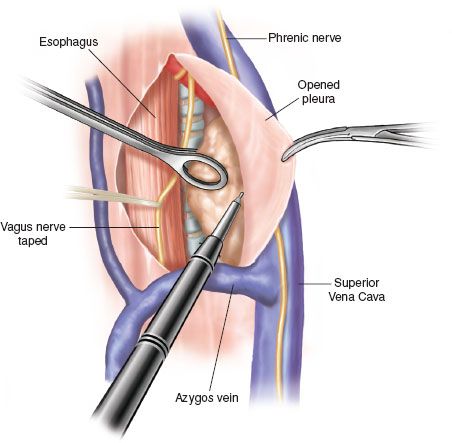
Figure 6.2 Dissection of lymph node levels 2R and 4R. Traction is placed on the pleural edge over the SVC, and the superior mediastinal fat pad is dissected from the lateral aspect of the SVC.
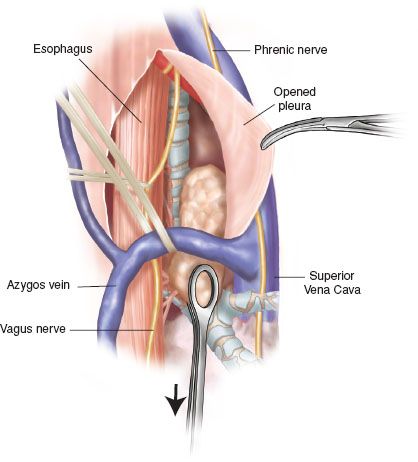
Figure 6.3 Completion of dissecting lymph node levels 2R and 4R. The azygos vein is elevated by a tape and the fat pad is passed through the azygos vein caudally. The dissection is completed at the cephalic border of the right upper lobe bronchus.
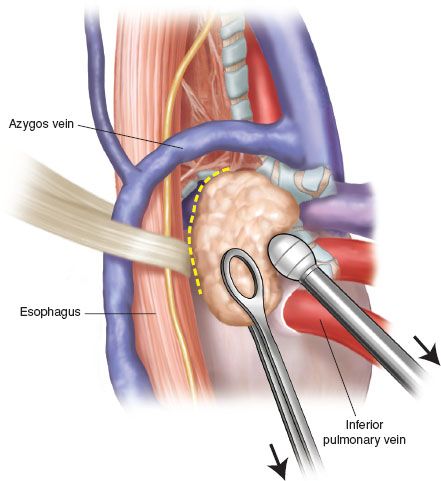
Figure 6.4 Dissection of lymph node level 7 via right thoracotomy. To widen the subcarinal space, the esophagus is retracted posteriorly by a plain retractor and the right intermediate bronchus is retracted anteriorly by a peanut sponge. The subcarinal fat pad is grasped gently by a lymph node clamp and dissected from the left main bronchus and the esophagus (dotted yellow line).