16 Mechanical Ventilation of the Neonate
Note 1: This book is written to cover every item listed as testable on all Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and WRE, it will simply be shown as (Code: …). If an item is only testable on the ELE, it will be shown as (ELE code: …). If an item is only testable on the WRE, it will be shown as (WRE code: …).
Note 2: A review of the most recent Entry Level Examinations (ELE) has shown an average of one question (out of 140), or <1% of the exam, will cover continuous positive airway pressure (CPAP) or mechanical ventilation of the neonate. A review of the most recent Written Registry Examinations (WRE) has shown an average of two questions (out of 100), or 1% of the exam, will cover continuous positive airway pressure (CPAP) or mechanical ventilation of the neonate. Of the 10 tested scenarios of the Clinical Simulation Examination, expect one neonatal patient and one pediatric patient. CPAP or mechanical ventilation may be involved in both situations. Be sure to review neonatal and pediatric assessment items in Chapter 1.
MODULE A
1. Initiate and adjust an elevated baseline pressure: continuous positive airway pressure (CPAP) breathing (Code: IIID2d) [Difficulty: ELE: R, Ap; WRE: An]
a. Physiologic effects
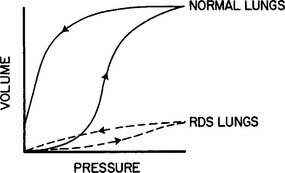
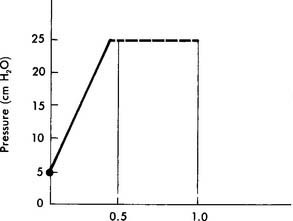
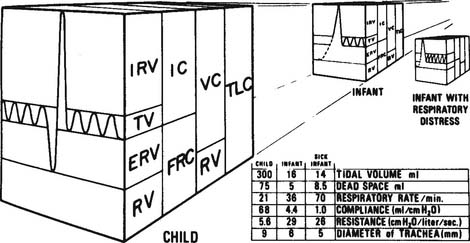
Continuous positive airway pressure (CPAP) and positive end-expiratory pressure (PEEP) increase the patient’s functional residual capacity (FRC). In neonates, the most common cause of a decreased FRC is infant respiratory distress syndrome (RDS). This condition is caused by the lack of surfactant in the lungs of the premature neonate. The neonate with RDS has relatively airless lungs that are prone to atelectasis. This results in hypoxemia. In addition, each tidal volume breath requires a greater than normal inspiratory effort (Figure 16-1). The restoration of FRC in the neonate increases its Pao2, decreases the percentage of shunt, narrows the alveolar to arterial difference in oxygen, and reduces its work of tidal volume breathing. CPAP must be used with caution in neonates with persistent pulmonary hypertension (PPHN) of the newborn. An excessive amount of pressure in the alveoli compresses the capillary bed. This decreases pulmonary blood flow, which in turn increases blood flow through the patent ductus arteriosus and worsens the problem.
b. Indications, contraindications, and hazards
CPAP is indicated for any condition that results in an unacceptably low Pao2 secondary to a decreased FRC. Some neonates respond so well to CPAP that mechanical ventilation is not needed. In addition, CPAP has been used to keep open the airways of infants with tracheal malacia or other conditions in which the airways collapse abnormally. In general, contraindications include any CPAP-related condition that results in a worsening of the patient’s original status. Some neonates cannot tolerate CPAP and progressively hypoventilate as the pressure level is increased. Clinical judgment is needed to decide how high the PaCO2 should be allowed to rise before discontinuing the CPAP and beginning mechanical ventilation. In general, the PaCO2 should not be greater than 50 torr as long as the pH is at least 7.25. An absolute contraindication is apnea resulting in hypoxemia and hypotension. These infants should be mechanically ventilated. Box 16-1 gives a complete listing of indications, contraindications, and hazards.
BOX 16-1 Indications, Contraindications, and Hazards of CPAP Therapy
INDICATIONS
c. Initiation
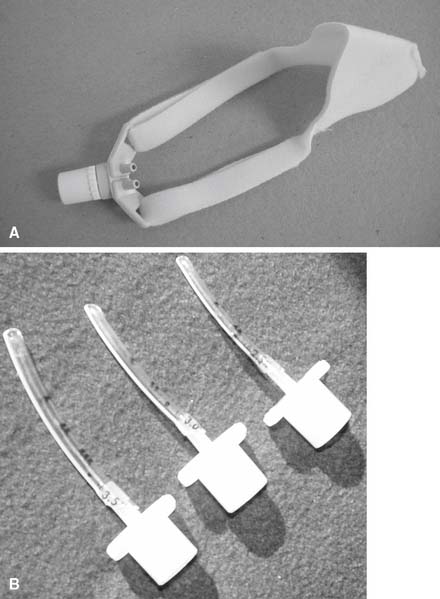
Before starting CPAP, a set of baseline arterial blood gases should be taken. Transcutaneous oxygen monitoring or pulse oximetry may be substituted in some clinical situations if oxygenation is the only parameter that must be measured. The neonate’s vital signs should also be recorded. Assemble the CPAP circuit and pressure device. The decision must be made whether to apply the CPAP above the epiglottis (Figures 16-2 and 16-3) or to intubate the infant and apply the CPAP within the trachea. Nasal CPAP (NCPAP) or nasopharyngeal tube CPAP (NP-CPAP) are both widely used to apply pressure from above the epiglottis. The neonate or infant must have an endotracheal tube placed to apply CPAP within the trachea. Among the factors to be considered are the neonate’s gestational age and weight, the amount of secretions that need to be suctioned, the pulmonary problem, and the likelihood of mechanical ventilation eventually becoming necessary. More mature and larger infants with few secretions and relatively stable pulmonary conditions will most likely have CPAP applied above the epiglottis by nasal prongs or nasopharyngeal tube. In contrast, less mature and smaller infants (less than 1000 to 1200 g) who need suctioning and have relatively unstable pulmonary conditions will probably be intubated. Mechanical ventilation can then be easily started if needed.
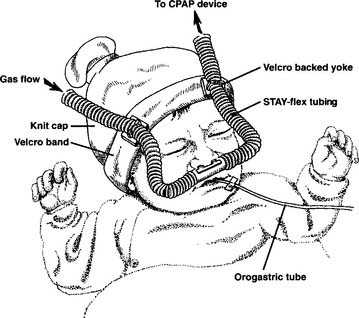
Figure 16-3 An assembly for supporting nasal CPAP prongs in an infant.
(Modified from advertisement of Stayflex tubing system from Ackrad.) (From Sills JR: Respiratory care registry guide, ed 1, St Louis, 1994, Mosby.)
d. Monitor and adjust alarm settings (ELE Code: IIIG3g) [Difficulty: ELE: R, Ap, An]
Equipment should have visual and audible alarms and include the following features:
e. CPAP adjustment
Blood gases and vital signs must be evaluated at the starting CPAP level. The heart rate, blood pressure, and respiratory rate should be stable or improved. Wait at least 10 minutes after a change in CPAP before getting an arterial blood gases sample. See Table 16-1 for the recommended blood gas limits. In general, the Pao2 should be kept between 60 and 70 torr, PaCO2 less than 50 to 55 torr, and pH at least 7.25. If the Pao2 is too low and the patient’s vital signs are acceptable, the CPAP may be increased in a step of 1 to 2 cm water. The vital signs and blood gases should then be reevaluated. In addition, the neonate’s work of breathing can be indirectly assessed. Improved lung function will be demonstrated by seeing decreased respiratory rate, retractions, expiratory grunting, and nasal flaring. If necessary, the process of adding CPAP and reassessing the patient can be continued. The maximum CPAP level in a neonate is generally held to be 10 cm water; the maximum CPAP level in an infant is generally held to be 15 cm water.
TABLE 16-1 Commonly Recommended Blood Gas Goals for CPAP and Mechanical Ventilator Therapy
| Age of Neonate | ||
|---|---|---|
| Less Than 72 Hours | Greater Than 72 Hours | |
| Pao2 (torr) | 60-70 | 50-70 |
| Ptco2 (torr) | Greater than 50,* less than 90* | Greater than 40,* less than 90* |
| Spo2 | 92%-96% | 92-96% |
| PaCO2 (torr) | 35-45† | 45-55 |
| PtcCO2 (torr) | May be used after correlation with PaCO2 as discussed in Chapter 3. | |
| pH | 7.25-7.45 | 7.25-7.45 |
NOTE: Keep the Pao2 no greater than 80 torr in the premature neonate to reduce the risk of retinopathy of prematurity.
* Ptco2 values may be used after they have been shown to correlate within 15% of the Pao2 from an arterial blood gas.
† With CPAP, this value may be increased to 50 to 55 torr as long as the pH is at least 7.25.
f. Independently initiate weaning from CPAP (Code: IIIF2i12) [Difficulty: ELE: R, Ap; WRE: An]
As the patient improves, it is necessary to reduce the CPAP level so as not to cause pulmonary barotrauma. The pressure level can be reduced in steps of about 2 cm water. The vital signs and blood gases should be reassessed after each step. The apparatus is usually removed when the CPAP level is down to 2 to 4 cm water. The infant is then placed into an oxyhood at the same oxygen percentage as before or 5% to 15% higher. If the infant has an endotracheal tube that is needed for suctioning or a secure airway, the pressure is usually left at 2 to 4 cm water. After extubation, the infant is placed into an oxyhood as before. Alternatively, the neonate may be weaned to a high flow nasal cannula and then to a traditional, low-flow nasal cannula. See Chapter 6 for more discussion on the high-flow nasal cannula.
MODULE B
1. Select a mechanical ventilation
a. Recommend changing the type of ventilator to be used on the patient (Code: IIIG3i) [Difficulty: ELE: R, Ap; WRE: An]
2. Adjust the ventilator settings.
a. Initiate and adjust continuous mechanical ventilator settings (Code: IIID2b) [Difficulty: ELE: R, Ap; WRE: An]
b. Recommend changes in mechanical ventilation to modify ventilator techniques (Code: IIIG3e) [Difficulty: ELE: R, Ap; WRE: An]
d. Sensitivity
1. Observe the patient for signs of ventilator-patient dyssynchrony (Code: IIIE5b) [Difficulty: ELE: R, Ap; WRE: An]
2. Independently adjust the ventilator to improve patient synchrony (Code: IIIF2i1) [Difficulty: ELE: R, Ap; WRE: An]
There is no sensitivity control on traditional continuous flow TPTV-type neonatal ventilators. The IMV mode is used with these units. Newer ventilators have the ability to sense a neonate’s respiratory effort and trigger a machine delivered breath. Some units sense a change in flow through the ventilator circuit when the neonate inspires. Other ventilators make use of electrocardiogram-type leads on the neonate’s chest to sense a change in electrical impedance (skin resistance) when the neonate makes an inspiratory effort. A child on a volume-cycled ventilator should have the sensitivity set at about −1 to −2 cm water pressure. No matter which method the ventilator uses to sense the patient’s respiratory effort, the neonate or child should not have to work hard to trigger a machine tidal volume.
f. I : E ratio
3. Indications for mechanical ventilation
All authors agree that apnea is an absolute indication for mechanical ventilation. A general indication is any condition that causes respiratory failure. This is usually documented by unacceptable arterial blood gases. Box 16-2 lists indications for mechanical ventilation.
BOX 16-2 Common Indications for the Initiation of Mechanical Ventilation
RESPIRATORY FAILURE
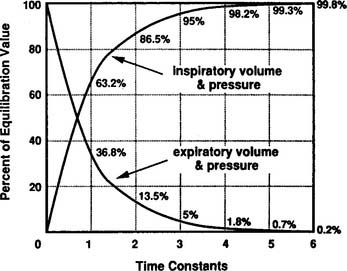
Although technically impractical to measure the time constant of ventilation at the bedside, the concept is important because it relates to two important clinical considerations during mechanical ventilation. First, it relates to the pressure that develops at the alveolar level as the tidal volume is delivered. For each time constant, progressively more of the peak inspiratory pressure (PIP) is applied within the alveoli (Figure 16-4). As can be seen, at three time constants, 95% of the PIP is applied to the alveoli. At five time constants, virtually the entire PIP is applied at the alveolar level. Second, the time constant relates to how rapidly the lung recoils to baseline (FRC) during an exhalation. As shown in Figure 16-4, it takes three time constants to exhale 95% and five time constants to completely exhale.
4. Initiation and adjustments based on the patient’s condition
a. Patients with normal cardiopulmonary function
Patients with normal cardiopulmonary function may need mechanical ventilation because of apnea from anesthesia, paralysis, or a neurologic condition. The initial TPTV ventilator parameters for this type of patient are listed in Box 16-3. Once mechanical ventilation is established, it is important to evaluate the patient’s blood gases, vital signs, breath sounds, and any other pertinent clinical information before changing any ventilator parameters.
BOX 16-3 Common Mechanical Ventilator Parameters for Neonates with Normal Lungs
As the patient recovers and begins to breathe spontaneously, it will probably be necessary to reduce the ventilator-delivered minute volume. This encourages the child to breathe more because the final goal is to completely wean and extubate the patient. The most accepted way to reduce the ventilator-delivered minute volume is to reduce the ventilator rate. A reduction of about 10% is a good starting place but must be tailored to meet the patient’s needs. The tidal volume is maintained as originally set. Obtain a set of blood gases in 10 to 20 minutes (or follow the transcutaneous or pulse oximetry values), and check the patient’s vital signs to see how well the adjustment is tolerated.
CALCULATION OF ESTIMATED TIDAL VOLUME DURING TPTV MECHANICAL VENTILATION
 = inspiratory flow rate on the ventilator in mL/sec
= inspiratory flow rate on the ventilator in mL/sec
Vc = volume compressed in the circuit and ventilator
 = 5.5 L/min. This is converted to mL/sec by dividing the flow in L/min by 60 seconds. So 5.5 L/min = .092 L/sec or 92 mL/sec:
= 5.5 L/min. This is converted to mL/sec by dividing the flow in L/min by 60 seconds. So 5.5 L/min = .092 L/sec or 92 mL/sec:It must be emphasized that this is only a calculated tidal volume. Leaks in the system, a decrease in the patient’s compliance, or an increase in the patient’s resistance decreases the true tidal volume. Conversely, an increase in the patient’s compliance or a decrease in the patient’s resistance increases the true tidal volume. Also, if the pressure limit is reached before the inspiratory time is completed, less volume than expected will be delivered. This is because part of the inspiratory time is spent as an inflation hold and no additional tidal volume is delivered (Figure 16-5). Finally, the infant must be completely passive during the delivery of the breath.
b. Patients with decreased lung compliance and normal airway resistance such as infant respiratory distress syndrome (RDS)
Although RDS in infants weighing less than 1000 g is the most common cause of decreased lung compliance with normal airway resistance, stiff lungs are also found in patients with other lung conditions such as pneumonia and pulmonary edema (Figure 16-6). The greatest challenge presented in the care of these infants is to oxygenate them without causing oxygen toxicity or pulmonary barotrauma. Common recommendations for the initial ventilator settings are listed in Box 16-4. As discussed earlier, blood gases, vital signs, and so forth must be monitored after the infant is placed on the ventilator. Any further adjustments can then be determined and evaluated by another set of blood gases and vital signs.
BOX 16-4 Common Mechanical Ventilator Parameters for Neonates with Low Compliance and Normal Resistance
The issue of time constants of ventilation helps to better explain the various options available for adjusting the ventilator. As presented earlier, the time constant of ventilation (Tc or time constant of the respiratory system TRS) is calculated as the product of compliance and resistance. For example, using the following values for a mechanically ventilated neonate with RDS, its time constant is calculated as
1. Administer oxygen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree