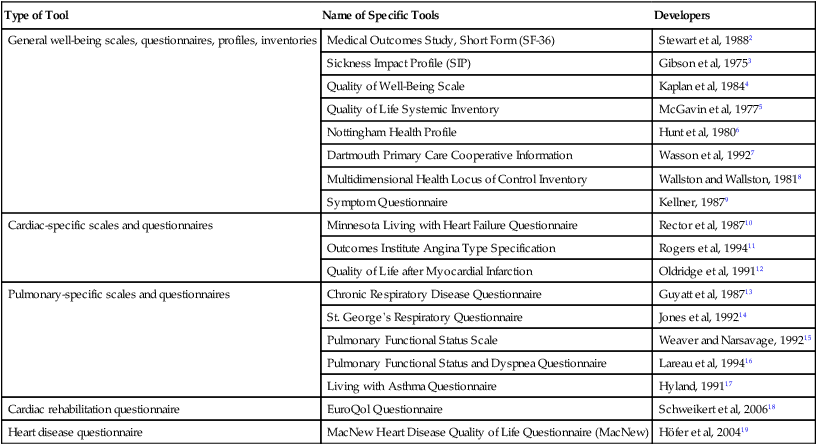
As direct access to patients becomes globally accepted, the capacity of the physical therapist to diagnose problems that are amenable to, as well as not amenable to, physical therapy is crucial for effective, safe, and responsible care. After formulating the diagnoses in partnership, as much as possible, with the patient and consistent with the health care team overall, the physical therapist prioritizes the diagnoses to address those most critical to the patient. These diagnoses may not necessarily be the reason the individual initially sought care from, or was referred to, a physical therapist. This is the essence of evidence-informed practice in the context of epidemiological indicators as distinct from evidence-based practice that supports the effectiveness of specific interventions (see Chapter 1). This chapter provides a basis for clinical decision making and intervention prescription in physical therapy for patients ranging from the individual who is medically unstable and critically ill to the individual who is medically stable with cardiovascular and pulmonary dysfunction or at risk and living in the community. In addition, physical therapists have an active role in wellness and its promotion in the form of structured programs as well as one-on-one care. Thus the individuals they counsel include those with cardiovascular and pulmonary pathologies secondary to impairments or threats of other organ systems as well as those with primary impairments or threats of the cardiovascular and pulmonary systems (see Chapter 6). Clinical reasoning is the process of critically analyzing the patient’s status (participation in life and activities, as well as anatomic structures or physiological function) with respect to the individual’s psychosocial, cultural, and environmental contexts (see Chapters 1 and 17). What is the individual able to do (and not able to do)? What is the status of the organ systems? How do these two interrelate? The answers to these questions serve as the basis of the detailed diagnostic work-up by the physical therapist. This process results in the diagnoses or problems that are then prioritized to ensure that the patient’s needs are addressed appropriately—that is, “the right interventions targeted at the right problems at the right time.” Initial priorities include life-preserving interventions (including addressing threats) and the minimizing of physical and psychological distress. Facilitators and barriers to the patient’s adhering to the intervention recommendations, including health literacy and lifestyle education, are clearly identified, and education and interventions are adapted to meet the needs of the individual. With this database, the physical therapist prescribes interventions so that their outcomes are maximized in the short term and the long term. For most individuals, the highest priority is the capacity to live a life consistent with their needs and wants according to their sociocultural norms. The World Health Organization (WHO) acknowledges this in its International Classification of Functioning, Disability and Health, which emphasizes the interrelationship among structure and function, activity, and participation in life. Health has been defined by WHO as emotional, spiritual, intellectual, and physical well-being—not merely the absence of pathology.1 Participation refers to the capacity of individuals to fulfill these needs in a social context and thereby fulfill the multiple roles in their lives—as parent, child, sibling, employee, employer, student, or homemaker, as well as in avocational pursuits (Figure 17-1). Participation in life is assessed by open-ended questions asked during the history and interview. In addition, an increasing number of questionnaire tools and scales are available for clinical use. Table 17-1 outlines some common generic and condition-specific tools that can be used to assess quality of life, life satisfaction, sickness impact, and subjective sense of well-being. These can be useful outcome measures (technically, these scales provide scores that are indexes rather than actual measures of the constructs) for the physical therapist and the patient. Many of these scales have been shown to be reliable as well as valid. Validating these scales is conceptually and methodologically challenging; hence their limitations must be recognized. Table 17-1 Tools for Evaluating Domains of Quality of Life (Activity and Participation) Participation in life and fulfilling one’s roles and obligations require the ability to perform a range of certain activities to some level of proficiency (see Figure 17-1). The role of a parent, for example, requires being able to identify the needs of children, as well as to plan and coordinate activities involved with their care (e.g., picking them up, bathing and dressing them, performing physical activities and playing with them, and taking them to school). With respect to occupational roles, for example, to fulfill the needs of being a truck driver, the individual needs to be able to get to work, climb into the truck, check the engine, crawl under the truck, load and unload the truck, read a map, and operate a standard transmission. To be an elementary school teacher requires being able to move around the classroom, help children with physical tasks, and anticipate their needs, stay alert to danger, and respond quickly. The physical therapist’s assessment must identify the composite activities that are limited and that affect an individual’s capacity to participate in fulfilling his or her roles. Limitations of anatomic structure and physiological function often interfere with the performance of specific activities that are involved in fulfilling roles and obligations in life (i.e., participating in life) (see Figure 17-1). Some limitations may be specific to a particular role, and some may interfere across roles. The physical therapy assessment identifies the limitations of structure and function and the degree to which they interfere with given activities and roles in life. Some limitations of structure and function related to oxygen transport do not necessarily limit activity or participation; yet they can be the most clinically important, life-threatening problems (e.g., high blood pressure, cardiac dysrhythmias, abnormal clotting factors, high blood glucose, and aerobic deconditioning). Given the prevalence of lifestyle-related conditions and their risk factors, each individual needs to be assessed for risk for heart disease, smoking-related conditions, hypertension and stroke, diabetes, and cancers (see Chapter 1). Assessment of a patient’s bone health and risk for osteoporosis and arthritis is also prudent, especially now that individuals are generally living longer and often have lifestyles that predispose them to osteopenia and osteoporosis. Physical therapists have a primary role in assessing these risks for several reasons: First, these problems can be the most important clinically in terms of health and threat to life (chronic morbidity and premature death) for the patient, either directly or indirectly. Second, identifying these problems enables the physical therapist to work collaboratively with the health care team in addressing and following the patient in a coordinated, integrated manner. If a patient was not referred and new problems are detected, the physician needs to be alerted. With direct-access practice, this is a primary responsibility of the contemporary physical therapist. If risk factors have been identified or have manifested clinically, the patient may be taking medication or may be a candidate for surgery. The physical therapist has a primary role in avoiding or minimizing the need for invasive care (specifically, drugs and surgery)—this is a particularly important and often underestimated goal of the physical therapist, who is committed to using and promoting noninvasive care. The physical therapist must closely monitor a patient’s responses to invasive care (i.e., drugs and surgery) in relation to problems of direct relevance to them, with the intention of reducing such intervention. Third, the physical therapist needs to institute relevant and targeted health education for lifelong behavior change (i.e., assess the patient’s needs, including health literacy, knowledge deficits about health and health status, learning readiness, and learning style; tailor the education materials to the learner; and assess the outcome of the educational intervention comparable to other physical therapy interventions) (see Chapters 1 and 27). Fourth, the presence of risk factors may require a higher level of patient monitoring, including the results of invasive testing (e.g., blood work for cholesterol, triglycerides, and blood glucose) and other tests such as imaging results and ECGs. Fifth, physical therapy interventions and their prescriptive parameters may need to be modified based on an individual’s risk factors for lifestyle-related conditions. Sixth, special attention to medications may be indicated, and these may need to be coordinated with physical therapy management. Seventh, the presence of risk factors for lifestyle-related conditions requires long-term management and follow-up. Psychosocial and cultural factors are assessed to identify beliefs, attitudes, lifestyle behaviors, and expectations of care (see Chapter 1). A learning assessment (see Chapter 28) is conducted to identify health literacy and knowledge deficits, the learning style of the patient, and readiness to participate in intervention. Identifying facilitators and barriers that will impact the outcome of the therapeutic relationship is central to ensuring maximal therapeutic outcomes, including an individual’s subjective sense of well-being and empowerment. The principles involved in relating cardiovascular and pulmonary physical therapy interventions to the patient’s needs depend on an analysis of those needs with respect to the patient’s level of participation in life and ability to perform the identified composite activities. The degree to which limitations of anatomic structure and physiological function (with a focus on impairments of the steps in the oxygen transport pathway; Chapter 2) affect activity and participation is assessed. The relationship of impairment to an individual’s ability and participation cannot be assumed. Verification can be extracted from the history and overall assessment, including measures and indexes of the individual’s capacity to perform activities and participate in life. These aspects of the assessment can be obtained through the use of standardized questionnaire tools that reveal the impact of health-related quality of life and sickness; these tools can be used as outcome measures in conjunction with measures of anatomic structure and physiological function (see Table 17-1). Changes in structure and function with intervention may or may not have a corresponding effect on health-related quality of life or sickness. For example, high blood pressure is most often asymptomatic, but the patient may be prescribed a stringent exercise program and education program. Such knowledge may help to identify those individuals whose quality of life is most likely to improve, as well as where intervention should be targeted.20 The physical therapist formulates a physiologically based intervention hierarchy based on the premise that physiological function, including oxygen transport, is optimal when humans are upright and moving (see Chapters 18, 19, and 20). Applying a systematic physiological approach to diagnosis and the analysis of the patient’s problems, with respect to limitations in the oxygen transport pathway, leads directly to identifying effective interventions. Such an approach provides a rational basis for modifying or discontinuing intervention based on the use of appropriate outcome measures. Consistent with the International Classification of Functioning, Disability and Health, there are three primary levels of analysis:21 These components are affected by facilitating factors and barriers (see Figure 17-1).21 Structure and function refer to the underlying anatomic and physiological limitations that may or may not contribute to the patient’s symptoms but are clinically important and warrant remediation or being addressed in management. Limitation of activities contributes to a compromised capacity to fulfill one’s roles in life, such as those of occupation, profession, parent, and member of various groups that make up an individual’s identity. Usually, a patient presents clinically with complaints of being unable to complete tasks or fulfill roles because of pathophysiological, psychological, or environmental and physical barriers and limitations. Measures and tools are standardized (concerning validity and reliability, see Chapter 7) for the assessment of each of these levels. With an increased focus on the quality of participation in life, numerous scales have emerged to quantify the subjective sense of well-being and health-related quality of life (see Table 17-1 for some examples). Oxygen transport is determined by a multitude of factors that affect the steps in the oxygen transport pathway, thereby affecting participation in life and related activities (see Figure 17-1; see Chapter 2).22–24 For intervention to be directed specifically to the underlying problems, the physical therapist needs to consider several levels of analysis of the deficits contributing to impaired or threatened oxygen transport. To be proficient in such analysis, the physical therapist must have a thorough knowledge of the multiple factors that contribute to normal gas exchange and those that contribute to abnormal gas exchange. This knowledge base includes a thorough understanding of the relevant anatomy and physiology; the multisystem and integrative pathophysiology; the impact of medical, surgical, and nursing procedures; the effects of various laboratory tests and procedures; and the impact of pharmacological agents on cardiovascular and pulmonary function (Box 17-1). Assessment of oxygen transport reserve and reserve capacity is fundamental to the management of all patients25 and their risk factors,26 regardless of disease acuity. Routine procedures contribute to fluctuations in oxygen demands.27 Maximizing the ratio of oxygen delivery to consumption improves clinical outcomes in patients who range from being medically stable to being unstable.28,29,30 For a given patient, the cardiovascular and pulmonary physical therapist prescribes intervention by extracting the relevant information from the history, the laboratory tests and investigative procedures, and the assessment (Box 17-2; see Part II). Although physical therapists are primarily noninvasive practitioners, they use and request the results of invasive tests and investigations in their assessments and evaluations. Problems are prioritized on the basis of the relative magnitude of each problem’s threat or effect on oxygen transport limitation, along with the evidence supporting the effectiveness of various noninvasive interventions in addressing each diagnosis or problem. Once the mechanisms of the cardiovascular and pulmonary dysfunction have been identified, specific interventions are selected and prioritized and the prescriptive parameters of each intervention are then defined. With respect to education, a learning assessment is an essential component of the overall assessment; it identifies health status knowledge deficits and prescribes learning interventions consistent with the patient’s needs (see Chapter 28). Anatomic and physiological limitations are the individual’s overall deficits in oxygen transport and those that specifically arise at the individual steps in the pathway. Examples of the limitations at each step in the pathway appear in Tables 17-2 and 17-3. Table 17-2 Examples of Limitations and Threats to the Steps in the Oxygen Transport Pathway Altered central nervous system (CNS) afferent input and control of breathing
Maximizing Outcomes
Relating Interventions to an Individual’s Needs
International Classification of Functioning, Disability and Health
Participation
Type of Tool
Name of Specific Tools
Developers
General well-being scales, questionnaires, profiles, inventories
Medical Outcomes Study, Short Form (SF-36)
Stewart et al, 19882
Sickness Impact Profile (SIP)
Gibson et al, 19753
Quality of Well-Being Scale
Kaplan et al, 19844
Quality of Life Systemic Inventory
McGavin et al, 19775
Nottingham Health Profile
Hunt et al, 19806
Dartmouth Primary Care Cooperative Information
Wasson et al, 19927
Multidimensional Health Locus of Control Inventory
Wallston and Wallston, 19818
Symptom Questionnaire
Kellner, 19879
Cardiac-specific scales and questionnaires
Minnesota Living with Heart Failure Questionnaire
Rector et al, 198710
Outcomes Institute Angina Type Specification
Rogers et al, 199411
Quality of Life after Myocardial Infarction
Oldridge et al, 199112
Pulmonary-specific scales and questionnaires
Chronic Respiratory Disease Questionnaire
Guyatt et al, 198713
St. George’s Respiratory Questionnaire
Jones et al, 199214
Pulmonary Functional Status Scale
Weaver and Narsavage, 199215
Pulmonary Functional Status and Dyspnea Questionnaire
Lareau et al, 199416
Living with Asthma Questionnaire
Hyland, 199117
Cardiac rehabilitation questionnaire
EuroQol Questionnaire
Schweikert et al, 200618
Heart disease questionnaire
MacNew Heart Disease Quality of Life Questionnaire (MacNew)
Höfer et al, 200419
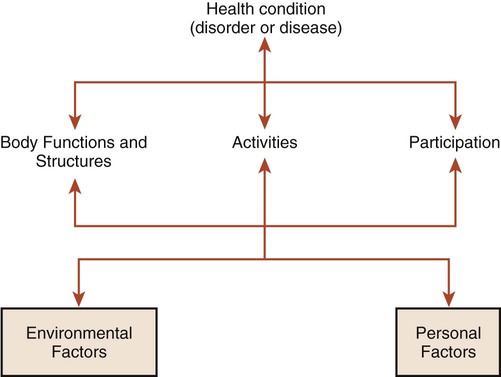
Activity
Structure and Function
 What are the problems with respect to participation, activity, and structure and function (impairments)? What are the interrelationships among these problems? (Remember: The interrelationships will be specific to the individual).
What are the problems with respect to participation, activity, and structure and function (impairments)? What are the interrelationships among these problems? (Remember: The interrelationships will be specific to the individual).
 What is the prognosis—with and without intervention?
What is the prognosis—with and without intervention?
 What is the relationship between the prognosis for each problem and the objectives of intervention and prescription?
What is the relationship between the prognosis for each problem and the objectives of intervention and prescription?
 What are the intervention priorities, and why?
What are the intervention priorities, and why?
 What are the interventions of choice, and why?
What are the interventions of choice, and why?
 What are the prescriptive parameters for each, and why? How should they be sequenced, and why?
What are the prescriptive parameters for each, and why? How should they be sequenced, and why?
 What is the course of intervention, and why? What are the requirements for follow-up in the short and long term, and why?
What is the course of intervention, and why? What are the requirements for follow-up in the short and long term, and why?
 What are the boundaries of knowledge that would guide a physical therapist to refer a patient to another health care professional (e.g., counselor, nutritionist, personal trainer, physician, psychologist)?
What are the boundaries of knowledge that would guide a physical therapist to refer a patient to another health care professional (e.g., counselor, nutritionist, personal trainer, physician, psychologist)?
What Is the Problem?
The Diagnoses or Problems
Impaired Oxygen Transport
Area of Limitation
Specific Threats
Central control of breathing
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


