The likelihood of success of conservative management of obstructive hypertrophic cardiomyopathy (HC) and the predictors of failure of conservative therapy are not known. We therefore evaluated the efficacy of an algorithm for the management of symptoms and predictors of failed conservative therapy in 249 consecutive symptomatic patients with obstructive HC referred to a dedicated HC program for management in general or for septal reduction therapy (SRT) in particular. There was considerable practice variation in the extent to which conservative therapy was optimized before referral for SRT. Over 3.7 ± 2.9-year follow-up, symptoms resolved with addition of or increase in dosage of a β blocker, calcium channel blocker, or disopyramide in 16%, 10%, and 10% of patients, respectively. Pacing with short atrioventricular delay controlled symptoms in 4 of 9 patients. In 63% of patients, conservative measures failed to control symptoms. Multivariate predictors of failure of conservative therapy were presence of New York Heart Association class III or IV symptoms (hazard ratio 2.0, 95% confidence interval 1.4 to 2.9, p = 0.001) and greater septal wall thickness (hazard ratio 1.06, 95% confidence interval 1.02 to 1.10, p = 0.003) at presentation. At time of presentation, 93 patients (37%) were already on optimal therapy and were referred for SRT. Of the remaining 156 patients who did not require immediate SRT, 93 (60%) were free from a recommendation for SRT at the end of the follow-up period. In conclusion, in symptomatic patients with obstructive HC, conservative therapy is successful in >1/3 of referred patients at 3.7-year follow-up, obviating SRT in these patients. Clinicians in programs offering SRT should optimize conservative therapy before recommending SRT.
Obstructive hypertrophic cardiomyopathy (HC) is characterized by asymmetrical, often genetically mediated, hypertrophy of the left ventricle with a left ventricular (LV) outflow tract gradient ≥30 mm Hg at rest or with provocation. Guidelines for evaluation and management of HC were published recently. Some patients with obstructive HC develop debilitating symptoms despite medical management and are often referred for septal reduction therapy (SRT) with septal myectomy or alcohol septal ablation (ASA). Although SRT decreases at-rest and dynamic LV outflow tract gradient and improves New York Heart Association (NYHA) functional status in most patients, such invasive therapy is associated with mortality and morbidity. Intensification of conservative therapy may obviate an exposure of some patients to these risks. We therefore assessed the efficacy of algorithm-driven conservative management and sought to identify clinical predictors of conservative treatment failure in a consecutive series of symptomatic patients with obstructive HC.
Methods
We consecutively enrolled all patients evaluated in the Hypertrophic Cardiomyopathy Program of the Massachusetts General Hospital Heart Center from January 1, 1998 through December 31, 2010. Diagnosis of HC was based on identification of a hypertrophied nondilated left ventricle in the absence of another cardiac or systemic disease capable of producing the observed magnitude of hypertrophy. Obstructive HC was defined as an LV outflow tract gradient under basal conditions and/or on provocation (with Valsalva maneuver or exercise) ≥30 mm Hg. Patients were referred to the Hypertrophic Cardiomyopathy Program by internists or cardiologists for HC evaluation and management in general or for SRT in particular.
Our general approach to the management of obstructive HC is summarized in a previously proposed algorithm ( Figure 1 ). This strategy was applied by a core group of physicians and nurse practitioners over a 13-year period of clinical practice.
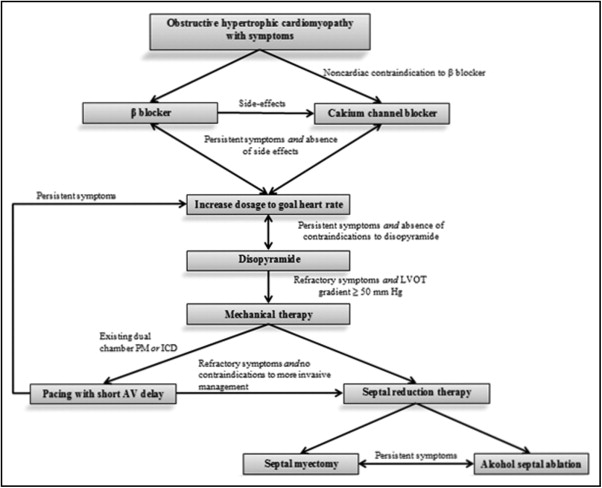
Patients presenting with obstructive HC and symptoms were initially offered a β blocker. Dose titration was governed by symptom control, side effects, and heart rate (goal 50 to 60 beats/min if needed for amelioration of symptoms). In some cases, we discontinued diuretic or vasodilator medications. In patients with noncardiac contraindications to β blockade such as severe asthma and in those requiring discontinuation of β blockade because of side effects, we substituted a nondihydropyridine calcium channel blocker, usually verapamil, similarly titrated to symptoms, side effects, and heart rate. In patients with symptoms refractory to optimal dosages of these medications, we added the class IA antiarrhythmic disopyramide in the absence of a contraindication to this medication. Contraindications to the use of disopyramide included corrected QT prolongation and (because of the drug’s anticholinergic effects) closed angle glaucoma. We also did not administer the drug to men who were elderly or had symptoms of urinary retention or to patients with difficult-to-control hypertension (because the drug is a vasoconstrictor). We obtained electrocardiograms 2 weeks after initiation of disopyramide or an increase in dosage for monitoring of the corrected QT interval. In accordance with American College of Cardiology Foundation/American Heart Association task force practice guidelines, we adjusted therapy to maintain the corrected QT interval <520 ms. Anticholinergic side effects such as dry mouth and constipation were managed with pyridostigmine. Patients with symptoms refractory to medical therapy who had a dual-chamber pacemaker or implantable cardioverter–defibrillator already in place were managed with a trial of pacing with short atrioventricular delay to pre-excite the LV apex. Patients were considered to have failed conservative management if they continued to have symptoms that interfered substantially with their quality of life despite these therapies; such patients were offered SRT.
The primary end point of the study was failure of conservative therapy to control symptoms, leading to a recommendation for SRT. Continuous variables are reported as mean ± SD and were compared using Student’s t test after confirmation of normality. Dichotomous and categorical variables were compared using chi-square test. We first conducted univariate comparisons of all baseline characteristics for patients in whom conservative therapy failed versus those in whom it succeeded. After confirmation that the proportionality assumption was met, we constructed a Cox proportional hazard model to assess multivariable-adjusted predictors of failed conservative treatment. Model variables were initially chosen by clinical relevance, selecting those that were significant predictors at an alpha of 0.05. We subsequently used backward elimination to remove variables found not to be significantly associated with SRT at an alpha of 0.1. We used SPSS 17.0 (SPSS, Inc., Chicago, Illinois) for all analyses.
Results
We evaluated 542 consecutive patients, of whom 297 (55%) had at-rest or inducible LV outflow tract obstruction. Of the 297 patients, 48 (16%) were free of symptoms at presentation. The other 249 patients who required further therapy constitute the study cohort. Characteristics of these 249 patients are listed in Table 1 . Of the 249 patients, 44 (18%) were not on any form of medical therapy. The follow-up period was 3.7 ± 2.9 years. Ultimately successful treatment for the 249 patients comprising the study cohort is depicted in Figure 2 . Overall, 93 patients (37%) were free from a recommendation for SRT at the end of the study period.
| Variable | All | General Evaluation | SRT | p Value ‡ |
|---|---|---|---|---|
| (n = 249) | (n = 125) | (n = 124) | ||
| Age (years), mean ± SD | 58 ± 15 | 57 ± 14 | 59 ± 15 | 0.318 |
| Men | 55% | 58% | 53% | 0.487 |
| Atrial fibrillation | 22% | 20% | 23% | 0.517 |
| New York Heart Association class III or IV | 66% | 47% | 84% | <0.001 |
| Medications on presentation | ||||
| β Blocker | 64% | 58% | 69% | 0.072 |
| Nondihydropyridine calcium channel blocker | 31% | 23% | 38% | 0.012 |
| Disopyramide | 12% | 6% | 18% | 0.003 |
| Diuretic | 20% | 12% | 8% | 0.167 |
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 13% | 16% | 10% | 0.262 |
| Dihydropyridine calcium channel blocker | 2% | 4% | 1% | 0.213 |
| Echocardiographic measurements | ||||
| Left ventricular outflow tract gradient at rest (mm Hg), mean ± SD | 63 ± 42 | 57 ± 42 | 69 ± 40 | 0.014 |
| Inducible left ventricular outflow tract gradient (mm Hg), mean ± SD | 89 ± 40 | 80 ± 39 ⁎ | 100 ± 40 † | 0.001 |
| Left ventricular outflow tract gradient ≥30 mm Hg at rest | 75% | 68% | 82% | 0.015 |
| Left ventricular outflow tract gradient ≥50 mm Hg at rest | 57% | 50% | 65% | 0.012 |
| Ventricular septum thickness (mm), mean ± SD | 19 ± 4 | 18 ± 4 | 20 ± 4 | 0.005 |
| Posterior wall thickness (mm), mean ± SD | 13 ± 3 | 13 ± 3 | 13 ± 3 | 0.258 |
| Ventricular septum:posterior wall thickness | 1.5 ± 0.4 | 1.5 ± 0.4 | 1.5 ± 0.5 | 0.478 |
| Referral source | ||||
| Cardiologist | 83% | 71% | 95% | <0.001 |
| Outcome | ||||
| Managed conservatively | 37% | 54% | 20% | <0.001 |
‡ Based on chi-square or t test comparing general evaluation and septal reduction therapy groups.

One hundred twenty-five patients (50%) were referred for general HC evaluation and management, and the remaining 124 (50%) were referred specifically for consideration of SRT; differences between the 2 populations are presented in Table 1 . Compared to patients referred for general evaluation, those referred for SRT had more advanced symptoms, were more often taking negative inotropic drugs, had higher LV outflow tract gradients, and had a greater degree of septal hypertrophy.
Of the 249 patients who had symptoms on presentation to our program, 90 (36%) were not taking a β blocker on presentation, of whom 47 had never received a β blocker. Beta blockers were absent on presentation in 31% of patients referred for SRT. Beta blockers were not instituted in patients with contraindications to or in those with previous adverse reactions to medications in this class. Of the 249 symptomatic patients, we started a β blocker in 47 patients and increased β blocker dosage in 45. Symptoms resolved with these measures in 40 of 92 patients (43%). Of the remaining 52 patients, symptoms remitted with substitution of a calcium channel blocker in 2, with addition of or increase in dosage of disopyramide in 7, and with short atrioventricular delay pacing in 3. For the remaining 40 patients, we recommended SRT.
Of the 249 symptomatic patients, 76 were taking a calcium channel blocker. Of these, 34 were also taking a β blocker. Thus, 42 of 249 symptomatic patients (17%) were taking a calcium channel blocker in the absence of β blockade. Of these 42 patients, symptoms remitted with an increase in calcium channel blocker dosage in 5, with substitution of a β blocker for the calcium channel blocker in 8, and with addition of or increase in disopyramide dosage in 4. SRT was recommended for the remaining 25 patients.
Twenty-nine of the 249 patients (12%) who were symptomatic at initial presentation were taking disopyramide. Of these, 22 patients (76%) were referred by a cardiologist and 25 (86%) were in NYHA class III or IV. Of these 29 patients, symptoms remitted with an increase in disopyramide dosage in 1, with institution of or intensification of β blockade in 1, and with addition of a calcium channel blocker in 2. SRT was recommended for the remaining 25 patients. In all, 27 of 249 symptomatic patients (11%) were initially managed with institution of (n = 24) or intensification of (n = 3) treatment with disopyramide. Of these 27 patients, symptoms resolved on disopyramide in 12 (44%); of these, 5 were also on a β blocker and a calcium channel blocker.
Nine patients with previously implanted dual-chamber devices underwent trials of short atrioventricular delay pacing in the course of their management. This treatment method was successful in controlling symptoms in 4 of these 9 patients (44%). Mean age of these patients was 63 years. All 4 patients were taking a β blocker, and 1 of the 4 was also taking disopyramide.
Of the 249 patients, 93 (37%) were on optimal conservative therapy at time of presentation, with ongoing symptoms. Of these 93 patients, 76 (82%) were taking a β blocker, 34 (37%) a calcium channel blocker, and 20 (22%) disopyramide. SRT was recommended for these 93 patients. Over the study duration, conservative management eventually failed in 63 additional patients (25% of original 249 symptomatic patients) who were therefore also offered SRT. Of the 124 patients referred specifically for consideration of SRT, 53 (43%) were initially managed conservatively. Of these 53 patients, conservative management ultimately failed in 28 (53%); these patients were offered SRT. In the remaining 25 patients (20% of those initially referred for SRT), conservative management obviated SRT. Thus, freedom from SRT in patients initially managed conservatively after being referred for SRT was 47%.
Of the 249 symptomatic patients, 156 (64%) had symptoms that were ultimately refractory to optimal conservative therapy. By univariate analysis, these patients were more likely to be in NYHA class III or IV and to be taking disopyramide on presentation, had higher LV outflow tract gradients at rest and with provocation, and had a greater degree of septal hypertrophy than did those whose symptoms were ultimately controlled with conservative management ( Table 2 ). In multivariable modeling, predictors of failure of conservative therapy were presence of NYHA class III or IV symptoms (hazard ratio [HR] 2.0, 95% confidence interval [CI] 1.4 to 2.9, p = 0.001) and greater septal wall thickness (HR 1.06, 95% CI 1.02 to 1.10, p = 0.003) at presentation.
| Variable | Success | Failure | p Value |
|---|---|---|---|
| (n = 93) | (n = 156) | ||
| Age (years), mean ± SD | 59 ± 14 | 58 ± 15 | 0.492 |
| Men | 55% | 56% | 0.886 |
| Atrial fibrillation | 24% | 21% | 0.561 |
| New York Heart Association class III or IV | 43% | 79% | <0.001 |
| Medications on presentation | |||
| β Blocker | 56% | 69% | 0.045 |
| Nondihydropyridine calcium channel blocker | 27% | 33% | 0.336 |
| Disopyramide | 4% | 16% | 0.009 |
| Diuretic | 28% | 16% | 0.026 |
| Echocardiographic measurements | |||
| Left ventricular outflow tract gradient at rest (mm Hg), mean ± SD | 55 ± 41 | 68 ± 42 | 0.023 |
| Inducible left ventricular outflow tract gradient (mm Hg), mean ± SD | 77 ± 35 ⁎ | 97 ± 42 † | <0.001 |
| Left ventricular outflow tract gradient ≥30 mm Hg at rest | 69% | 78% | 0.91 |
| Left ventricular outflow tract gradient ≥50 mm Hg at rest | 47% | 64% | 0.013 |
| Inducible left ventricular outflow tract gradient ≥50 mm Hg | 71% ⁎ | 92% † | <0.001 |
| At-rest or Inducible left ventricular outflow tract gradient ≥50 mm Hg | 76% | 91% | 0.002 |
| Ventricular septum thickness (mm) mean ± SD | 18 ± 3 | 20 ± 4 | 0.015 |
| Posterior wall thickness (mm), mean ± SD | 13 ± 2 | 13 ± 3 | 0.094 |
| Ventricular septum:posterior wall thickness | 1.5 ± 0.4 | 1.5 ± 0.5 | 0.52 |
| Referral source | |||
| Cardiologist | 76% | 87% | 0.029 |
| Referral reason | |||
| Septal reduction therapy | 27% | 63% | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


