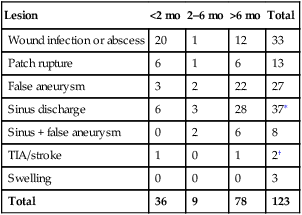
There was a biomodal pattern of symptoms in the 123 patients with patch infection (Table 1). Thirty-six patients (29%) presented within 2 months of their primary CEA, and 78 (63%) presented after 6 months or more had elapsed. Patients presenting within 2 months were more likely to present with an abscess or complex wound infection (20/36, 56%) or patch rupture (6/36, 17%). A minority presented with false aneurysm formation (3/36, 8%). By contrast, patients presenting after more than 6 months had elapsed since their CEA were significantly more likely to present with false aneurysm (22/78, 28%) or chronic sinus discharge (28/78, 36%) and were unlikely to present with either a wound abscess (12/78, 15%) or patch rupture (6/78, 8%). Overall, only four of the 123 patients (3%) presented with either a transient ischemic attack (TIA) or stroke. TABLE 1 Mode of Presentation of 75 Cases of Prosthetic Patch Infection Relative to Timing after Surgery TIA, Transient ischemic attack. ∗Two of these patients presented with TIA as well. †Paper did not specify any other presentation but recorded positive cultures. It is usually accepted that most prosthetic infections begin at the time of surgery. In the review of 123 cases, it was possible to correlate timing of onset of symptoms with the presence or absence of wound complications in the perioperative period in the majority of patients (Table 2). No information was provided in 46 patients. Out of the remaining 77, 32 (42%) reported either a wound infection or hematoma in the perioperative period. However, the prevalence varied according to the delay to presentation, with 26 of 31 (84%) and 3 of 7 (43%) of patients presenting at less than 2 months or 2 to 6 months (respectively), having documented evidence of a wound complication in the perioperative period compared with only 3 of 39 (8%) patients presenting late. TABLE 2 Wound Complications 30 Days after Carotid Endarterectomy and Their Relationship with Prosthetic Patch Infection
Management of the Infected Carotid Artery Patch
Clinical Presentation
Lesion
<2 mo
2–6 mo
>6 mo
Total
Wound infection or abscess
20
1
12
33
Patch rupture
6
1
6
13
False aneurysm
3
2
22
27
Sinus discharge
6
3
28
37∗
Sinus + false aneurysm
0
2
6
8
TIA/stroke
1
0
1
2†
Swelling
0
0
0
3
Total
36
9
78
123
Relationship with Perioperative Infection
TIMING OF PRESENTATION WITH PATCH INFECTION
Complication
<2 mo
2–6 mo
>6 mo
Total
No data provided
5
2
39
46
Wound infection
19
3
1
23
Hematoma
7
0
2
9
No wound problem
5
4
36
45
Fraction with a wound complication
26/31 (84%)
3/7 (43%)
3/39 (8%)
32/77 (42%) ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Management of the Infected Carotid Artery Patch
