Malignant Pleural Effusion
Presentation
A 57-year-old woman presents with increasing shortness of breath during the past 3 months. Her medical history includes breast cancer, for which she underwent a left modified radical mastectomy, a prophylactic right mastectomy, and first-stage breast reconstruction. The patient received chemotherapy and radiation initially and is currently receiving tamoxifen. The patient is hemodynamically stable. Respiratory rate is 12 breaths/min. Breath sounds are diminished on the right.
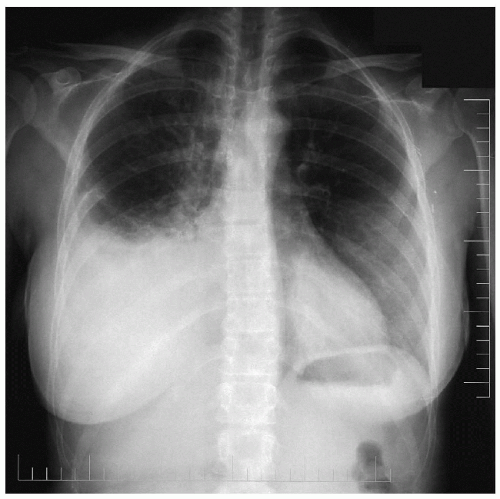
▪ Chest X-ray Report
There is a large right pleural effusion. There is also linear atelectasis at the base of the right lung consistent with compression atelectasis.
The left lung field is clear. There are surgical clips in the left axilla and bilateral breast implants.
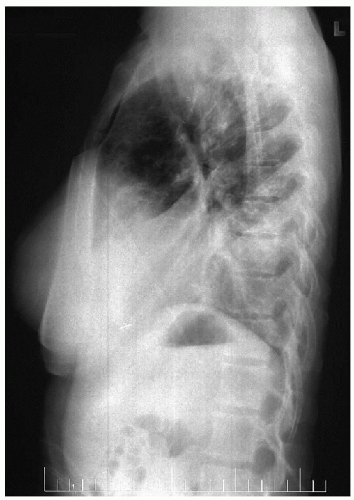
CT Scan Report
Right pleural effusion consistent with the findings on the chest x-ray. The lung fields are clear of masses and infiltrates; however, compressive atelectasis is present in the right lower lobe.
Differential Diagnosis
The diagnosis of pleural effusions should be divided into two categories: transudative and exudative effusions. Based on the type of effusion and the clinical history, a differential diagnosis is formulated. The distinction between transudates and exudates can be made based on the criteria proposed by Light and colleagues in 1972. Using Light’s criteria, a pleural effusion is considered an exudate when:
Pleural fluid lactate dehydrogenase (LDH) is greater than two thirds of the upper limit of normal for serum LDH.
The pleural fluid LDH-to-serum LDH ratio is greater than 0.6.
The pleural fluid protein-to-serum protein ratio is greater than 0.5.
Forty-three percent of patients with an exudate have a malignancy, and 83% of patients with a transudate have congestive heart failure. Other causes of transudative effusion include cirrhosis, nephrotic syndrome, myxedema, peritoneal dialysis, hypoproteinemia, Meigs’ syndrome, and sarcoidosis. Exudative effusions are caused by neoplastic disease, infectious disease, pulmonary infarction, collagen vascular diseases (rheumatoid arthritis, systemic lupus erythematosus), gastrointestinal diseases (pancreatitis, pancreatic pseudocyst, esophageal rupture, subphrenic abscess, hepatic abscess), trauma (hemothorax, chylothorax), and other causes (after radiation therapy and after myocardial infarction).
Other laboratory tests can be performed on the pleural fluid to help narrow the differential diagnosis. White blood cell counts greater than 10,000/mm3 suggest an empyema, whereas red blood cell counts greater than 100,000/mm3 suggest trauma, pulmonary infarction, or malignancy. Elevated amylase levels are often found with esophageal perforations, acute pancreatitis, and a ruptured pancreatic pseudocyst. The diagnosis of chylothorax can be made by demonstrating elevated levels of cholesterol, triglycerides, and chylomicrons in the pleural effusion. If the glucose in the pleural fluid is lower than in the serum, the diagnoses of tuberculosis, rheumatoid arthritis, empyema, and malignancy should be entertained. A low pleural fluid (pH less than 7.2) suggests contamination with bacteria. A parapneumonic effusion containing glucose greater than 40g/dL, pH greater than 7.2, and LDH greater than 1,000 units/L would likely resolve with treatment of the pneumonia. However, if the glucose is less than 40g/dL or the pH is less than 7.2, a thoracostomy tube is generally necessary to treat the effusion. Some exceptions include rheumatoid arthritis, tuberculosis, and malignant effusions, in which the pH is regularly less than 7.2 and a thoracostomy tube is not necessary.
Cytologic examination should be routinely performed on pleural fluid specimen. In patients with malignant pleural effusions, the initial specimen reveals a diagnosis of malignancy 60% of the time. Accuracy increases to 90% when three separate specimens are obtained.
Cytologic examination should be routinely performed on pleural fluid specimen. In patients with malignant pleural effusions, the initial specimen reveals a diagnosis of malignancy 60% of the time. Accuracy increases to 90% when three separate specimens are obtained.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree