The aim of this study was to investigate the incidence of composite short-term and long-term major adverse upper gastrointestinal (UGI) events (MAUGIEs; defined as gastric ulcer, duodenal ulcer, gastroduodenal ulcer, or UGI bleeding) in patients with acute ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention and routinely received dual-antiplatelet therapy. From May 2002 to September 2010, a total of 1,368 consecutive patients who experienced ST-segment elevation myocardial infarction and underwent primary percutaneous coronary intervention were prospectively enrolled in the study. The incidence of in-hospital UGI bleeding complications and composite MAUGIEs was 8.9% and 9.9%, respectively. The in-hospital mortality rate was significantly higher in patients with in-hospital MAUGIEs than in those without (p <0.001). Multivariate analysis showed that age, advanced Killip score (≥3), and respiratory failure were the strongest independent predictors of in-hospital composite MAUGIEs (all p <0.003). The cumulative composite of MAUGIEs after uneventful discharge in patients without adverse UGI events who continuously received dual-antiplatelet therapy for 3 to 12 months, followed by aspirin therapy, was 10.4% during long-term (mean 4.0 years) follow-up. In conclusion, the results of this study show a remarkably high incidence of composite short-term and long-term MAUGIEs in patients with ST-segment elevation myocardial infarction who underwent primary percutaneous coronary intervention and received routine dual-antiplatelet therapy. Age, advanced Killip score, and respiratory failure were significantly and independently predictive of in-hospital composite MAUGIEs.
The link between stress and peptic ulcer has been well recognized. Undoubtedly, the degree of stress patients experience in the setting of acute ST-segment elevation myocardial infarction (STEMI) is higher than in those with non-STEMI or unstable or stable angina pectoris. It is rational, therefore, to expect a higher incidence of stress ulcer in patients with STEMI compared to those in other clinical settings. Surprisingly, most clinical trials investigating the association between dual-antiplatelet therapy and upper gastrointestinal (UGI) bleeding have focused on patients with unstable angina or non-STEMI instead of those with STEMI. Indeed, peptic ulcer with or without UGI bleeding in patients who undergo primary percutaneous coronary intervention (PCI) for STEMI has seldom been reported. Furthermore, the long-term incidence of in-stent thrombosis in patients with STEMI after the withdrawal of aspirin because of peptic ulcer with or without UGI bleeding has not been reported, especially in Chinese patients. Accordingly, in the present study, we investigated the incidence of composite short-term and long-term major adverse UGI events (MAUGIEs; defined as gastric ulcer, duodenal ulcer, gastrointestinal ulcer, or UGI bleeding) in patients with STEMI who underwent primary PCI and were receiving dual-antiplatelet therapy, and we also examined the incidence of in-stent thrombosis after the withdrawal of aspirin because of peptic ulcer or UGI bleeding on long-term follow-up.
Methods
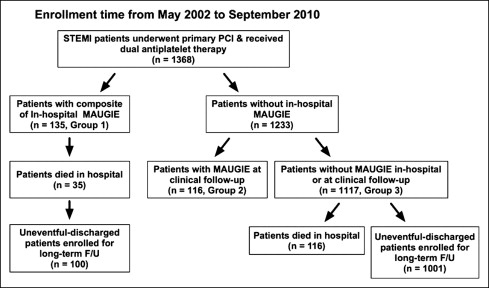
Since May 1993, all patients with acute STEMI at our institute have been considered eligible for primary PCI. From May 2002 to September 2010, a total of 1,368 consecutive patients of all ages with acute STEMI of <12 hours in duration underwent primary PCI ( Figure 1 ). Of these 1,368 patients, 135 (9.9%) experiencing in-hospital composite MAUGIEs were prospectively recruited for this study as group 1. Of the 1,233 patients (90.1%) without MAUGIEs, 116 (9.4%) died in the hospital. Thus, the remaining 1,117 patients without MAUGIEs during hospitalization were continuously followed up after discharge from the hospital. Of these 1,117 patients, 116 (10.4%) who experienced MAUGIEs during clinical follow-up served as group 2. Finally, those 1,117 patients who had no MAUGIEs in the hospital or during clinical follow-up served as group 3. Informed consent was obtained from each study subject. The institutional review committee on human research at our institution approved the study protocol.
Primary PCI was performed according to a protocol previously described. A transradial artery approach using a 6Fr arterial sheath is a routine procedure for acute STEMI at Kaohsiung Chang Gang Memorial Hospital, unless the results of Allen’s test are negative on both sides. A 6Fr Kimny guiding catheter (Boston Scientific Corporation, Maple Grove, Minnesota) was used for the diagnosis of coronary artery occlusion and primary PCI. Intra-aortic balloon pump support was performed using the femoral arterial approach in patients experiencing acute pulmonary edema associated with unstable condition or hemodynamic instability. Extracorporeal membrane oxygenation support was performed using the femoral arterial and vein approaches for patients who experienced profound cardiogenic shock. The procedure and protocol have been described in detail in our recent report.
STEMI was defined as (1) typical chest pain lasting >30 minutes with ST-segment elevation >1 mm in 2 consecutive precordial or inferior leads or (2) typical chest pain lasting >30 minutes with new-onset complete left bundle branch block. Procedural success was defined as a reduction to residual stenosis of <20% by balloon angioplasty or successful stent deployment at the desired position with residual stenosis <10%, followed by Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow in the infarct-related artery. Multivessel disease was defined as stenoses ≥50% in ≥2 major epicardial coronary arteries. Advanced Killip score was defined as ≥3 in patients upon presentation to emergency room.
UGI bleeding was defined as hemorrhage from the esophagus, stomach, or duodenum confirmed by means of endoscopic examination of the UGI tract or overt clinical manifestations of UGI bleeding (presence of tarry stool or coffee-ground substance from nasogastric tube) of unknown origin, with a documented decrease in hemoglobin of ≥2 g/dl within 48 hours. Peptic ulcer disease was defined as mucosal erosions ≥0.5 cm in the UGI tract.
All patients received a loading dose of clopidogrel (300 mg orally) in the emergency room, followed by a maintenance dose (75 mg/day orally) for ≥12 weeks if bare-metal stent deployment was performed or ≥12 months if drug-eluting stent implantation was the chosen procedure. Aspirin (100 mg/day orally) was given indefinitely to each patient. Other commonly prescribed medications also included angiotensin-converting enzyme inhibitors, statins, β-blockers, isornitrate, and diuretics.
A loading dose of tirofiban (30 μg/kg body weight) was administered to patients upon presentation to the emergency room, followed by a maintenance infusion of 0.15 μg/kg/min for 18 to 24 hours at the beginning of the study. However, tirofiban therapy was subsequently withheld because it failed to provide any additional benefit for patients with STEMI who underwent primary PCI. Therefore, only 17.6% of patients (241 of 1,368) received tirofiban therapy in this study.
The primary PCI program began at our institute in May 1993. For the purpose of this study, all patients who underwent primary PCI were prospectively recruited. Detailed in-hospital and follow-up data, including age, gender, coronary risk factors, Killip score on admission, peak level of creatinine phosphokinase, arrival time, duration from puncture to first balloon inflation, reperfusion time, duration of procedure, pre- and post-PCI TIMI flow grades, angiographic results, number of diseased vessels, in-hospital adverse events, in-hospital mortality, and long-term adverse events, were obtained. These data were collected prospectively and entered into a digital database.
Data are expressed as mean ± SD or as percentages. Differences in continuous variables were analyzed using independent Student’s t tests and in categorical variables using chi-square tests. The baseline variables were used for univariate analysis. Multiple stepwise logistic regression analysis was used for independent predictors of in-hospital MAUGIEs and mortality. A multiple stepwise Cox proportional-hazards regression model was adopted to identify independent predictors of long-term mortality. Statistical analysis was performed using SPSS for Windows version 13 (SPSS, Inc., Chicago, Illinois). Two-sided p values ≤0.05 were considered statistically significant.
Results
Group 1 patients were significantly older, with a higher frequency of diabetes mellitus, higher white blood cell counts, higher serum levels of creatinine and peak levels of creatinine phosphokinase, a lower frequency of male gender, and lower levels of hemoglobin, than those in group 2 and group 3, but there were no significant differences between the patients in group 2 and group 3 ( Table 1 ). Group 1 patients had significantly lower serum levels of total cholesterol than those in group 3, but there were no differences between the patients in group 1 and group 2 and between the patients in group 2 and group 3.
| Variable | MAUGIEs | p Value | ||
|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | ||
| (n = 135) † | (n = 116) † | (n = 1,117) † | ||
| Age (years) | 67.3 ± 12.8 ∥ | 62.3 ± 11.4 ¶ | 60.5 ± 12.5 ¶ | <0.001 |
| Men | 97 (71.9%) ∥ | 102 (87.9%) ¶ | 925 (82.8%) ¶ | 0.002 |
| Current smoking | 36 (26.7%) | 37 (31.9%) | 377 (33.8%) | 0.238 |
| Hypertension | 78 (57.8%) | 66 (56.9%) | 604 (54.1%) | 0.632 |
| Diabetes mellitus | 63 (46.7%) ∥ | 43 (37.1%) ¶ | 383 (34.3%) ¶ | 0.017 |
| Previous stroke | 12 (8.9%) | 8 (6.9%) | 85 (7.6%) | 0.824 |
| Previous myocardial infarction | 5 (3.7%) | 7 (6.0%) | 52 (4.7%) | 0.681 |
| Body mass index (kg/m 2 ) | 24.9 ± 3.9 | 25.0 ± 3.6 | 25.4 ± 3.7 | 0.244 |
| Total cholesterol level (mg/dl) | 171.2 ± 49.3 ∥ | 184.2 ± 39.0 ∥ ¶ | 189.1 ± 45.1 ¶ | <0.001 |
| White blood cell count (×10 3 /dl) ‡ | 12.4 ± 5.0 ∥ | 10.3 ± 3.3 ¶ | 11.1 ± 3.9 ¶ | <0.001 |
| Creatinine level (mg/dl) ‡ | 2.03 ± 1.86 ∥ | 1.41 ± 1.23 ¶ | 1.34 ± 1.22 ¶ | <0.001 |
| Total peak level of creatinine phosphokinase (IU/ml) ‡ | 3,703.8 ± 5,061.0 ∥ | 2,463.7 ± 2,608.5 ¶ | 2,761.8 ± 2,806.8 ¶ | 0.003 |
| Hemoglobin (g/dl) ‡ | 13.2 ± 2.5 ∥ | 14.1 ± 2.0 ¶ | 14.3 ± 2.0 ¶ | <0.001 |
| Platelet count (×10 3 /dl) ‡ | 219.5 ± 81.9 | 209.8 ± 55.8 | 220.3 ± 66.7 | 0.290 |
| Systolic blood pressure (mm Hg) | 116.2 ± 36.3 ∥ | 129.7 ± 38.3 ¶ | 129.0 ± 35.4 ¶ | 0.001 |
| Diastolic blood pressure (mm Hg) | 67.5 ± 21.3 ∥ | 77.8 ± 20.7 ¶ | 76.4 ± 20.4 ¶ | <0.001 |
| Multivessel disease | 90 (66.7%) ∥ | 64 (55.2%) ¶ | 607 (54.3%) ¶ | 0.024 |
| Tirofiban use | 24 (17.8%) | 17 (14.7%) | 200 (17.9%) | 0.668 |
| Advanced Killip score (≥3) | 78 (57.8%) ∥ | 21 (18.1%) ¶ | 253 (22.6%) ¶ | <0.001 |
| Stent implantation | 99 (73.3%) ∥ | 96 (82.8%) ¶ | 943 (84.4%) ¶ | 0.015 |
| Drug-eluting stent | 7 (5.2%) | 4 (3.4%) | 74 (6.6%) | |
| Bare-metal stent | 92 (68.1%) | 92 (79.3%) | 869 (77.8%) | |
| Procedural success | 112 (83.0%) ∥ | 111 (95.7%) ¶ | 1,046 (93.6%) ¶ | <0.001 |
| Intra-aortic balloon pump | 68 (50.4%) ∥ | 18 (15.5%) ¶ | 196 (17.5%) ¶ | <0.001 |
| Extracorporeal membrane oxygenation | 10 (7.4%) ∥ | 0 (0%) ¶ | 32 (2.9%) ¶ | 0.002 |
| Respiratory failure § | 59 (43.7%) ∥ | 2 (1.7%) ¶ | 129 (11.5%) # | <0.001 |
| Stroke during hospitalization | 5 (3.7%) | 1 (0.9%) | 15 (1.3%) | 0.090 |
| Duration of hospitalization (days) | 17.3 ± 20.6 ∥ | 6.0 ± 4.3 ¶ | 7.3 ± 9.9 ¶ | <0.001 |
| In-hospital mortality | 35 (25.9%) ∥ | 0 (0%) ¶ | 116 (10.4%) # | <0.001 |
| Cardiac death | 26 (19.3%) ∥ | 0 (0%) ¶ | 105 (9.4%) # | <0.001 |
| Noncardiac death | 9 (6.7%) ∥ | 0 (0%) ¶ | 11 (1.0%) # | <0.001 |
| Long-term cumulative mortality | 46 (34.1%) ∥ | 12 (10.3%) ¶ | 168 (15.0%) ¶ | <0.001 |
| Cardiac death | 31 (23.0%) ∥ | 4 (3.4%) ¶ | 123 (11.0%) # | <0.001 |
| Noncardiac death | 15 (11.1%) ∥ | 8 (6.9%) ¶ | 45 (4.0%) ¶ | 0.001 |
| Nonsteroidal anti-inflammatory drug use | 2 (1.5%) | 0 (0%) | 7 (0.6%) | 0.335 |
⁎ All patients who received dual-antiplatelet therapy (aspirin and clopidogrel) after primary PCI were enrolled in the present study.
† Group 1: presence of MAUGIEs (gastric ulcer, duodenal ulcer, gastroduodenal ulcer, or UGI bleeding) during hospitalization; group 2: without in-hospital MAUGIEs but with MAUGIEs at clinical follow-up; group 3: without MAUGIEs in hospital or at clinical follow-up.
‡ All data recorded upon presentation.
§ Acute respiratory failure with requirement for mechanical ventilator support.
∥,¶,# Significant difference (at 0.05 level) by Bonferroni’s multiple comparison procedure.
Group 1 patients had significantly lower systolic and diastolic blood pressures and higher frequencies of advanced Killip scores on initial presentation and cardiogenic shock with requirement for intra-aortic balloon pump and extracorporeal membrane oxygenation life support than those in groups 2 and 3, but there were no significant differences between the patients in groups 2 and 3. Moreover, the frequency of respiratory failure with requirement for mechanical ventilation was significantly higher in group 1 than in groups 2 and 3 and significantly higher in group 3 than in group 2.
Because of the absence of reflow phenomenon in the infarct-related artery and/or unfavorable clinical outcomes that might preclude the implantation of coronary stents in group 1 patients, the percentage of procedural success and the incidence of stent implantation were significantly lower in group 1 than in groups 2 and 3.
Group 1 patients had significantly longer durations of hospitalization and a higher long-term cumulative mortality rate than those in groups 2 and 3, but there were no significant differences between the patients in groups 2 and 3. The in-hospital mortality rate, including the incidence of noncardiac death or cardiac death, was also remarkably higher in group 1 than in groups 2 and 3. Moreover, compared to group 2, the in-hospital mortality rate was significantly higher in group 3.
The baseline variables listed in Table 1 were also analyzed using multiple stepwise logistic regression analysis and a Cox proportional-hazards regression model, and the results showed that the occurrence of composite MAUGIEs lacked significant independent predictive value for in-hospital mortality (odds ratio 0.678, 95% confidence interval 0.364 to 1.263, p = 0.221) and long-term mortality (hazard ratio 1.427, 95% confidence interval 0.982 to 2.072, p = 0.062).
To investigate whether the incidence of MAUGIEs and UGI bleeding had any difference between patients with and those without extracorporeal membrane oxygenation, intra-aortic balloon pump, or mechanical ventilator support, subgroup analysis was performed in the ( Table 2 ). The results demonstrated that the incidence of MAUGIEs and UGI bleeding were substantially increased in patients who received these forms of mechanical support.
| Variable | ECMO, IABP, or Ventilator Support | |||
|---|---|---|---|---|
| Overall Cohort | Yes | No | p Value † | |
| (n = 1,368) | (n = 316) | (n = 1,052) | ||
| MAUGIEs | 135 (9.9%) | 77 (24.4%) | 58 (5.5%) | <0.001 |
| UGI bleeding | 122 (8.9%) | 73 (23.1%) | 49 (4.7%) | <0.001 |
⁎ Gastric ulcer, duodenal ulcer, gastroduodenal ulcer, or UGI bleeding.
† Comparison between patients with and those without ECMO, IABP, or ventilator support.
Multiple stepwise logistic regression analysis of the variables listed in Table 1 showed that respiratory failure with the requirement for mechanical ventilation was the strongest independent predictor of the occurrence of composite MAUGIEs ( Table 3 ). Other factors, including old age, elevated serum creatinine level, and advanced Killip score, were also independently predictive of in-hospital composite MAUGIEs. In contrast, procedural success was a significant independent predictor of the absence of in-hospital composite MAUGIEs.



