Lymphatics of the Lungs
Thomas W. Shields
The lung has an extensive network of lymphatic vessels that are situated in the loose connective tissue beneath the visceral pleura, in the connective tissue in the interlobular septa, and in the peribronchial vascular sheaths.
In the pulmonary parenchyma, the lymphatic capillaries form extensive plexuses within the connective tissue sheaths that surround the airways and the blood vessels. The origin of these channels is believed to be at the level of the terminal and respiratory bronchioles, and they do not extend into the inter-alveolar septa, according to Okada and colleagues50 as well as Leak and Jamuar.29 The channels begin as blind-end tubes and saccules. As these channels extend proximally toward the hilar area associated with the enlarging airways and blood vessels, they have been designated as juxta-alveolar lymphatics by Lauweryns27 and Leak.28 These networks drain into larger collecting vessels with thicker walls and contain monocuspid, conical valves that direct the flow of lymph toward the hilar area in a centripetal direction. The physiologic mechanisms controlling this lymphatic flow are little understood.
Lymphatic channels that also drain the periphery of the lung lobules run in the lobular septa along with the pulmonary veins. With the occurrence of extra-alveolar interstitial edema, some of these may be recognized as Kerley’s B lines radiographically, as noted by Steiner.60
The extensive subpleural network drains primarily by the channels in the interlobular septa to the hilar area, but direct connections to the mediastinum have been recorded by Rouvière,59 Borrie,6,7 and Riquet52 as well as Riquet and associates.54 The channels in the lobular septa have multiple connections with the channels in the bronchovascular sheaths. These connecting channels are frequently ≤4 cm in length and lie midway between the hilus and the periphery of the lung. When distended, they are recognized as Kerley’s A lines.
Collections of lymphatic cells may be seen along the course of the lymphatic channels and within the bronchial structures, but recognizable intrapulmonary lymph nodes are identified only infrequently in contrast to the common presence of bronchopulmonary lymph nodes.
Pulmonary Lymph Nodes
The pulmonary lymph nodes are divided into the intrapulmonary and bronchopulmonary nodes. The latter are subdivided into the lobar and hilar lymph nodes.
Intrapulmonary Lymph Nodes
The intrapulmonary lymph nodes, when present, are located most often just beneath the visceral pleura. Rarely, a peripheral lymph node may present as a solitary peripheral nodule, as reported by Greenberg,17 Houk and Osborne,21 and Ehrenstein.13 In addition to these infrequent, radiographically identified intrapulmonary lymph nodes, Trapnell62 reported the identification of other intrapulmonary lymph nodes in the substance of the lung by a combined technique of injection of the subpleural lymphatics and subsequent radiologic evaluation of autopsy lung specimens. Intrapulmonary nodes were observed in 5 of 28 injected specimens, an incidence of 18%. The actual location of these nodes was undocumented. However, Trapnell63 was able to identify peripheral lymph nodes radiologically in only 1 of 92 inflated lungs obtained at autopsy, an incidence of just over 1%. Despite this early study, Dail11 reported that intraparenchymal lymph nodes could be identified in about 10% of resected lobes when they were sought, and Kradin and associates26 had previously recorded that all such nodes were anthracotic and were not encapsulated. In Kradin and associates’26 report, the identified lymph nodes were solitary in 65% of the cases and multiple in the remainder; in 22%, two lymph nodes were found, and in 12% three or more were identified. The multiple nodes may be in the same lobe in 40% of the cases in which they are found, but in 60%, the lymph nodes are located bilaterally. Most are in the size range of 0.5 to 1.0 cm; occasionally, nodes as large as 1.5 cm are identified. Only rarely is a larger one present. All these intraparenchymal lymph nodes are within 1 cm of the pleura, adjacent to it, or in an interlobular septum. With rare exception, these lymph nodes are found only in adults and are identified more commonly in individuals >50 years of age.
With high-resolution computed tomography (HRCT), some of the small lesions identified in patients with multiple metastases to the lung are proved subsequently to be small peripheral lymph nodes. Ohbuchi and associates48 reported excision by video-assisted thoracic surgery (VATS) of 10 intrapulmonary lymph nodes suspected as malignant lesions, either primary or secondary, over a 1-year period. The average size of the pulmonary nodes was 5.9 mm, and all were located in the lower lobes: seven on the left and three on the right. Over a 2-year period in nine patients, Nagahiro and colleagues37 resected 13 intrapulmonary lymph nodes that had been identified on chest radiographs in three patients and on HRCT in the other six. The characteristics of these nodes on HRCT were that the borders
were sharp, the shapes were ovoid, all were located in the lower portion of the lungs in a subpleural location, and the interval density was high and homogeneous. No borders were irregular, although short spicules could be present, and none contained cavities or calcifications. As the aforementioned authors—as well as Ohbuchi48 and Yokomise69 and their associates—have pointed out, these lesions must be differentiated from small malignant nodules.
were sharp, the shapes were ovoid, all were located in the lower portion of the lungs in a subpleural location, and the interval density was high and homogeneous. No borders were irregular, although short spicules could be present, and none contained cavities or calcifications. As the aforementioned authors—as well as Ohbuchi48 and Yokomise69 and their associates—have pointed out, these lesions must be differentiated from small malignant nodules.
Bronchopulmonary Lymph Nodes
Nagaishi38 noted that segmental lymph nodes are related to the bifurcation of the segmental bronchi or may lie in the bifurcation of the branches of the associated pulmonary arteries and may extend out to the fifth- or sixth-order segmental bronchi.
The lobar bronchopulmonary lymph nodes are found at the angles formed by the origins of the various lobar bronchi and lie in close association with the bronchus or the adjacent pulmonary vessels. The hilar lymph nodes are situated alongside the lower portions of the main bronchi or the respective pulmonary artery and the pulmonary veins lying within the visceral pleural reflections.
The number of bronchopulmonary lymph nodes is variable. These lymph nodes more frequently are present in greater numbers in children than in adults. Borrie7 suggests that the maximal development of these nodes is reached by the end of the first decade of life; then these lymph nodes gradually atrophy and disappear during adulthood. The presence of pulmonary infection or malignancy greatly affects the number of bronchopulmonary lymph nodes that may be identified.
In a study of 200 operative specimens of lungs containing lung cancer, Borrie7 identified lymph nodes in 13 locations in the right lung and 15 in the left that are now considered bronchopulmonary lymph nodes. These sites are listed in Table 6-1 and are shown schematically in Figures 6-1 and 6-2. The incidence of bronchopulmonary lymph nodes present in each location is listed in Table 6-2.
Table 6-1 Distribution of Bronchopulmonary Lymph Nodes | ||||||
|---|---|---|---|---|---|---|
| ||||||
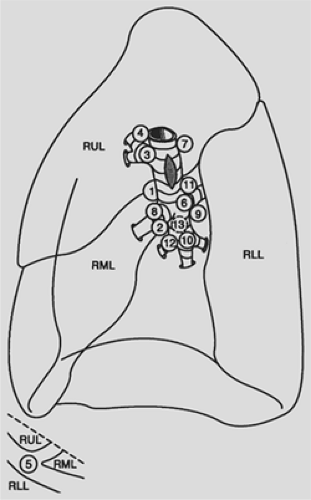 Figure 6-1. Bronchopulmonary lymph nodes of the right lung. Drawing of the medial aspect of the right lung shows the 13 most common locations of lymph nodes identified in 93 specimens by Borrie. The sites are numbered in the order of decreasing frequency in which lymph nodes were identified in each respective site (see Tables 6-1 and 6-2). Inset at bottom shows the lateral view of the junction of the oblique and transverse fissures. At this site, lymph nodes are lateral to the origins of the middle and lower lobe branches of the right pulmonary artery. RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe. (Redrawn from Borrie J. Lung Cancer. Surgery and Survival. New York: Appleton-Century-Crofts, 1965.) |
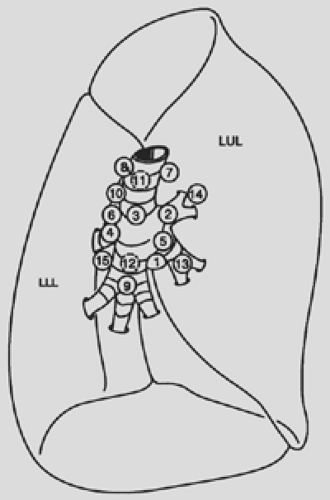 Figure 6-2. Bronchopulmonary lymph nodes of the left lung. Drawing of the medial aspect of the left lung shows the 15 most common locations of bronchopulmonary lymph nodes identified in 101 specimens by Borrie. The sites are numbered in the order of decreasing frequency in which lymph nodes were identified in each respective site (see Tables 6-1 and 6-2). LLL, left lower lobe; LUL, left upper lobe. (Redrawn from Borrie J. Lung Cancer. Surgery and Survival. New York: Appleton-Century-Crofts, 1965. |
Hilar Lymph Nodes
The hilar lymph nodes are contiguous with the lobar lymph nodes distally as well as with the mediastinal lymph nodes proximally. The hilar lymph nodes lying superior to the right mainstem bronchus classically have been considered to extend up to the inferior border of the azygos vein, but this concept was questioned by Tisi and associates61 in their recommendations about the location of the various mediastinal lymph node stations. The lymph nodes medial to the right mainstem bronchus may be considered as hilar nodes when located away from the tracheal carina and within the visceral pleural sheath, but as they become subjacent to this structure, they are best termed subcarinal lymph nodes and thus belong to the lymph nodes of the mediastinal compartment.
On the left side, the anatomic separation between the hilar and the mediastinal lymph nodes proximally is at an imaginary plane connecting the lateral surfaces of the ascending and descending portions of the thoracic aorta. The left hilar nodes are located medial, anterior, posterior, and lateral to the left mainstem bronchus in order of decreasing frequency in number. The hilar nodes located anteriorly are found in relation to the left mainstem pulmonary artery. Proximally, these latter nodes are contiguous with the subaortic lymph nodes of the mediastinum, including the lymph node located at the site of the ligament arteriosum, the so-called Bartello’s node. The nodes on the medial surface of the main-stem bronchus, as their position advances upward, become subcarinal in location.
Table 6-2 Bronchopulmonary Nodes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Lobar Lymph Nodes
The two most common locations in which lobar lymph nodes are found in the right lung are between the upper-lobe bronchus and middle-lobe bronchus: the area that Borrie6 termed the right bronchial sump (the superior interlobar lymph node of Rouvière59) and the region just below the middle-lobe bronchus adjacent to the lower lobe bronchus (the inferior interlobar lymph node of Rouvière59). In the left lung, the most common location is at the angle of the left-upper-lobe bronchus and the lower-lobe bronchus. Borrie6 designated this area as the left lymphatic sump, and the nodes found here correspond to the left interlobar node of Rouvière.59
Right Lymphatic Sump
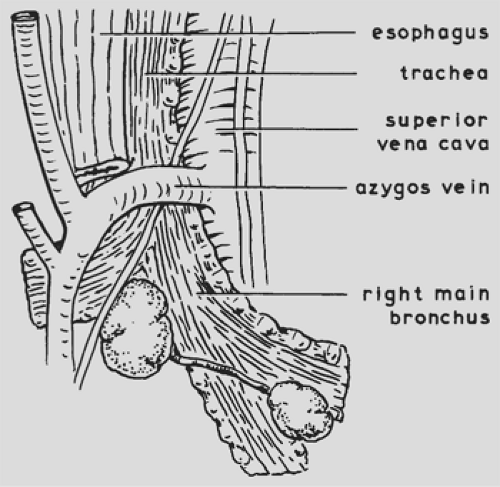
The lymph nodes in the lymphatic sump of the right lung lie in relation to the bronchus intermedius (Fig. 6-3). According to Nohl-Oser,47 a constant lymph node is found at the upper posterior end of the major fissure in the angle between the right-upper-lobe bronchus and the bronchus intermedius. A branch of the bronchial artery coursing over the posterior aspect of the right main bronchus leads to it (Fig. 6-4). Another lymph node is found on the interlobar portion of the pulmonary artery where this vessel gives off the posterior ascending segmental branch to the posterior segment of the upper lobe and the superior segmental artery to the superior segment of the lower lobe. Inferiorly, this lymph node is contiguous with a constant node lying above the superior segmental bronchus of the lower lobe. Other
lymph nodes of the sump are found at the base of the major fissure lying closely alongside the interlobar portion of the pulmonary artery or in the bifurcations of its branches. Frequently, lymph nodes are identified more anteriorly, lying among the upper lobe branches of the superior pulmonary vein.
lymph nodes of the sump are found at the base of the major fissure lying closely alongside the interlobar portion of the pulmonary artery or in the bifurcations of its branches. Frequently, lymph nodes are identified more anteriorly, lying among the upper lobe branches of the superior pulmonary vein.
Other Interlobar Lymph Nodes of the Right Lung
In addition to the sump nodes, the other interlobar lymph nodes can be grouped, according to Borrie,7 into those of the upper, middle, and lower lobes. The lymph nodes of the right upper lobe are located above the upper-lobe bronchus, medial to it, and just behind it. Those lying above the bronchus merge with the hilar nodes of the distal portion of the right mainstem bronchus. The lymph nodes of the middle lobe, in addition to the subjacent node below the middle-lobe bronchus (the inferior interlobar node of Rouvière59) are located lateral to the middle-lobe bronchus near its confluence with the lower-lobe bronchus as well as medial to it. The right-lower-lobe lymph nodes, in addition to the aforementioned superior and inferior sump nodes, are found medial to the superior segmental bronchus or between it and the basal bronchi. Lymph nodes are present also in relationship to the basal stem of the lower-lobe bronchus and lie on its medial aspect, lateral to it, and between the anterior and medial basal bronchi.
Left Lymphatic Sump
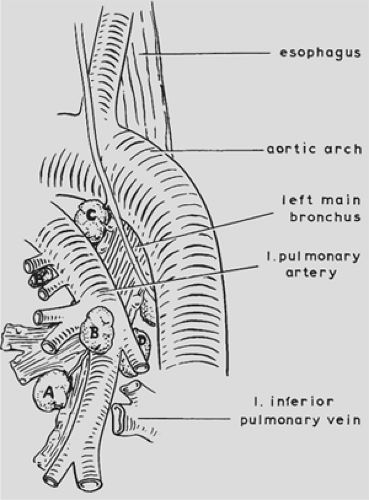
The collection of lymph nodes described by Nohl44,45 and Nohl-Oser47 as composing the left lymphatic sump lies between the upper and lower lobes in the main fissure (Fig. 6-5). A constant node is present in the bifurcation between the upper- and lower-lobe bronchi in close relation to the origin of the lingular (inferior division) branch of the upper lobe (Fig. 6-6). A small bronchial arterial branch passing across the membranous portion of the left main bronchus leads to it. Other lymph nodes are found lying on the interlobar portion of the left pulmonary artery in the fissure and in the angles formed by its branches. Another constant node is described, which is found above and posterior to the left interlobar bronchus. This node is contiguous with a node lying in the angle formed by the interlobar bronchus and the takeoff of the bronchus to the superior segment of the lower lobe.
Other Interlobar Lymph Nodes of the Left Lung
In addition to the left lymphatic sump nodes, Borrie7 noted that lymph nodes of the left upper lobe are present medial, posterior, and lateral to the upper-lobe bronchus. Lymph nodes are present also between the segmental divisions of this bronchus.
The lymph nodes of the left lower lobe are located more commonly in the vicinity of the superior segmental bronchus of the lobe. They are found medial, above, and inferior to it, between it and the basal bronchi. The other lobar nodes of the lower lobe are found medial or lateral to the basilar stem of the lower lobe bronchus.
Lymphatic Drainage of the Lobes of the Lung to the Bronchopulmonary Lymph Nodes
The lymphatic drainage of the lobes of the lungs is primarily to the bronchopulmonary nodes, although direct lymphatic drainage to the mediastinal lymph nodes was described by Rouvière,59 Borrie,6 Cordier,10 and Riquet54 and their colleagues, as well as by the last author in 1993. This direct drainage is discussed subsequently.
The right-upper-lobe lymphatic drainage, as deduced from the study of Borrie,7 is commonly to one of the superior interlobar lymph nodes (the sump nodes) on the lateral aspect of the bronchus intermedius, to the nodes above the right-upper-lobe bronchus and to those medial to it. Subsequent drainage is proximal to the azygos or subcarinal lymph nodes. Distal drainage has not been described as occurring to any lymph nodes below the lower level of the right lymphatic sump.
The middle lobe lymphatics drain to lymph nodes of the superior sump region, although drainage to the inferior sump node also occurs. Okada and associates50 also recorded drainage directly to the subcarinal nodes. Later studies by Watanabe65 and Asamura2 and their colleagues as well as by Naruke40 have confirmed this direct drainage to the subcarinal area and also to the midline pretracheal mediastinal nodal area. Drainage from the right lower lobe is to the inferior interlobar node and to the superior sump nodes, primarily those lying on the medial surface of the bronchus intermedius. Proximal drainage may also occur directly as well to the subcarinal nodes, as recorded by Okada and colleagues50 and subsequently by the authors noted previously in the discussion of the drainage of the middle lobe.
Drainage of the left upper lobe from all segments may occur to the left sump nodes. Nodes around the upper lobe bronchus and the left mainstem bronchus also receive drainage from this lobe. Direct drainage to subaortic mediastinal nodes may occur from the superior division of the left upper lobe, whereas direct drainage to the mediastinum from the inferior division (lingula), when it occurs, is commonly to the subcarinal mediastinal nodes, as recorded by Asamura and associates.1,2 Lymphatic drainage of the lower lobe is to the subjacent peribronchial nodes and to the interlobar sump nodes. From here, drainage is proximal to the hilar or mediastinal lymph node groups or both.
Lymphatic drainage from the middle and right lower lobes and the left lower lobe also occurs to the nodes in the respective pulmonary ligament. These lymph nodes are considered to be mediastinal lymph nodes. The incidence of nodes identified in Borrie’s work7 was 12% in the right pulmonary ligament and 47% in the left.
Mediastinal Lymph Nodes
The mediastinal lymph nodes that are important in the lymphatic drainage of the lungs can be divided into four distinct but interconnected groups: the anterior (prevascular) lymph nodes in the anterior mediastinal compartment, the tracheobronchial lymph nodes, the paratracheal lymph nodes, and the posterior lymph nodes in the posterior area of the visceral compartment of the mediastinum.
Anterior Mediastinal Lymph Nodes
The anterior mediastinal lymph nodes are in the prevascular compartment of the mediastinum and override the upper portions of the pericardium and great vessels as these extend upward. On the right side, the nodes lie parallel and anterior to the right phrenic nerve. They extend upward to and along the superior vena cava (these may be located between the vein and the ascending aortic arch) to the area beneath the right innominate vein. On the left, they are in close proximity to the origin of the pulmonary artery and the ligamentum arteriosum. They extend upward near the left phrenic nerve to lymph nodes
lying along the inferior border of the left innominate vein in the region where it is joined by the left superior intercostal vein.
lying along the inferior border of the left innominate vein in the region where it is joined by the left superior intercostal vein.
Tracheobronchial Lymph Nodes
The tracheobronchial lymph nodes lie in three groups around the bifurcation of the trachea. The right and left superior tracheobronchial nodes are located in the obtuse angles between the trachea and the corresponding mainstem bronchus. These nodes lie outside of the pretracheal fascia. The lymph nodes of the right superior tracheobronchial group are medial to (beneath) the arch of the azygos vein and above the right pulmonary artery. These nodes are contiguous with the right superior hilar nodes distally and the right paratracheal nodes proximally. On the left side, the superior tracheobronchial nodes lie deep within the concavity of the aortic arch. Some are closely related to the left recurrent laryngeal nerve; others are situated slightly more anteriorly and are contiguous with the node at the ligamentum arteriosum and the root of the left pulmonary artery. Their association with these nodes constitutes the link between the nodes in the visceral compartment and those in the anterior mediastinal lymph node group. Last, the para-aortic nodes lying anterior and lateral to the ascending aorta and the arch are also in the anterior compartment.
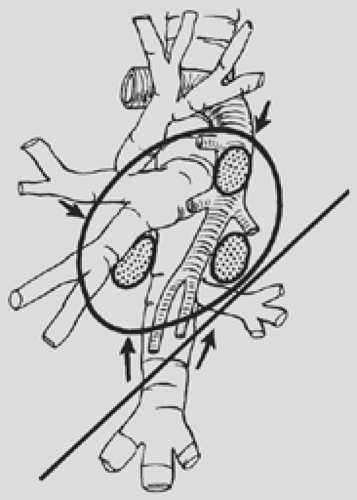
The inferior tracheobronchial nodes, more commonly referred to as the subcarinal nodes, lie in the angle of the bifurcation of the trachea (Fig. 6-7). Although these nodes, in contrast to the superior tracheobronchial groups, lie within the pretracheal fascial envelope, they lie outside the relatively dense bronchopericardial membrane. These nodes are contiguous with the hilar nodes on the medial aspect of both the right and left mainstem bronchi. Some of the subcarinal lymph nodes lie more posteriorly in relationship to the tracheal bifurcation and are on the anterior surface of the esophagus and are thus connected with the posterior group of lymph nodes. In addition, Brock and Whytehead8 described a low anterior tracheal group lying in front of the lower end of the trachea, which constitutes a bridge between the right superior tracheobronchial lymph nodes and the subcarinal, inferior tracheobronchial lymph nodes.
The paratracheal lymph nodes are situated on the right and left sides of the trachea above the respective superior tracheobronchial nodes and extend upward along the trachea. The right paratracheal lymph nodes lie anterolaterally to the trachea and to the right of the innominate artery. Inferiorly, these nodes are overlapped by the superior vena cava. More superiorly, these nodes lie behind and above the innominate artery to the right of the midline of the trachea and extend to the inlet of the chest. Inferiorly, the left paratracheal nodes lie above the tracheobronchial angle to the left of the midline of the trachea behind the aortic arch. More superiorly, they are situated above the arch but behind the great vessels and extend to the inlet of the chest. The left paratracheal lymph nodes are generally smaller in size and number compared with the right paratracheal lymph nodes.
Posterior Mediastinal Lymph Nodes
The posterior mediastinal lymph nodes may be separated into two groups: the paraesophageal nodes and those located in either pulmonary ligament. These posterior nodes are identified less commonly in the superior portion than in the inferior portion of the mediastinum. A paraesophageal node occasionally is found retrotracheally at the level of the arch of the azygos vein. The paraesophageal nodes as a group are more numerous in the inferior portion of the mediastinum and are found more frequently on the left than on the right side. The inferiorly located nodes have connections with the para-aortic nodes beneath the diaphragm. In the pulmonary ligament on either side, usually two or more small lymph nodes may be present. A relatively constant node, and usually the largest, lies in close proximity to the inferior border of the inferior pulmonary vein and is often termed the sentinel node of the pulmonary ligament.
Mediastinal Lymph Node Maps
Naruke and associates42 suggested the use of an anatomic map with the aforementioned conventional lymph node stations numbered so that the various lymph node stations involved by tumor could be uniformly recorded in patients with lung cancer (Fig. 6-8). This mapping scheme is used by most Japanese surgeons and has been used with minor modifications by the Sloan-Kettering Memorial group and others in North America. The American Joint Committee for Cancer Staging and End Results Reporting (AJC) published a similar map in its 1983 fascicle. The lymph node stations are defined in Table 6-3. The American Thoracic Society (ATS) in a report by Tisi and colleagues,61 however, noted what they believed to be deficiencies in the commonly accepted specific anatomic definition of each nodal station when determined by mediastinoscopy, mediastinotomy, and computed tomography (CT) examinations of the chest. Although some of the points were minor, a major area of conflict was the recommendation that the hilar stations, the right and left stations 10 of the Naruke and AJC maps, be deleted because of the ambiguity of the radiologic definition of these areas. It was suggested that these areas be redesignated as peribronchial on the left and tracheobronchial on the right and be assigned to the mediastinal compartments, both stations being outside of the pleural reflection. It should be noted that recently Asamura
and coworkers3 presented data supporting the concept that the station 10 nodes rightly belong in the hilar compartment rather than being included in the mediastinal compartment. The ATS suggested the anatomic stations as listed in Table 6-4 and located as represented in Figure 6-9. The ATS map has been adopted by many investigators in North America. The validity of one schema over the other is moot. In reviewing data presented in the literature, however, cognizance of the differences in the method of recording the data must be borne in mind for their proper interpretation.
and coworkers3 presented data supporting the concept that the station 10 nodes rightly belong in the hilar compartment rather than being included in the mediastinal compartment. The ATS suggested the anatomic stations as listed in Table 6-4 and located as represented in Figure 6-9. The ATS map has been adopted by many investigators in North America. The validity of one schema over the other is moot. In reviewing data presented in the literature, however, cognizance of the differences in the method of recording the data must be borne in mind for their proper interpretation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree