Lymphatic Distribution, Centrilobular Nodules
Eric J. Stern, MD
DIFFERENTIAL DIAGNOSIS
Common
Sarcoidosis, Pulmonary
Silicosis/Coal Worker’s Pneumoconiosis
Lymphangitic Carcinomatosis
Less Common
Lymphoma, Non-Hodgkin or Hodgkin
Bronchiolitis, Follicular
Amyloidosis
Berylliosis
Rare but Important
Lymphocytic Interstitial Pneumonia
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Definition of lymphatic pattern
Predominant abnormality is nodules (< 1 cm diameter) in pulmonary lymphatics
Often called “perilymphatic” (pathology, however, usually in lymphatics)
Lymphatic compartments
Axial: Follows bronchi and arteries to level of terminal bronchioles in secondary pulmonary lobule
Peripheral: Follows veins, septa, and pleura
Alveoli and respiratory bronchioles devoid of lymphatics
Same disease process may sometimes preferentially involve axial lymphatics, sometimes peripheral lymphatics
Pathophysiology of disease
Inhalational: Especially from rounded dust particles
Hematogenous less common, implies migration into adjacent lymphatics (lymphohematogenous dissemination)
Lymphatic vs. hematogenous pattern
Lymphatic nodules
Clustered like grapes, unlike dispersion in random distribution pattern
May be focal and localized; random is usually diffuse
Lymphatic pattern
Nodules arranged in rays along bronchovascular pathways
Usually associated with subpleural and fissural nodules that comprise > 10% of total number of nodules
Often more severe in upper lung zones, random pattern often more severe in lower lung zones
Often associated with hilar and mediastinal adenopathy
Lymphatic vs. bronchovascular pattern
Bronchovascular pattern nodules less common along fissure and subpleural lung (< 10% of total number of nodules)
Associated with small airways disease: Mosaic attenuation, air-trapping, tree-in-bud opacities
May be focal (from aspiration) or diffuse (from inhalation disorders)
Some diseases start as bronchovascular pattern (from acute-semiacute reaction from inhaled pathogen) and evolve into lymphatic pattern (as pathogen migrates to draining lymphatics)
Lymphatic pattern often associated with hilar and mediastinal adenopathy
Helpful Clues for Common Diagnoses
Sarcoidosis, Pulmonary
Focal aggregation of nodules along bronchovascular bundles
Nodules may be clustered into large masses (called alveolar sarcoid)
Galaxy sign: Coalescent mass surrounded by its constituent smaller nodules
Nodules more profuse in upper lung zones
Symmetric hilar and mediastinal adenopathy common
Nodes may contain chalky-smudgy or eggshell pattern calcification
Silicosis/Coal Worker’s Pneumoconiosis
Work history of occupational exposure to silica particles or coal
Nodules more profuse in upper lung zones
Nodules tend to aggregate in dorsal aspect of lung; right lung usually more severely involved than left
Severity and time results in progressive massive fibrosis (PMF)
Hilar and mediastinal lymphadenopathy may show “eggshell” calcification (5%)
Inhalational talcosis and siderosis give identical findings (reflects lung’s ability to chronically handle small rounded dusts)
Lymphangitic Carcinomatosis
Seen primarily with adenocarcinomas
Frequency of involvement: Axial lymphatics (75%), axial + peripheral (20%), peripheral (5%)
Characteristically spares whole lobe or even whole lung
Lung architecture preserved, unlike sarcoidosis and silicosis, which show architectural distortion
Pleural effusion(s) common (unusual in sarcoidosis or silicosis)
May have adenopathy
Helpful Clues for Less Common Diagnoses
Lymphoma, Non-Hodgkin or Hodgkin
Pulmonary involvement in Hodgkin (40%) and non-Hodgkin (25%) disease
Primarily involves axial lymphatics
Pulmonary nodules, usually > 1 cm (often with air-bronchograms)
Associated with bulky lymphadenopathy, effusion(s) also common
Bronchiolitis, Follicular
Synonym: Lymphoid hyperplasia of bronchus-associated lymphoid tissue (BALT)
Pathology: Similar to lymphocytic interstitial pneumonia (LIP)
Follicular bronchiolitis: Centered on airway lymphatics
Interlobular septal thickening, bronchiolectasis, thin-walled cysts
Associated with collagen vascular diseases (rheumatoid arthritis, Sjögren syndrome), AIDS, infections, hypersensitivity reaction
Amyloidosis
Primary (associated with myeloma) and secondary (associated with chronic inflammatory disease)
Wide spectrum findings: Tracheobronchial thickening and nodularity, centrilobular nodules, septal thickening
Diffuse septal form more commonly has nodules in subpleural lung
Nodules may calcify
Berylliosis
Gives identical findings, occupational history important
Beryllium lightweight metal with high melting point, used in wide variety of industries
Latent period after exposure of 1 month to 40 years
Incites hypersensitivity reaction with granulomas
Helpful Clues for Rare Diagnoses
Lymphocytic Interstitial Pneumonia
Also associated with viral infection: HIV and Epstein-Barr virus, dysproteinemias, or Sjögren syndrome
Thin-walled cysts distinctive (80%)
Usually associated with nonspecific ground-glass opacities (100%)
Diffuse distribution
Image Gallery
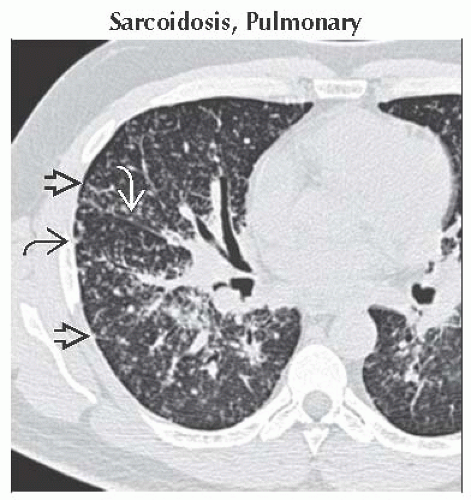 Axial HRCT shows typical perilymphatic distribution of subpleural
 , interlobular septal , interlobular septal  , and major fissure nodules , and major fissure nodules  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|