Figure 20.1
Dissection of paratracheal lymph nodes from right thoracotomy. All fatty areolar tissue is dissected from the superior vena cava (SVC), aorta, and trachea. Gentle traction and dissection with a blunt tipped aspiration cannula help mobilize the tissue packet
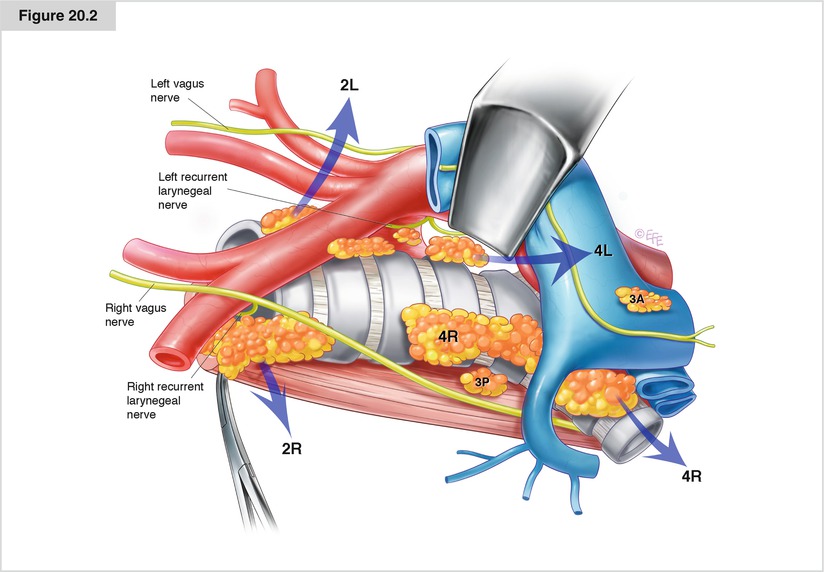
Figure 20.2
The packet is removed en bloc. Both innominate veins and the SVC, aorta, trachea, right subclavian artery, and truncus anterior of the right pulmonary artery form the borders
Dissection of Subcarinal and Inferior Mediastinal Nodes
Hyperinflation of the contralateral lung pushes the carina toward the surgeon. The bronchus intermedius is retracted in the anterior direction to widen this area. An incision with cautery is made parallel to the esophagus all the way from the azygos vein to the inferior pulmonary vein; caution should be used not to harm the vagus nerve, although branches of the vagus nerve coursing to the lung are divided. The esophagus is retracted posteriorly with a sponge. Subcarinal nodes are dissected by dividing the bronchopericardial ligaments and capsule surrounding the level 7 nodes. First, the nodes are dissected and a plane is created from the intermediate bronchus with cautery. By developing a space for the dissection of level 7 nodes that is inferior and anterior to the intermediate and main bronchi, the pericardium of the left atrium becomes visible. The nodes are dissected starting at the lower rim. Dissection near the pericardium releases half the subcarinal nodes, although these nodes are still attached to the tracheal carina and left main bronchus. Generally, at least one bronchial artery arising from the aorta feeds the nodes. Careful management, typically ligation, or a clip is needed to prevent postoperative bleeding. Dissection of the triangle formed by the left and right main bronchi and the right inferior pulmonary vein can be seen in Fig. 20.3.
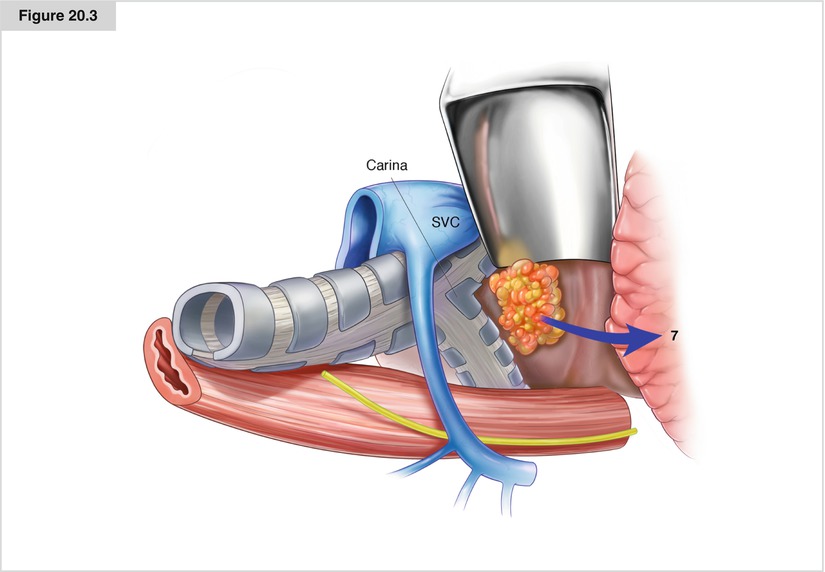
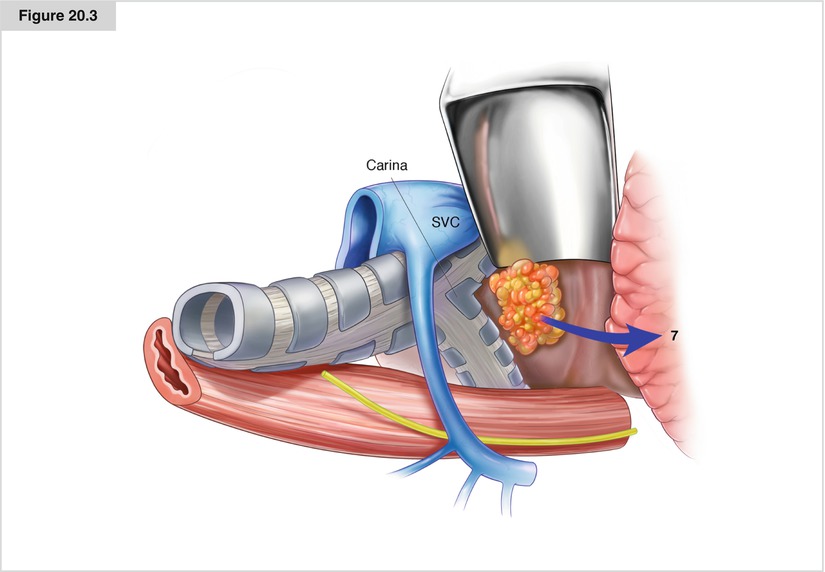
Figure 20.3
Dissection around the main bronchus and subcarinal space from the right side. The inferior pulmonary vein and left and right bronchi form the borders of the dissection
Level 8 nodes are dissected over the esophagus behind the inferior pulmonary vein. Level 9 nodes are included in the pulmonary ligament.
Left-Sided Lymph Node Dissection
Dissection of Stations 4L to 6
An inverse T-shaped incision similar to that used on the right side is made over the left hilum, and a vertical incision between the vagus and phrenic nerves above the aorta is used to remove level 5–6 nodes. In patients with cancer in the left upper lobe, it is extremely important to dissect the para-aortic (level 6) and subaortic lymph nodes (level 5) (Fig. 20.4). The left-sided tracheobronchial lymph nodes (level 4L) are located medial to the subaortic lymph nodes, and these nodes can be dissected easily with or without Botallo’s ligament division by giving extreme care to the left recurrent laryngeal nerve branch. A bronchial artery almost always arises from the aorta in that window (Fig. 20.5).
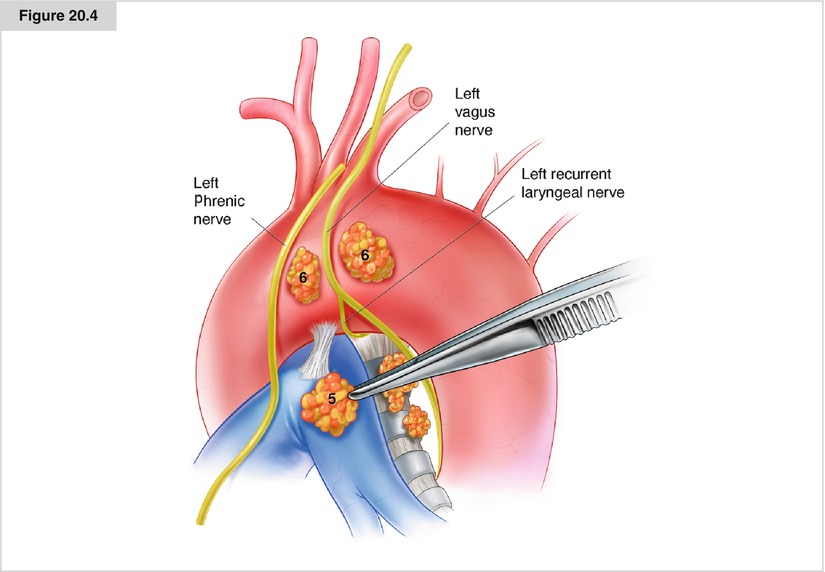
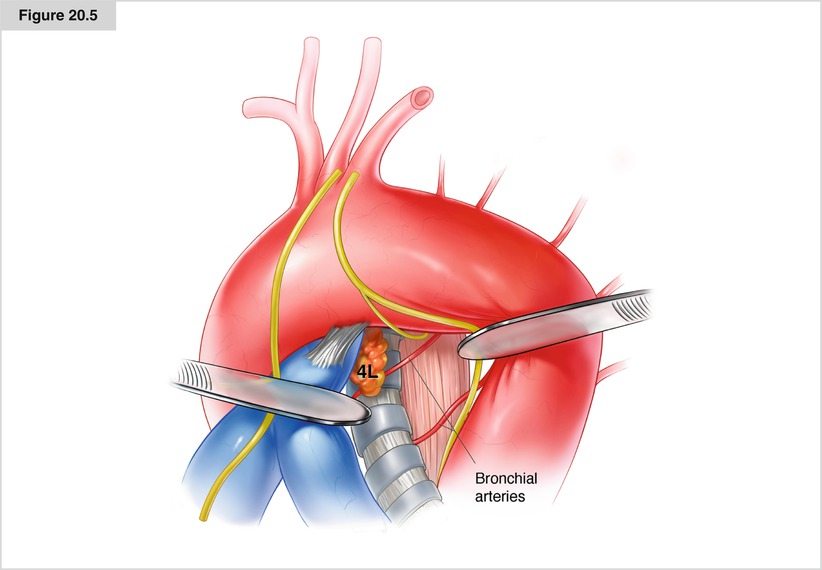
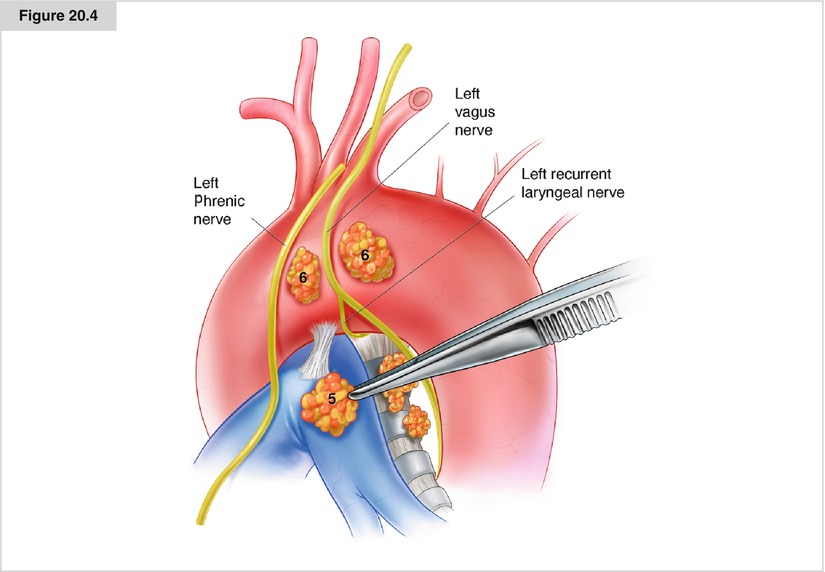
Figure 20.4
Dissection of stations 5 and 6. Careful dissection in this station enables a place for dissection of station 4L
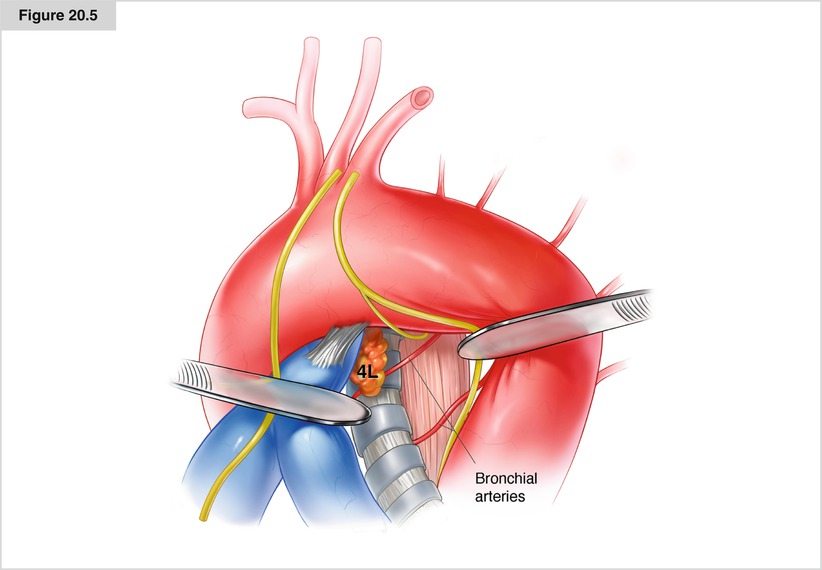
Figure 20.5




Dissection of station 4L. The left tracheobronchial angle and inferior part of the trachea and esophagus are dissected. A bronchial artery may be seen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


