Figure 48.1
Lungs are harvested via a standard midline sternotomy. After the pericardium and both pleurae are opened, the lungs are palpated and examined visually. The superior and inferior venae cavae are encircled, and a suture is placed around the superior vena cava to prepare for later ligation. The aorta and pulmonary artery are separated; then, a pursestring suture is placed in the main pulmonary artery approximately 1–2 cm central to the bifurcation to ensure adequate perfusion of both lungs and to leave a sufficient length of main artery in case the heart is to be harvested simultaneously. After full heparinization of the donor with 300 IU/kg of heparin, the pulmonary artery is cannulated. Most centres administer 500 μg of prostaglandin E1 intravenously or directly into the pulmonary artery prior to any vascular occlusion. Thereafter, the superior vena cava is ligated. The inferior vena cava is clamped to allow a sufficient cuff for both the heart and liver. Finally, the ascending aorta is cross-clamped and perfusion with a preservative solution is started. Most centers use 4–6 L of extracellular dextran solution for preservation. Immediately after cross-clamping, the auricle of the left atrium is opened to allow drainage of the preservative solution. If the heart is to be harvested simultaneously, the solution is administered via the ascending aorta and drained via an incision in the inferior vena cava. During the entire perfusion period, the lung is ventilated to allow optimal distribution of the preservative solution. As soon as perfusion is complete, ventilation is stopped and the perfusion cannulas are removed. If the heart is to be harvested, that step is done immediately after perfusion, usually by first dissecting the inferior vena cava. During separation of the left atrium, special attention must be paid to ensure a sufficient cuff for both the lungs and the heart. Too much upward traction on the heart should be avoided to ensure normal vein anatomy, especially on the right side, and to avoid cutting too peripherally. Finally, the superior vena cava and aorta are divided. The pulmonary artery is divided just central to the bifurcation to maximize the length of the main truncus for heart transplantation and the full length of the left and right main arteries for lung transplantation. Retrograde flush perfusion of the lungs with preservative solution may be performed either at this stage, with the lungs in situ, or on the back table after removal. After the heart is removed, the pericardium is incised caudally down to both pulmonary ligaments. Starting on either side, the pulmonary ligament is divided, then the dissection is carried upward along the posterior mediastinum anterior to the esophagus until it reaches the level of the upper trachea. Thereafter, dissection is performed on the other side. During this maneuver, the azygos vein has to be divided on the right side and the descending aorta on the left. Next, the anterior trachea is prepared cervically, and the remaining tissue lateral to the trachea, including the carotid artery, subclavian artery, and corresponding veins, is divided. This leaves the entire double-lung block just connected to the trachea. The lungs are moderately inflated, and the trachea is stapled as cranially as possible. Finally, the lungs are removed from the donor chest cavity. After the lungs are inspected carefully, separation may be performed at the back table. After the posterior pericardium is dissected, the left atrium and the pulmonary arteries are separated in the midline. Thereafter, the left main bronchus is prepared and stapled just below the carina. Care must be taken not to denude the bronchus to avoid ischemic complications of the anastomosis after transplantation. The lungs are stored inflated on Perfadex (Vitrolife, Englewood, CO) and cooled on ice at 4 °C for transport. Harvesting is standardized as described earlier in brain-dead donors. In non–heart-beating donors, additional logistic preparations with topical cooling of the lungs in the donor may be necessary (Aigner 2003b, Orens 2003)
Single-Lung Transplantation Technique
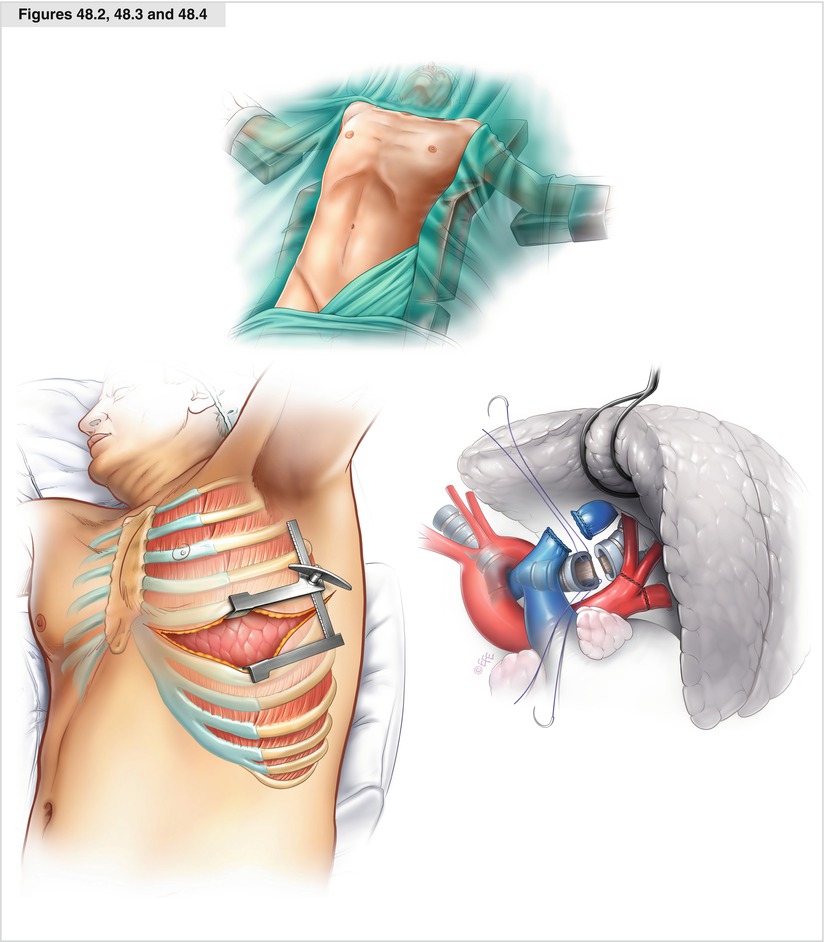
Figures 48.2, 48.3 and 48.4




The patient may be placed either in a supine position with the arms abducted and chest elevated as for double-lung transplantation or at a 45° angle with the ipsilateral arm positioned above the head to improve exposure to the posterior hilum. At least one groin is scrubbed to allow placement of cannulas for extracorporeal support. Anterolateral thoracotomy is performed, preferably in the fourth intercostal space on the right side and the fifth intercostal space on the left. Standard pneumonectomy with stapling of the pulmonary artery and veins is performed. The bronchus is prepared centrally and cut with a scalpel. Two polydioxanone (PDS) 4-0 stay sutures are placed at the angle between the membranous portion and the cartilaginous part. After the lung is removed from the chest cavity, the pericardium is opened above the superior pulmonary vein and the left atrium is dissected circumferentially. Thereafter, the pulmonary artery is dissected intrapericardially as centrally as possible. After the intrapericardial dissection is complete, the posterior mediastinum may be closed with a PDS 4-0 suture to prevent bleeding, which is difficult to control after the lung has been implanted. Before implantation begins, it is crucial to achieve accurate haemostasis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


