Lung Transplantation
Michael J. Weyant
G. Alec Patterson
Lung transplantation is an accepted therapeutic modality for patients with nonmalignant end-stage lung disease. Currently the most common indications for lung transplantation include:
Pulmonary fibrosis
Cystic fibrosis
Chronic obstructive pulmonary disease (COPD)
Primary pulmonary hypertension
Specific guidelines for acceptability for transplant according to disease type are as follows:
Chronic Obstructive Pulmonary Disease
BODE* index >5
FEV1 <20% of predicted
Diffusion capacity <20% of predicted
Pulmonary hypertension or cor pulmonale despite oxygen therapy
Hypercapnia, PaCO2 >50 mm Hg
Interstitial Lung Disease
Usual interstitial pneumonia (UIP) or nonspecific interstitial pneumonia (NSIP)
FVC <60% of predicted
Diffusion capacity <39% of predicted (UIP) or <35% of predicted (NSIP)
Drop in FVC by ≥10% or diffusion capacity by ≥15% over a 6-month period
Drop in SaO2 on pulse oximetry by <88% on 6-minute walk test
Secondary pulmonary hypertension
Cystic Fibrosis
FEV1 <30% of predicted
PaO2 <55 mm Hg
PaCO2 >50 mm Hg
Exacerbations requiring intensive care unit stays
Increasing frequency of pulmonary exacerbations requiring antibiotic therapy
Recurrent and/or refractory pneumothorax
Recurrent hemoptysis not controlled by bronchial artery embolization
Pulmonary hypertension
Progressive weight loss, body mass index (BMI) <18 kg/m2
Primary Pulmonary Hypertension
Low or declining 6-minute walk test at <380 ft
Maximum oxygen intake <10.4 mL/min/kg
World Health Organization functional stage III or IV on maximal medical therapy
Cardiac index <2 L/min/m2
Right atrial pressure >15 mm Hg
Failure of intravenous epoprostenol therapy or equivalent
Absolute
Malignancy in the last 2 years except for cutaneous squamous and basal cell tumors, 5-year disease-free interval is prudent
Dysfunction of another major organ system (heart, liver, or kidney) that is not amenable to treatment
Noncurable extrapulmonary infection (active viral hepatitis B, hepatitis C, human immunodeficiency virus)
Significant chest wall/spinal deformity
Nonadherence and/or inability to follow through with medical therapy or office follow-up
Untreatable psychiatric or psychologic condition(s) associated with the inability to cooperate or comply with medical therapy
Lack of dependable social support system
Substance addiction (alcohol, tobacco, or narcotics) within the last 6 months
Relative
Age older than 65 years
Critical or unstable clinical condition
Severely limited functional status with poor rehabilitation potential
Colonization with highly resistant or highly virulent bacteria, fungi, or mycobacteria
Severe obesity defined as a BMI exceeding 30 kg/m2
Severe or symptomatic osteoporosis
Mechanical ventilation
Other medical conditions that have not resulted in end-stage organ damage, such as diabetes mellitus, systemic hypertension, peptic ulcer disease, or gastroesophageal reflux should be optimally treated before transplantation
Donor Lung Identification and Management
The standard selection criteria used for many years to identify suitable lungs from brain dead donors:
Age <55 years
No history of pulmonary disease
Normal chest radiographs
Adequate gas exchange—PaO2 >300 mm Hg on FiO2 of 100%, PEEP 5 cm H2O
Normal bronchoscopic examination
Negative serologic screening for hepatitis C and human immunodeficiency virus
Recipient matching for ABO group
Size matching
Using these criteria however leads to a rate of usage of approximately 20% of offered organs. This has generated significant interest in identifying additional donors outside of the standard brain dead donor classification.
Donor Management
The significant points of donor management aimed at increasing the chances of successful procurement are as follows:
Ventilation at 8 to 10 cc/kg
Closed tracheal suction every 2 hours
Reposition patient every 2 hours
Restrict crystalloids and diurese to CVP 4 to 8 mm Hg
Arterial blood gas on FiO2 1.0 and peep 5 cm H2O
Recruitment maneuver if PaO2/FiO2 ratio <300 mm Hg
Increase peep to 15 cm H2O
Tidal volume 8 to 10 cc/kg
Plateau pressure ≤30 cm H2O
Bronchoscopy and BAL
Donation after Cardiac Death
Donors that are deemed to have no recoverable function but do not meet standard brain death criteria are eligible candidates for DCD organ donation. There are significant legislative and ethical hurdles to the use of DCD donors in many communities, which is demonstrated by a very low usage rate of these organs. Several centers have published results that are comparable to the standard technique. This population of patients represents a large potential organ pool and continued interest in this area is critical.
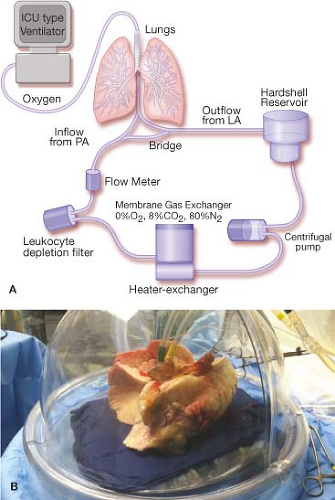
Ex Vivo Lung Perfusion
Ex vivo lung perfusion (EVLP) has become an accepted technique in several countries to evaluate donor lungs outside the donor for an extended period of time (Fig. 34.1A,B). Several clinical trials have demonstrated equivalence with standard transplant. This technique represents the potential to evaluate donors from DCD and marginal candidates to improve their function and expand the donor pool.
The detailed workup of a recipient is beyond the scope of this text as most lung transplant recipients are evaluated weeks to months prior to transplant. The immediate preoperative planning regarding lung transplantation is, however, extremely important and covers multiple areas including recipient evaluation, donor evaluation, operating room preparation, and staffing concerns. The change in the lung allocation scoring (LAS) system in 2005 was beneficial for patients with the highest degree of pulmonary failure who were moved to the top of the list and therefore more likely to receive donor organs. This change significantly altered how we conduct the lung transplant process. The patients presenting for transplant are more critically ill than in the past and are more likely to need to be transplanted in the setting of a lung support device such as ECMO. These patients are
more likely to have significant secondary pulmonary hypertension and extreme hypoxia or CO2 retention and in need of intraoperative cardiopulmonary support. The pertinent considerations in the immediate preoperative period are discussed here.
more likely to have significant secondary pulmonary hypertension and extreme hypoxia or CO2 retention and in need of intraoperative cardiopulmonary support. The pertinent considerations in the immediate preoperative period are discussed here.
Patient Evaluation
Given the severity of the disease which patients present with at transplant it is important to understand the pulmonary status of the patient at the time of presentation for the operation compared to the initial evaluation period. This interval can range from days to months and having an understanding of the pace at which the patient has declined is helpful to have the appropriate support available in the operating room. A good example would be a pulmonary fibrosis patient who required 6 L of oxygen and had normal pulmonary artery pressures at the time of initial evaluation. At the time of presentation the status of the patient may be altered to the extent that the oxygen requirement is significantly increased which has implications on the development of secondary pulmonary hypertension in this short interval.
Level of Pulmonary Support
Is the patient being supported by ECMO or mechanical ventilation? The patient on ECMO will need support during the operation until at least one lung is implanted and functioning so that the device can be weaned. The decision has to be made as to whether ECMO will be continued throughout the procedure or be converted to centrally cannulated cardiopulmonary bypass. The patient who has recently been placed on mechanical ventilation will also likely need mechanical cardiopulmonary support at the outset of the procedure. Discussing all of the techniques of mechanical pulmonary
support is also beyond the scope of this text, however, several choices exist along the spectrum of ECMO to full cardiopulmonary bypass.
support is also beyond the scope of this text, however, several choices exist along the spectrum of ECMO to full cardiopulmonary bypass.
Single Lung or Double Lung
It may seem obvious to note single versus double lung, however, communicating this information to all donor coordinators, anesthesia staff, and operating room personnel will decrease the likelihood of catastrophic error.
Redo Transplant or First Time
The time required for a redo transplant can be significantly greater than a first-time operation. Planning the appropriate time of entry into the operating room will help decrease both the warm and cold ischemic times during the operation.
Level of Secondary Pulmonary Hypertension and Hypoxia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree