and Alessandra Cancellieri2
(1)
Department of Radiology, Bellaria Hospital, Bologna, Italy
(2)
Department of Pathology, Maggiore Hospital, Bologna, Italy
Radiology | Maurizio Zompatori Domenico Attinà |
CB | Constrictive Bronchiolitis | Page 240 |
CPTE | Chronic Pulmonary Thromboembolism | Page 242 |
DIPNECH | Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia | Page 244 |
Emphysema, panlobular | Emphysema, panlobular | Page 246 |
SJS | Swyer-James Syndrome | Page 248 |
Constrictive Bronchiolitis (CB)
Definition
Constrictive bronchiolitis (CB) refers to an irreversible destructive process characterized by inflammation and concentric fibrosis in the bronchiolar submucosal layer, associated with luminal occlusion and resulting in extrinsic compression and obliteration of the airway. CB is limited to the bronchioles and does not extend into the alveoli. The causes of CB include toxic fumes, oral toxins, respiratory infections (Mycoplasma), drugs, connective tissue diseases (particularly rheumatoid arthritis), and organ transplantation. CB is the most common form of chronic rejection in patients with lung transplants, occurring in up to 50 % of patients, especially after graft-versus-host reaction. CB is also seen as a manifestation of graft-versus-host disease in 10 % of people who have received allogeneic bone marrow transplants. Imaging findings in patients with this form of bronchiolitis are identical to those found with CB after lung transplantation.
Obliterative bronchiolitis, bronchiolitis obliterans
Kang EY (2009) Bronchiolitis: classification, computed tomographic and histopathologic features, and radiologic approach. J Comput Assist Tomogr 33:32
Leung AN (1998) Bronchiolitis obliterans after lung transplantation: detection using expiratory HRCT. Chest 113:365
High-Resolution CT: HRCT
Key Signs
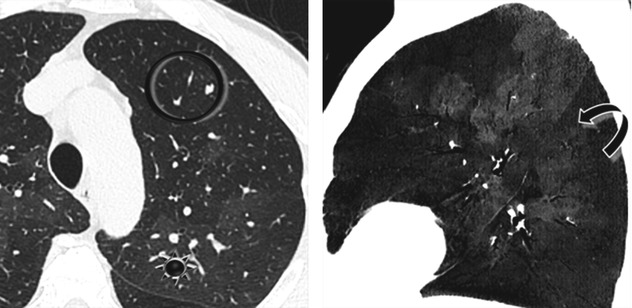
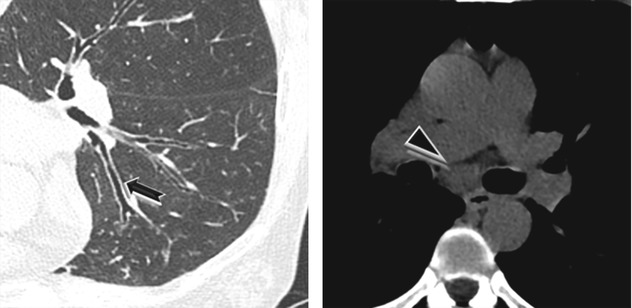
Sharply defined, areas of decreased lung attenuation (dark lung areas ) associated with vessels of decreased caliber (
) associated with vessels of decreased caliber ( ) (mosaic oligemia).
) (mosaic oligemia).
Air trapping is seen as dark parenchymal areas which remain dark or appear darker on end-expiration CT scans ( ) (please compare the HRCT images below).
) (please compare the HRCT images below).
Lung volume is normal or increased.
Distribution
Generally bilateral, asymmetrical. Patchy lobular, segmental, or larger confluent areas accentuated on expiratory scans. In some secondary forms of localized CB, such as postinfectious CB in Swyer-James syndrome (MacLeod), the lesions may predominate in one lung or lobe. In contrast, severe and extensive disease (rare) may have an almost uniform distribution similar to emphysema.
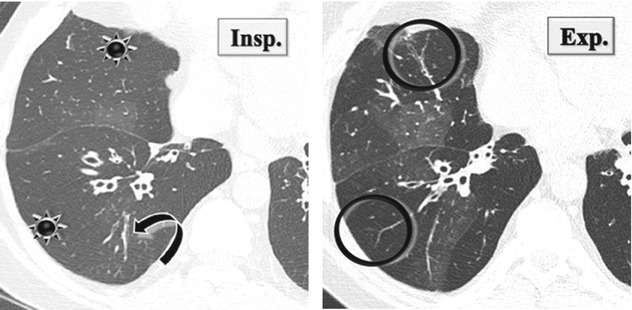
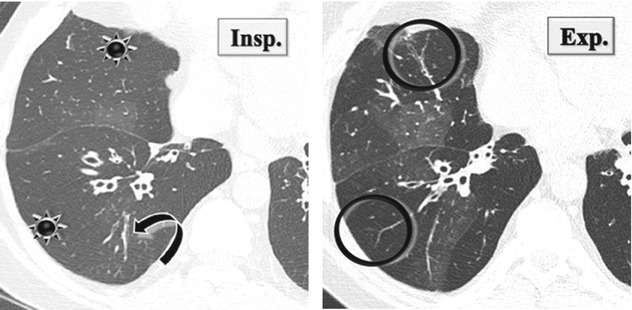
Paired inspiratory and expiratory thin-section CT can help distinguish CB from vascular obstructive lung disease. In CB, at the expiration state, dark areas remain as dark as in inspiration state, or get even darker, often with minimal decrease in volume.
Increased density of the normally ventilated areas where the vessels are enlarged due to hyperperfusion, at times to the point of simulating disease (pseudo-ground-glass opacity).
CB should not be confused with both bronchiolitis obliterans organizing pneumonia (BOOP), in which inflammation involves also alveoli and causes consolidations, and proliferative bronchiolitis with intraluminal polyps, which is a steroid-reversible lesion limited to the bronchiolar lumen which results obliterated.
Epler GR (2007) Constrictive bronchiolitis obliterans: the fibrotic airway disorder. Expert Rev Respir Med 1:139
Pipavath SJ (2005) Radiologic and pathologic features of bronchiolitis. AJR Am J Roentgenol 185:354
Ancillary Signs
Thickening of the bronchiolar walls (➨) and dilatation of the small bronchioles
Mucus plugs
Non-parenchymal Signs
Lymph nodes enlargement ( ►)
Hansell DM (1997) Obliterative bronchiolitis: individual CT signs of small airways disease and functional correlation. Radiology 203:721
Lynch JP 3rd, Weigt SS, DerHovanessian A et al (2012) Obliterative (constrictive) bronchiolitis. Semin Respir Crit Care Med 33:509
Course and Complications
Prognosis is variable, ranging from slowly progressive to rapidly deteriorating disease.
Most patients deteriorate inexorably, ultimately dying of respiratory failure within months to years. In some patients the disease stabilizes after an initial decline.
Secondary bacterial infections may accelerate the course of disease.
Pulmonary function tests traditionally show airway irreversible obstruction with no response to bronchodilator inhalation. The extent of air trapping on expiratory CT provides the best correlation with indexes of physiologic impairment.
Bankier AA (2001) Bronchiolitis obliterans syndrome in heart-lung transplant recipients: diagnosis with expiratory CT. Radiology 218:533
Chronic Pulmonary Thromboembolism (CPTE)
Definition
Chronic pulmonary thromboembolism (CTPE) is a consequence of incomplete resolution of acute pulmonary thromboembolism. The failure of complete clot lysis occurs in 4–5 % of patients with pulmonary embolism. Unresolved thrombi form endothelialized fibrotic obstructions of the pulmonary vascular bed. Vascular stenosis and increased vascular resistance may lead to severe pulmonary hypertension (CTEPH) and cor pulmonale. In the majority of patients, months or even years (the so-called honeymoon period) may pass before clinically significant CTEPH manifests. The most common presenting symptom is indolent but progressive shortness of breath with normal pulmonary functional tests. Patients with CTEPH become symptomatic only when at least 60 % of the pulmonary arterial bed is obstructed.
CPTE, CPE
Wittram C (2004) CT angiography of pulmonary embolism: diagnostic criteria and causes of misdiagnosis. Radiographics 24:1219
Guérin L (2014) Prevalence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Thromb Haemost 2;112:598
High-Resolution CT: HRCT
Key Signs
Patchy regions of decreased attenuation (dark lung ) and increased attenuation (white lung
) and increased attenuation (white lung  ) because of irregular perfusion (mosaic oligemia).
) because of irregular perfusion (mosaic oligemia).
Distribution
Patchy, generally lower lobes are more affected.