Lung Disease in Bone Marrow Transplant Patients
Fabio R. Tavora, M.D., Ph.D.
Allen P. Burke, M.D.
Graft-Versus-Host Disease
Incidence
Graft-versus-host disease (GVHD) occurs in approximately one-third of patients with allogeneic stem cell transplants and primarily affects the skin, liver, and gastrointestinal tract. Clinically significant pulmonary complications occur in 40% to 60% of all patients, of which nearly one-half have noninfectious causes and are related to GVHD.1 While less common than in other organ systems, patients with pulmonary GHVD tend to have more severe long-term complications and shorter disease-specific survival. Only a small proportion of patients with clinical pulmonary GHVD undergo biopsy, and histologic descriptions in the literature are few.2 Although GVHD has been reported after autologous stem cell transplant,3 the lung as a target organ has yet to be reported.
Stages of Pulmonary GVHD
Traditionally, pulmonary GVHD is synonymous with bronchiolitis obliterans syndrome (BOS), considered a chronic form of GVHD, and histologic similar to chronic lung allograft rejection. Although “acute” GVHD is not applied to a specific pulmonary syndrome, there is evidence that an acute form of pulmonary GVHD may exist. GVHD is a risk factor for the development of idiopathic pneumonia syndrome (IPS), which is a form of acute lung injury. Acute and organizing lung injury may be seen in biopsies of patients with extrapulmonary acute GVHD.2 Additionally, CT abnormalities have been described in patients with acute GVHD, which correspond to interstitial lung disease with relatively acute patterns of injury.
Acute GVHD: Clinical and Imaging Findings
The diagnostic criteria of acute GVHD-induced lung injury are as follows: (1) patients have manifestations of GVHD in other organs (skin, liver, or gut); (2) patients have abnormal chest high-resolution computed tomography (HRCT) scans; (3) lung injury induced by infection and heart diseases are excluded; and (4) chest HRCT scans are improved after treatment for acute GVHD.4 Because the clinical concept of acute pulmonary GVHD is not generally accepted, pulmonary function test (PFT) results have not been extensively reported.6
The median onset of acute GVHD with pulmonary involvement was 31 days, with a range of 17 to 122 days.4 Several studies, in fact, reported the incidence acute noninfectious lung injury in the first 120 days after stem cell transplantation to be 3% to 15%.7
Pathologic Findings
The diagnosis of lung involvement with GVHD is generally based on clinical findings of noninfectious lung infiltrates in a patient with documented GVHD of other organs, often with biopsy of the skin, colon, and liver. In the lung, there are no accepted grading systems for GVHD. Because biopsies are seldom performed, it is endorsed that the diagnosis of chronic GVHD/BOS can be done using PFT alone. In fact, the lung score proposed by the 2014 Diagnosis and Staging Working Group report emphasizes clinical symptoms and FEV1 in lung function tests to increase sensitivity, but does not require biopsy diagnosis.9
Histologic findings of pulmonary GVHD include acute lung injury, chronic interstitial inflammation, organizing pneumonia, and obliterative bronchiolitis (OB) (Figs. 55.1, 55.2, 55.3, 55.4, 55.5). Denuded bronchiolar epithelium, regenerating atypical respiratory epithelial cells, and reactive pneumocytes are common.1,2 Prominent apoptotic debris and a chronic venulitis have also been described.5
The distinction between obliterative bronchiolitis and organizing pneumonia should be made, as the former is characteristic of BOS and the latter is a nonspecific pattern of subacute lung injury that does not inevitably scar the airway.2 A follow-up pathologic study showed that those patients who progressed to BOS showed chronic inflammatory changes, not organizing pneumonia, on prior lung biopsies.5
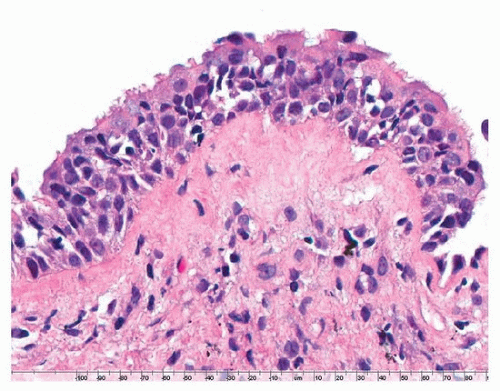 FIGURE 55.1 ▲ GVHD. The respiratory epithelium shows inflammatory infiltrates by mature lymphocytes and apoptotic bodies.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|