Lower-extremity Amputation
Lloyd A. Jacobs
Gerald B. Zelenock
Amputation is among the most ancient of surgical procedures. The basic operations have long been defined, and advances in operative technique for amputation surgery have been few of late. Nevertheless, important considerations in the detailed understanding of the disease processes underlying the need for amputation, the appropriate pre-operative assessment of these often severely compromised patients (including selection of the level of amputation), and integrated rehabilitative efforts, are critical for optimal outcomes. Many of the current treatment paradigms were developed by military surgeons and the Veterans Administration in the era since World War II and have been instrumental in defining optimal rehabilitation protocols of considerable benefit to amputees. However, as the population ages, these protocols, which were optimal for young combatants, must be significantly modified. The interaction of a host of physiologic processes on the decision for or against an amputation and the selection of the proper level of amputation will require careful integration of a variety of technical, physiologic, and sociologic factors.
Amputation is a generally straightforward surgical procedure but is not to be taken lightly. Patients requiring amputation for vascular disorders are usually elderly, frail, and have multiple comorbidities and co-existing medical illnesses. The procedure occurs in the setting of severely compromised tissues, and all the principles of appropriate handling of soft tissue, bone, and compromised wounds come into play to ensure an optimal outcome. The goal of amputation is to return the patient to an optimal level of function while relieving pain and removing all nonviable tissue. Ideally this is accomplished with a single definitive procedure rather than multiple returns to the operating room. When multiple procedures are required by a patient’s clinical status it is unfortunate; when multiple procedures result from a failure of preoperative evaluation or surgical technique it is doubly so.
The epidemiology of amputation is revealing; more than 140,000 amputations are performed each year in this country, with approximately half being major amputations of the leg either above or below knee. Digital, ray, transmetatarsal, and other less commonly employed procedures comprise the remainder. Diabetes, arterial insufficiency, chronic infection, and trauma account for the majority of amputations. Malignancy, congenital deformity, and other miscellaneous conditions represent the balance. In contemporary vascular surgical practice, amputation is indicated for gangrene, unremitting pain, persistent complicated osteomyelitis, and nonhealing ulcers.
Evaluation of patients requiring amputation includes a general medical evaluation as well as the specific evaluations required for proper selection of amputation level. It is axiomatic that appropriate measures to prevent amputation have already been accomplished, including revascularization and aggressive wound care. Standard general medical assessment includes a complete history and physical examination, baseline laboratory studies, a chest radiograph, an electrocardiogram (EKG), additional diagnostic studies, and consultations as required. Lower-extremity Doppler assessments are regularly used to predict healing at a given amputation level. Coupled with clinical assessment they are reasonably accurate. Transcutaneous O2 assessment and/or other more sensitive measures of skin blood flow are not routinely used but may prove beneficial. Because these patients are often elderly, frail, and compromised by significant systemic illness, thorough evaluations are essential, and optimal preparation is required prior to amputation to maintain acceptable mortality rates.
The specific management of the limb requiring amputation includes consideration of potential for revascularization to preserve length and function and the management of concurrent infectious problems. When possible, revascularization will often allow the patient to maintain a higher degree of functional status. However, the associated medical problems and rehabilitation potential for each individual patient must be balanced against the incremental peri-operative risk of a bypass procedure. One must consider the potential for bypass failure, reoperation, and subsequent amputation with added mortality and morbidity. Appropriate use of the diagnostic vascular laboratory, angiography, and advanced revascularization techniques, either open or endovascular, may enable revascularization that prevents or provides the opportunity for a more optimal amputation. In most series of lower-extremity revascularization, mortalities range from 2% to 5% and are comparable to those for below-knee amputation.
Because gangrene and/or other infectious problems typically co-exist in patients requiring amputation, careful attention to proper antibiotic therapy and aggressive debridement and wound care is essential. The polymicrobial nature of most infections in these patients, the immunocompromise that accompanies diabetes and other medical illnesses, and the compromised perfusion that results from peripheral vascular occlusive disease make these
considerations challenging. Cellulitis, lymphangitis, and evidence of spreading infection require very careful attention to debridement, antibiotic therapy, and drainage of abscesses. The role of a guillotine amputation followed by definitive amputation therapy must be considered in patients with advanced and aggressively spreading infection.
considerations challenging. Cellulitis, lymphangitis, and evidence of spreading infection require very careful attention to debridement, antibiotic therapy, and drainage of abscesses. The role of a guillotine amputation followed by definitive amputation therapy must be considered in patients with advanced and aggressively spreading infection.
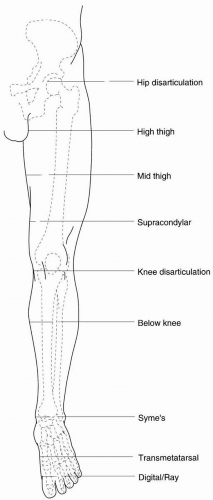
Selection of the level of amputation in elective circumstances is predicated upon several principles. The goal of amputation is to remove all nonviable tissue, relieve the source of ischemic rest pain, ensure primary wound healing, and facilitate rehabilitation. In a general sense, more distal amputations are preferred to more proximal. Ultimately the most functional extremity is the goal. Common amputation levels are indicated in Figure 62-1. The anticipated functional outcome of an amputation must be considered in the decision to perform an amputation at a given level in an individual patient. The more proximal the amputation, the greater the likelihood of primary healing and initial success. Likewise, in nonambulatory patients with limited rehabilitation potential or medically compromised patients with multiple comorbidities (a contracted knee or a paralyzed leg from a prior stroke), an above-knee amputation might be preferable to a below-knee amputation with a risk of subsequent need for revision. These must be carefully individualized decisions, formulated in the context of the individual patient. Rehabilitation potential is critically important to assess prospectively.
There is considerable variability in the energy expenditures required for amputation at various levels (Table 62-1), and this directly influences rehabilitation potential. The status of the contralateral leg is also a critical factor in these considerations.
The tissue most likely to fail in an amputation is skin, and skin blood flow is difficult to assess precisely in most settings. The most common branch point in the decision tree for vascular surgeons is the selection of above- versus below-knee amputation. Clinical judgment alone by an experienced practitioner will accurately predict healing in about 80% of patients undergoing below-knee amputation. Using Doppler techniques, the accuracy of healing prediction can be increased to the mid-90% range. Digital pressures, systemic arterial pressures at various levels, and a variety of nuclear medicine techniques have been used to assess the likelihood of healing. Skin blood flow measurements with fluorescein and transcutaneous oxygen
measurements and a variety of other techniques have also been described but are infrequently used.
measurements and a variety of other techniques have also been described but are infrequently used.
Table 62-1 Rehabilitation Energy Cost of Amputation at Various Levels | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
The major levels of amputation include digital and ray amputation, transmetatarsal, below-knee and above-knee amputation, and rarely, hip disarticulation. The level and selection criteria for each are provided in Figures 62-2, 62-3, 62-4, 62-5 and Tables 62-2, 62-3, 62-4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree