The relation between low-density lipoprotein (LDL) cholesterol levels and clinical outcomes after percutaneous coronary intervention (PCI) in patients with acute myocardial infarction (AMI) has not been described. A total of 9,571 eligible patients (mean age 62.6 ± 12.5 years, 6,967 men) who underwent PCI with a final diagnosis of AMI from the Korea Acute Myocardial Infarction Registry (KAMIR) were divided into 5 groups according to LDL cholesterol level: <70, 70 to 99, 100 to 129, 130 to 159, and ≥160 mg/dl. Clinical outcomes in hospital and 1 and 12 months after PCI in patients with AMI were examined. Age and co-morbidities decreased as LDL cholesterol increased. Patients with higher LDL cholesterol levels had favorable hemodynamic status and laboratory findings. Lifesaving medications, including lipid-lowering drugs, were underused in patients with lower LDL cholesterol levels. Clinical outcomes in hospital and 1 and 12 months after PCI showed better results as LDL cholesterol increased, except for patients with LDL cholesterol levels ≥160 mg/dl. In a Cox proportional-hazards model, LDL cholesterol level was not an independent predictor of mortality at 12 months, after adjusting for clinical characteristics including demographics and biologic data. In conclusion, the cholesterol paradox in patients with AMI is related to confounding by baseline characteristics associated with survival. More intensive treatment including lipid-lowering therapy for AMI in patients with lower LDL cholesterol level may result in better clinical outcomes.
As a part of the Korea Acute Myocardial Infarction Registry (KAMIR) initiative, in this study we investigated the relation between low-density lipoprotein (LDL) cholesterol levels and clinical outcomes after percutaneous coronary intervention (PCI) in patients with acute myocardial infarction (AMI). The aim was to help refine the treatment goal for lipid-lowering therapy and improve outcomes in patients with AMI.
Methods
KAMIR is a prospective, multicenter, observational data collection registry investigating the risk factors of mortality in AMI and establishing the universal management for the prevention of AMI, with the support of Korean Circulation Society since November 2005. The database is comprehensive and includes age, gender, body mass index (BMI), vital signs, Killip class, symptom onset time, door-to-needle time, door-to-balloon time, each risk factor, past regular medications, co-morbidities, electrocardiographic locations of myocardial infarction, initial treatment strategy, and drugs. After every PCI procedure, operators filled in standard report forms including angiographic findings, in-hospital complications, and medical therapy in the hospital and completed 12-month follow-up major cardiac events later.
From November 2005 to January 2008, 9,571 patients (mean age 62.6 ± 12.5 years, 6,967 men) who underwent PCI with a final diagnosis of AMI were enrolled in the KAMIR. Of these patients, the numbers of patients at 1- and 12-month follow-up were 8,603 (mean age 62.4 ± 12.5, 6,271 men) and 7,485 (mean age 62.5 ± 12.4, 5,454 men), respectively. Blood samples except lipid profiles were collected at admission or before PCI. Overnight fasting blood was drawn for lipid measurements. Lipid profiles were measured directly using routine analyses of local hospitals. Clinical data after discharge were collected from outpatient visits and telephone contacts at 1 and 12 months.
All patients in this study underwent PCI. The initial treatment strategy for ST-segment elevation myocardial infarction included PCI, thrombolysis, or conservative treatment. For non–ST-segment elevation myocardial infarction, early invasive PCI or conservative treatment was performed as the initial treatment strategy. The initial treatment strategy for AMI was performed at the discretion of the attending physician on the basis of current guidelines. Primary PCI was defined as emergent PCI performed <12 hours after admission in patients with ST-segment elevation myocardial infarctions. Early invasive PCI was defined as emergent PCI performed <48 hours after admission in patients with non–ST-segment elevation myocardial infarctions. Rescue PCI was defined as emergent PCI for patients with failure of thrombolysis, ongoing ischemic symptoms, cardiogenic shock, severe congestive heart failure, pulmonary edema, or hemodynamically compromising ventricular arrhythmias after thrombolysis or conservative treatment. Optimal evidence-based medical therapies were encouraged in all patients who had no contraindication to drugs before and after discharge.
AMI was diagnosed by clinical features, increased biochemical markers, and electrocardiographic findings. The left ventricular ejection fraction (LVEF) was determined by echocardiography at admission or before PCI. Estimated creatinine clearance was calculated by the use of the Cockcroft-Gault formula : creatinine clearance (ml/min) = [(140 − age) × weight (kg)]/[serum creatinine (mg/dl) × 72], corrected in women by a factor of 0.85. Multivessel disease was defined as >50% diameter stenosis by quantitative coronary angiography in ≥2 coronary arteries or a left main coronary artery lesion. Coronary artery lesion type was determined according to American College of Cardiology and American Heart Association classification. Successful PCI was defined as a residual stenosis <50% in diameter with final Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow.
Patients were categorized into 5 groups according to baseline LDL cholesterol level: <70, 70 to 99, 100 to 129, 130 to 159, and ≥160 mg/dl. We analyzed baseline demographic and clinical characteristics, relevant laboratory results, and treatment strategies. In-hospital complications included hypotension, cardiogenic shock, or arrhythmia, requiring cardiopulmonary resuscitation or the insertion of an intra-aortic balloon pump or temporary cardiac pacemaker. Major cardiac events included death, myocardial infarction, ischemic target vessel revascularization, and coronary artery bypass grafting.
Statistical analysis was performed using SPSS version 17.0 (SPSS, Inc., Chicago, Illinois). All continuous variables are reported as mean ± SD. The relation between age and LDL cholesterol was assessed using bivariate correlation analysis. The cumulative incidence of all-cause death was estimated according to the life table method, and Wilcoxon’s rank test was used to evaluate differences between groups. One-way analysis of variance and the chi-square test for independence and trend were used for baseline demographic and clinical comparisons among 5 groups. Univariate analyses using Pearson’s chi-square test or Student’s t test were performed to evaluate the prognostic significance of demographic and clinical variables for 12-month mortality. The variables tested in univariate analysis were those known to potentially affect outcomes after myocardial infarction and variables showing variation according to LDL cholesterol quintiles. The variables tested were the following; age, gender, BMI, waist-to-hip ratio, systolic blood pressure, diastolic blood pressure, heart rate, Killip class, ST-segment elevation myocardial infarction, family history of coronary artery disease, smoking history, co-morbidities (hypertension, diabetes, dyslipidemia, coronary artery disease, heart failure, stroke, and peripheral vascular disease), the LVEF, glucose, creatinine clearance, high-sensitivity C-reactive protein, N-terminal–pro–B-type natriuretic peptide, multivessel disease, infarct-related artery, coronary artery lesion type, initial and final TIMI flow grade, stent implantation, and medical therapy before and after discharge (aspirin, clopidogrel, cilostazol, β blockers, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, and lipid-lowering drugs). Cox regression analysis was performed to identify independent predictors of 12-month mortality. All continuous variables were converted into categorical variables. After considering univariate analysis results and collinearity among variables, significant variables were entered into a Cox proportional-hazards model in phases. These variables included age, gender, BMI, systolic blood pressure, heart rate, the LVEF, serum glucose, creatinine clearance, high-sensitivity C-reactive protein, N-terminal–pro–B-type natriuretic peptide, ST-segment elevation myocardial infarction, Killip class, family history of coronary artery disease, smoking history, hypertension, diabetes, previous coronary artery disease, previous dyslipidemia, previous heart failure, previous stroke, previous peripheral vascular disease, cilostazol, β blockers, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, lipid-lowering drugs, multivessel disease, left main coronary artery disease, lesion type C, initial TIMI flow grade 0, final TIMI flow grade 3, and stent implantation. All LDL cholesterol groups were independently entered into the model, with the group with LDL cholesterol 130 to 159 mg/dl being the reference. The enter method was used to select the predictive variables. To examine the collinearity among the independent variables, eigenvalues, condition index, and variance proportions were checked using linear regression analysis, which showed no significant collinearity among variables.
Results
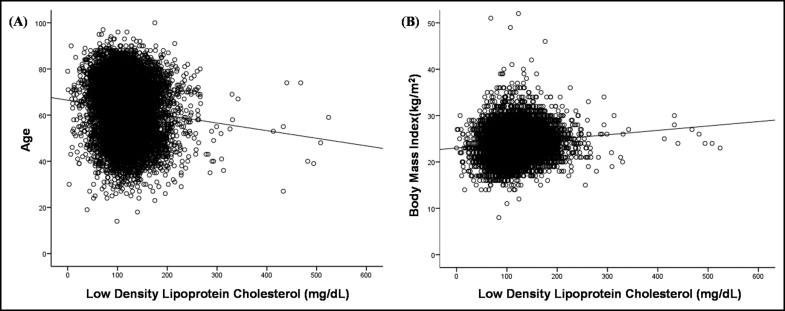
The mean LDL cholesterol level in all patients was 118 ± 43 mg/dl. The mean LDL cholesterol levels were 116 ± 40 mg/dl in men and 123 ± 49 mg/dl in women (p <0.001). LDL cholesterol levels were correlated weakly with age and decreased with increasing age. The correlation between LDL cholesterol level and BMI was positive but weak ( Figure 1 ).
Baseline clinical characteristics and laboratory findings of the patients’ groups are listed in Table 1 . A history of hypertension, diabetes, previous coronary artery disease, previous heart failure, previous stroke, and previous peripheral vascular disease decreased as LDL cholesterol increased. A U-shaped relation between LDL cholesterol level and a history of previous dyslipidemia was observed. The use of lipid-lowering therapy before admission decreased as LDL cholesterol increased, from 9.3% for patients with LDL cholesterol <70 mg/dl to 4.2% for those with LDL cholesterol ≥160 mg/dl (linear p <0.001, data not shown). Waist-to-hip ratio and creatinine clearance decreased as LDL cholesterol level decreased. Patients with higher LDL cholesterol levels had higher systolic blood pressures and LVEFs and lower Killip classes, serum glucose levels, and N-terminal–pro–B-type natriuretic peptide levels, except for patients with LDL cholesterol levels ≥160 mg/dl.
| Characteristic | Serum Level of LDL Cholesterol (mg/dl) | p Value | Linear p Value ⁎ | ||||
|---|---|---|---|---|---|---|---|
| <70 | 70–99 | 100–129 | 130–159 | ≥160 | |||
| (n = 840) | (n = 2,265) | (n = 3,182) | (n = 2,075) | (n = 1,209) | |||
| Age (years) | 65 ± 13 | 64 ± 12 | 63 ± 12 | 61 ± 12 | 60 ± 13 | <0.001 | |
| Men | 609 (73%) | 1,735 (77%) | 2,376 (75%) | 1,465 (71%) | 782 (65%) | <0.001 | <0.001 |
| Body mass index (kg/m 2 ) | 23 ± 4 | 24 ± 3 | 24 ± 3 | 25 ± 4 | 25 ± 4 | <0.001 | |
| Waist-to-hip ratio | 0.936 ± 0.072 | 0.943 ± 0.077 | 0.944 ± 0.068 | 0.947 ± 0.083 | 0.950 ± 0.088 | 0.005 | |
| Systolic blood pressure (mm Hg) | 121 ± 31 | 125 ± 29 | 129 ± 28 | 132 ± 28 | 132 ± 27 | <0.001 | |
| Diastolic blood pressure (mm Hg) | 74 ± 18 | 77 ± 18 | 79 ± 17 | 81 ± 16 | 81 ± 16 | <0.001 | |
| Heart rate (beats/min) | 78 ± 32 | 75 ± 20 | 76 ± 18 | 77 ± 23 | 78 ± 18 | <0.001 | |
| Killip class >1 | 274 (33%) | 565 (26%) | 656 (22%) | 400 (20%) | 281 (24%) | <0.001 | <0.001 |
| ST-segment elevation myocardial infarction | 537 (64%) | 1,537 (68%) | 2,079 (65%) | 1,328 (64%) | 771 (64%) | 0.040 | 0.063 |
| Family history of coronary artery disease | 49 (6%) | 140 (6%) | 221 (7%) | 156 (8%) | 90 (8%) | 0.290 | 0.035 |
| Previous hypertension | 453 (54%) | 1,122 (50%) | 1,488 (47%) | 957 (46%) | 525 (44%) | <0.001 | <0.001 |
| Previous diabetes mellitus | 290 (35%) | 666 (30%) | 805 (25%) | 504 (24%) | 278 (23%) | <0.001 | <0.001 |
| Previous dyslipidemia | 92 (11%) | 194 (9%) | 245 (8%) | 245 (12%) | 175 (15%) | <0.001 | <0.001 |
| Smokers | 466 (56%) | 1,365 (61%) | 1,991 (63%) | 1,225 (59%) | 687 (57%) | <0.001 | 0.530 |
| Previous coronary artery disease | 215 (26%) | 406 (18%) | 383 (12%) | 223 (11%) | 125 (10%) | <0.001 | <0.001 |
| Previous heart failure | 19 (2.3%) | 43 (1.9%) | 30 (0.9%) | 17 (0.8%) | 19 (1.6%) | 0.001 | 0.009 |
| Previous stroke | 68 (8%) | 152 (7%) | 193 (6%) | 111 (5%) | 64 (5%) | 0.031 | 0.002 |
| Previous peripheral vascular disease | 12 (1.4%) | 27 (1.2%) | 25 (0.8%) | 16 (0.8%) | 6 (0.5%) | 0.096 | 0.008 |
| Left ventricular ejection fraction (%) | 50 ± 12 | 51 ± 12 | 52 ± 12 | 52 ± 11 | 52 ± 12 | <0.001 | |
| Serum glucose (mg/dl) | 178 ± 88 | 170 ± 79 | 166 ± 75 | 166 ± 73 | 169 ± 80 | <0.001 | |
| Creatinine clearance (ml/min) | 62 ± 54 | 68 ± 33 | 72 ± 35 | 75 ± 30 | 77 ± 43 | <0.001 | |
| High-sensitivity C-reactive protein (mg/dl) | 16 ± 49 | 13 ± 49 | 9 ± 42 | 13 ± 59 | 16 ± 72 | 0.002 | |
| N-terminal–pro–B-type natriuretic peptide (pg/ml) | 4,083 ± 8,706 | 2,499 ± 6,060 | 1,784 ± 4,438 | 1,701 ± 4,245 | 1,752 ± 4,479 | <0.001 | |
| Total cholesterol (mg/dl) | 127 ± 38 | 154 ± 23 | 180 ± 24 | 209 ± 22 | 253 ± 37 | <0.001 | |
| Triglyceride (mg/dl) | 121 ± 174 | 120 ± 101 | 125 ± 95 | 136 ± 102 | 147 ± 93 | <0.001 | |
| High-density lipoprotein cholesterol (mg/dl) | 42 ± 25 | 45 ± 25 | 45 ± 14 | 46 ± 15 | 48 ± 22 | <0.001 | |
⁎ Statistical significance for linear by linear association between categorical variables, calculated using the chi-square test for trend.
Table 2 lists the findings of coronary angiography and intervention. Proportions of lesions of the left anterior descending coronary artery and stent implantation increased, while that of right coronary artery lesions decreased, as LDL cholesterol level increased. An increasing trend of the proportion of left circumflex coronary artery lesions was observed with increasing values of LDL cholesterol, except for patients with LDL cholesterol levels ≥160 mg/dl. There were no significant differences in the proportions of multivessel disease, lesion type C, initial TIMI grade 0 flow, and final TIMI grade 3 flow.
| Characteristic | Serum Level of LDL Cholesterol (mg/dl) | p Value | Linear p Value ⁎ | ||||
|---|---|---|---|---|---|---|---|
| <70 | 70–99 | 100–129 | 130–159 | ≥160 | |||
| (n = 840) | (n = 2,265) | (n = 3,182) | (n = 2,075) | (n = 1,209) | |||
| Multivessel coronary disease | 476 (58%) | 1,195 (54%) | 1,726 (56%) | 1,164 (58%) | 673 (57%) | 0.143 | 0.253 |
| Infarct-related coronary artery | |||||||
| Left main | 21 (3%) | 41 (2%) | 48 (2%) | 30 (2%) | 21 (2%) | 0.294 | 0.154 |
| Left anterior descending | 357 (44%) | 1,020 (46%) | 1,449 (47%) | 997 (49%) | 591 (50%) | 0.019 | 0.001 |
| Left circumflex | 105 (13%) | 330 (15%) | 551 (18%) | 362 (18%) | 205 (17%) | 0.001 | 0.001 |
| Right | 337 (41%) | 822 (37%) | 1,051 (34%) | 645 (32%) | 369 (31%) | <0.001 | <0.001 |
| Lesion type C | 363 (49%) | 992 (49%) | 1,360 (48%) | 904 (48%) | 513 (47%) | 0.866 | 0.286 |
| Initial TIMI grade 0 flow | 360 (47%) | 944 (45%) | 1,318 (45%) | 871 (45%) | 498 (44%) | 0.842 | 0.361 |
| Stent implantation | 728 (89%) | 2,045 (93%) | 2,914 (94%) | 1,923 (95%) | 1,119 (95%) | <0.001 | <0.001 |
| Stent length (mm) | 25 ± 6 | 25 ± 6 | 25 ± 6 | 25 ± 6 | 25 ± 6 | 0.779 | |
| Stent diameter (mm) | 3.2 ± 0.4 | 3.2 ± 0.4 | 3.2 ± 0.5 | 3.2 ± 0.4 | 3.1 ± 0.4 | 0.404 | |
| Stent number | 1.5 ± 0.8 | 1.5 ± 0.8 | 1.5 ± 0.8 | 1.6 ± 0.9 | 1.5 ± 0.9 | 0.209 | |
| Final TIMI grade 3 flow | 700 (92%) | 1,969 (94%) | 2,739 (94%) | 1,819 (94%) | 1,050 (94%) | 0.287 | 0.341 |
⁎ Statistical significance for linear by linear association between categorical variables, calculated using the chi-square test for trend.
Table 3 lists the types of PCI and medical therapies. There were no significant differences among groups in performing the initial treatment strategy and early or rescue PCI. The use of cilostazol, β blockers, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, and lipid-lowering drugs during hospitalization and cilostazol, β blockers, and lipid-lowering drugs after discharge increased as LDL cholesterol level increased, with significant differences among groups.
| Characteristic | Serum Level of LDL Cholesterol (mg/dl) | p Value | Linear p Value ⁎ | ||||
|---|---|---|---|---|---|---|---|
| <70 | 70–99 | 100–129 | 130–159 | ≥160 | |||
| (n = 840) | (n = 2,265) | (n = 3,182) | (n = 2,075) | (n = 1,209) | |||
| ST-segment elevation myocardial infarction | |||||||
| Primary percutaneous coronary intervention | 422 (79%) | 1,147 (75%) | 1,531 (74%) | 960 (73%) | 579 (75%) | 0.062 | 0.098 |
| Early percutaneous coronary intervention, not primary | 23 (4%) | 96 (6%) | 134 (7%) | 85 (6%) | 38 (5%) | 0.231 | 0.872 |
| Elective percutaneous coronary intervention | 51 (10%) | 188 (12%) | 257 (12%) | 193 (15%) | 102 (13%) | 0.045 | 0.013 |
| Rescue PCI after thrombolysis | 20 (4%) | 51 (3%) | 83 (4%) | 57 (4%) | 30 (4%) | 0.731 | 0.354 |
| Rescue PCI after conservative treatment | 19 (4%) | 52 (3%) | 70 (3%) | 29 (2%) | 20 (3%) | 0.229 | 0.061 |
| Non–ST-segment elevation myocardial infarction | |||||||
| Early invasive percutaneous coronary intervention | 200 (66%) | 525 (72%) | 789 (72%) | 549 (74%) | 300 (69%) | 0.114 | 0.563 |
| Elective percutaneous coronary intervention | 76 (25%) | 144 (20%) | 228 (21%) | 146 (20%) | 103 (24%) | 0.162 | 0.854 |
| Rescue PCI after conservative treatment | 25 (8%) | 57 (8%) | 79 (7%) | 50 (7%) | 33 (8%) | 0.883 | 0.477 |
| Medical therapy during hospitalization | |||||||
| Aspirin | 831 (99%) | 2,240 (99%) | 3,151 (99%) | 2,055 (99%) | 1,193 (99%) | 0.983 | 0.617 |
| Clopidogrel | 819 (98%) | 2,210 (98%) | 3,122 (99%) | 2,046 (99%) | 1,182 (99%) | 0.078 | 0.020 |
| Cilostazol | 246 (29%) | 721 (32%) | 1,055 (33%) | 738 (36%) | 423 (35%) | 0.005 | <0.001 |
| β blockers | 589 (70%) | 1,626 (72%) | 2,369 (75%) | 1,584 (77%) | 922 (77%) | <0.001 | <0.001 |
| Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers | 656 (78%) | 1,825 (81%) | 2,575 (81%) | 1,711 (83%) | 1,028 (86%) | <0.001 | <0.001 |
| Lipid-lowering drugs | 569 (68%) | 1,619 (72%) | 2,553 (81%) | 1,768 (86%) | 1,066 (89%) | <0.001 | <0.001 |
| Medical therapy after discharge | |||||||
| Aspirin | 744 (98%) | 2,142 (99%) | 3,015 (99%) | 1,963 (98%) | 1,145 (99%) | 0.383 | 0.221 |
| Clopidogrel | 726 (96%) | 2,102 (97%) | 2,952 (97%) | 1,941 (97%) | 1,124 (97%) | 0.227 | 0.043 |
| Cilostazol | 236 (31%) | 739 (34%) | 1,074 (35%) | 756 (38%) | 411 (36%) | 0.010 | 0.004 |
| β blockers | 533 (70%) | 1,526 (70%) | 2,241 (73%) | 1,532 (77%) | 889 (77%) | <0.001 | <0.001 |
| Angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers | 620 (82%) | 1,771 (82%) | 2,459 (81%) | 1,660 (83%) | 963 (83%) | 0.084 | 0.090 |
| Lipid-lowering drugs | 499 (66%) | 1,560 (72%) | 2,488 (81%) | 1,744 (88%) | 1,036 (90%) | <0.001 | <0.001 |
⁎ Statistical significance for linear by linear association between categorical variables, calculated using the chi-square test for trend.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


