We sought to determine significant relations between atherogenic lipoproteins and the contribution of calcified plaque (CP), mixed plaque (MP), and noncalcified plaque (NCP) to the total plaque (TP) burden in patients without previous coronary artery disease. From 823 adult patients without previously established coronary artery disease (52% receiving statin therapy, 34% asymptomatic) but with visible coronary plaque on coronary computed tomographic angiography, we obtained segmental CP, MP, NCP, and TP counts from contrast-enhanced, electrocardiographic-gated computed tomography. Multivariate linear regression analysis was used to determine the associations of clinical factors and lipoprotein levels to CP, MP, and NCP counts and CP/TP, MP/TP, and NCP/TP count ratios. Age, male gender, diabetes, smoking, and statin therapy were significantly associated with the CP count (p <0.001, p <0.001, p = 0.049, p = 0.016, and p = 0.003, respectively). Low-density lipoprotein (LDL) cholesterol was significantly associated with MP and NCP counts (all p values ≤0.002). LDL cholesterol was also the only variable to demonstrate significant concurrent relations with CP/TP, MP/TP, and NCP/TP ratios, including an inverse association with CP/TP (p = 0.008) and a positive association with MP/TP (p = 0.032). Analyses using non–high-density lipoprotein cholesterol in place of LDL cholesterol yielded similar results. In conclusion, among the traditional clinical factors used to estimate cardiovascular event risk, LDL cholesterol is associated with an increased MP and NCP burden and is the sole variable that independently predicted relative predominance of CP, MP, and NCP, suggesting a potentially important role for lipoprotein levels in modulating the type of detectable coronary arterial plaque.
Histologic, intracoronary ultrasound, and noninvasive imaging studies have demonstrated that most plaques responsible for acute coronary syndromes contain little or no calcium and suggested that plaques containing both calcified and noncalcified components might be at greatest risk of eventual plaque rupture. In patients without documented coronary artery disease, clinicians routinely use “traditional” risk information—such as the presence of diabetes mellitus, cigarette smoking, blood pressure, and lipid profile—to estimate the long-term chances of experiencing an adverse coronary event. Because of this effort, improving serum low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol profiles frequently becomes a goal of preventive therapy. However, little is known about the connection among lipoprotein levels, statin therapy, and underlying coronary plaque composition. To better characterize these relations, we systematically analyzed a cohort of patients without previous coronary artery disease and in whom coronary computed tomographic angiography detected visible plaque. We hypothesized that LDL cholesterol, HDL cholesterol, and ongoing statin therapy would all demonstrate significant associations with the relative contributions of calcified plaque (CP), noncalcified plaque (NCP), and mixed plaque (MP).
Methods
From September 12, 2006 to November 30, 2008, we identified 823 consecutive adult patients without a previous diagnosis of coronary artery disease in whom coronary artery plaque was detected on coronary computed tomographic angiography. All coronary computed tomographic angiograms were performed within 30 days of the fasting lipid profile evaluation. All patients gave informed consent. The Cedars-Sinai institutional review board approved by the present study.
The demographics, medical history, and risk factors were collected. Hypertension was defined as a previously established diagnosis, systolic blood pressure >140 mm Hg, diastolic blood pressure >90 mm Hg, or antihypertensive use. Smoking was defined as any cigarette smoking within 1 year of the coronary computed tomographic angiographic date. Diabetes mellitus was defined as a previously established diagnosis, insulin or oral hypoglycemic therapy, fasting glucose of ≥126 mg/dl, or nonfasting glucose of ≥200 mg/dl. Family coronary artery disease history was defined as myocardial infarction, coronary revascularization, or sudden cardiac death in a first-degree male relative <55 years old or female relative <65 years old. Lipid profiles were obtained by processing a fasting blood sample in the Cholestec LDX System analyzer (Cholestec, Hayward, California). Hypercholesterolemia was defined according to the National Cholesterol Education Panel guidelines or by the current use of lipid-lowering medication.
Coronary computed tomographic angiography was performed using the Somatom Definition dual-source CT scanner (Siemens Medical Systems, Forchheim, Germany). Patients received oral and/or intravenous metoprolol as needed to attain a heart rate of <70 beats/min. An initial noncontrast coronary calcium scan was performed, using triggering at a heart-rate dependent percentage of the RR interval, 350-mm field of view, 2.5-mm slice thickness, 120-kVp tube voltage, and 42-mA tube current. After a sublingual spray of 0.4 mg nitroglycerin (Sciele Pharma, Alpharetta, Georgia), 80 to 92 ml of intravenous iodinated contrast (Omnipaque or Visipaque, GE Healthcare, Princeton, New Jersey), followed by 50 to 80 ml of saline, were power injected into the antecubital vein. The detection of ≥100 Hounsfield units in the ascending aorta initiated electrocardiographic-gated scanning, from 1 cm below the tracheal bifurcation to just below the diaphragm, during a single breath-hold. Scanning parameters included heart-rate dependent pitch (0.2 to 0.45), 330-ms gantry rotation time, 100- or 120-kVp tube voltage, and ≤600-mA tube current (≤330 mA for 100 kVp). A tube voltage of 100 kVp was used in the patients with a body mass index <30 kg/m 2 , weight <85 kg, and no more than mild calcification in the proximal coronary arteries on the noncontrast scan.
Retrospectively gated reconstruction of the coronary computed tomographic angiographic data were performed at end-systole and in diastole with 0.6-mm slice thickness (0.75 mm if the body mass index was >35 kg/m 2 ), 0.3-mm slice increment, 250-mm field-of-view, 512 × 512 matrix, and the B26f medium “smooth” kernel (B46f “sharp” kernel was also used for patients with dense coronary calcium). Reconstructed data were analyzed using the Vitrea 2 software package (Vital Images, Minnetonka, Minnesota). Two readers consensually evaluated each study using interactive axial, oblique, and curved displays to determine the presence of any plaque and plaque composition. Detected plaques were assigned locations according to a 19-segment version of the 15-segment American Heart Association coronary tree model (with the addition of distal left circumflex, ramus intermedius, third diagonal, and third obtuse marginal segments).
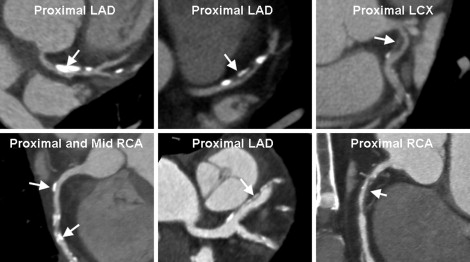
The noncalcified component of a plaque was defined as a lesion with a radiodensity greater than neighboring soft tissue and lower than the luminal contrast. The calcified component of a plaque was defined as a lesion with a radiodensity greater than the luminal contrast. Plaques exhibiting <25% calcified component by volume on visual inspection were categorized as NCP; 25% to 75% as MP and >75% as CP ( Figure 1 ). In segments containing more than one plaque, the characteristics of the most stenotic plaque were recorded. The numeric ratios of NCP, MP, and CP to the total number of plaques (TP) were calculated for each patient.
For descriptive analysis, continuous variables are expressed as the mean ± SD and categorical variables as percentages. Our primary statistical testing examined LDL cholesterol and HDL cholesterol. Multivariate linear regression analyses were performed to first evaluate the associations between individual cardiovascular risk profile components (age, gender, body mass index, diabetes, hypertension, smoking, family coronary artery disease history, current statin therapy, LDL cholesterol, and HDL cholesterol) and absolute CP, MP, and NCP counts and then between the same components and CP/TP, MP/TP, and NCP/TP ratios. In our secondary statistical testing, the same regression analyses were performed with non-HDL cholesterol (HDL cholesterol subtracted from total cholesterol) in place of LDL cholesterol and HDL cholesterol. Because CP, MP, and NCP counts and CP/TP, MP/TP, and NCP/TP ratios were generated for every patient, every patient contributed equally to all analyses. By definition, CP/TP, MP/TP, and NCP/TP must total 1 for each patient; thus, CP/TP and (MP + NCP) / TP were exactly inversely related for all analyses. Model stability was verified by varying the number and combination of predictors. For regression models that evaluated CP/TP, MP/TP, and NCP/TP ratios, all potential 2 × 2 interactions among model variables were tested for significance using the Wald test, both singly with the main effects and in the full model, using a relaxed α level of <0.1. No significant interaction was found. Associations with p <0.05 were considered significant. Standardized coefficients were calculated to estimate the strength of the significant associations.
Results
The study patients were predominantly men (64%), with a mean age of 65 ± 12 years (range 27 to 94), mean body mass index of 27 ± 5 kg/m 2 , and the following risk factor prevalences: hypertension 67%, hypercholesterolemia 67%, family coronary artery disease history 42%, diabetes mellitus 19%, and smoking 10%. In this population, 34% were asymptomatic (23% were referred for risk stratification, 3% for abnormal or equivocal stress testing results, 3% before noncoronary surgery, 2% for an aortic or a noncoronary cardiac structure evaluation, 1% for cardiomyopathy, and 2% for other reasons), and 24% had typical angina. The patients receiving active statin therapy (52%) had lower mean LDL cholesterol (88.3 ± 31.9 vs 111.9 ± 38.7 mg/dl, p <0.001) and similar mean HDL cholesterol (50.1 ± 16.3 vs 48.1 ± 17.0 mg/dl, p = 0.09). The mean coronary calcium score (available for 800 patients) was 412 ± 682.
Coronary computed tomographic angiography identified 3,849 total plaques. The absolute CP, MP, and NCP counts were 2,457, 997, and 395, constituting 64%, 26%, and 10% of the TP count, respectively. The median TP count was 4 (range 1 to 17). CP only was found in 292 patients (35%), MP only in 69 patients (8%), and NCP only in 28 patients (3%; 20 of these patients had a calcium score of 0). The remaining 434 patients (53%) had more than one type of plaque.
Table 1 summarizes the variables that exhibited significant associations with the absolute CP, MP, and NCP counts. In the primary analyses, age, male gender, diabetes, smoking, and ongoing statin therapy were positively associated with the CP count. Male gender, ongoing statin therapy, and LDL cholesterol (p = 0.001) were positively associated with the MP count. LDL cholesterol (p = 0.001) alone was positively associated with the NCP count. In the secondary analyses, non-HDL cholesterol exhibited positive associations with MP count (p = 0.002) and NCP count (p <0.001), with preservation of all other significant associations from the LDL cholesterol-based analyses.
| Variable | β-Coefficient ± SE | Standardized Coefficient | p Value |
|---|---|---|---|
| Calcified plaque count | |||
| Age, per year | 0.069 ± 0.009 | 0.800 | <0.001 |
| Male gender | 0.995 ± 0.212 | 0.479 | <0.001 |
| Diabetes mellitus | 0.502 ± 0.255 | 0.197 | 0.049 |
| Smoking within 1 year | 0.772 ± 0.320 | 0.230 | 0.016 |
| Current statin therapy | 0.589 ± 0.199 | 0.294 | 0.003 |
| Mixed plaque count | |||
| Male gender | 0.352 ± 0.134 | 0.169 | 0.009 |
| Current statin therapy | 0.280 ± 0.126 | 0.140 | 0.026 |
| Low-density lipoprotein cholesterol, per mg/dl | 0.006 ± 0.002 | 0.216 | 0.001 |
| Non–high-density lipoprotein cholesterol, per mg/dl ⁎ | 0.005 ± 0.001 | 0.197 | 0.002 |
| Noncalcified plaque count | |||
| Low-density lipoprotein cholesterol, per mg/dl | 0.004 ± 0.001 | 0.133 | 0.001 |
| Non-high-density lipoprotein cholesterol, per mg/dl ⁎ | 0.004 ± 0.001 | 0.163 | <0.001 |
⁎ All multivariate regression models adjusted for continuous variables of age, body mass index, LDL cholesterol, and HDL cholesterol (or non-HDL cholesterol in place of LDL cholesterol and HDL cholesterol, as noted) and binary variables of gender, diabetes, hypertension, smoking, family coronary artery disease history, and current statin therapy.
The primary analyses of CP/TP, MP/TP, and NCP/TP ratios found significant associations only with LDL cholesterol. Each milligram per deciliter increase in LDL cholesterol showed a strong inverse association with the CP/TP ratio (p = 0.008) and a positive association with the MP/TP ratio (p = 0.032). Similarly, in the secondary analyses, significant associations were only found with non-HDL cholesterol. Each milligram per deciliter increase in non-HDL cholesterol showed a strong inverse association with the CP/TP ratio (p = 0.002) and positive associations with the MP/TP (p = 0.050) and NCP/TP (p = 0.033) ratios. These findings are summarized in Table 2 . The predicted plaque type ratios by linear regression modeling of LDL cholesterol and non-HDL cholesterol are shown in Figures 2 and 3 .
| Variable | β-Coefficient ± SE | Standardized Coefficient | p Value |
|---|---|---|---|
| CP/TP ratio | |||
| Low-density lipoprotein cholesterol, per mg/dl | −0.098 ± 0.037 | −3.671 | 0.008 |
| Non–high-density lipoprotein cholesterol, per mg/dl ⁎ | −0.101 ± 0.033 | −4.265 | 0.002 |
| MP/TP ratio | |||
| Low-density lipoprotein cholesterol, per mg/dl | 0.070 ± 0.033 | 2.603 | 0.032 |
| Non–high-density lipoprotein cholesterol, per mg/dl ⁎ | 0.056 ± 0.029 | 2.373 | 0.050 |
| NCP/TP ratio | |||
| Non–high-density lipoprotein cholesterol, per mg/dl ⁎ | 0.045 ± 0.021 | 1.892 | 0.033 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


