The aim of the present study was to report the short- and long-term clinical outcomes of percutaneous coronary intervention in young women with premature coronary artery disease. From February 2003 to December 2011, 168 consecutive women aged ≤45 years who underwent percutaneous coronary intervention with stent implantation were retrospectively analyzed. The primary end point was the incidence of major adverse cardiac events (MACEs) at short- and long-term follow-up. The mean age was 40.3 ± 2.0 years. Conventional coronary artery disease risk factors were common. Autoimmune or connective tissue diseases were present in 6.5% of the population, 4% had gynecologic diseases, 4 were postpartum, and 9 were taking contraceptives. The left anterior descending coronary artery was the most commonly affected vessel (83.3%) and the most common target vessel for stenting (76.8%). A total of 268 stents were implanted, 95.3% of which were drug-eluting stents. During the hospital stay, 1 patient died, and the incidence of MACEs was 1.2%. No additional events had occurred at 30-day follow-up. After a median follow-up duration of 36 months (interquartile range 12 to 60), cumulate MACE-free survival was 80.5%, the rate of target vessel revascularization was 16.5%, and the rate of stent thrombosis was 3.6%. Cox regression showed that hypertension, smoking, a left ventricular ejection fraction <50%, anterior myocardial infarction, and autoimmune disease were independent predictors of MACEs. In conclusion, percutaneous coronary intervention in young women tends to result in an increased rate of target vessel revascularization during long-term follow-up, which may be influenced by conventional and nonconventional risk factors.
Data have shown an increase in the coronary death rate among young women, more prominent than in young men. This is due to steady increases of a spectrum of unfavorable coronary risk factors, such as obesity, diabetes mellitus, hypertension, and metabolic syndrome. Previous studies have reported that the prognosis of young patients who undergo percutaneous coronary intervention (PCI) is good. However, the numbers of young women in these studies have been limited. In some young women with coronary artery disease (CAD), the underlying pathophysiology is not atherosclerotic, and the risk factors and clinical characteristics in this subset of patients are not equivalent to traditional CAD. However, the impact of PCI on the clinical outcomes of young women with CAD has rarely been investigated. Thus, the aim of this study was to report short- and long-term clinical outcomes in a consecutive series of young women with CAD who underwent PCI with stent implantation.
Methods
One hundred sixty-eight consecutive female patients aged 20 to 45 years who underwent PCI and bare-metal stent or drug-eluting stent (DES) implantation for CAD were included from a large cardiac catheterization registry with a yearly volume of 4,000 to 8,000 PCIs from February 2003 to December 2011. CAD was diagnosed if a stenosis >70% was found in a major epicardial coronary artery.
Conventional risk factors included obesity, smoking, hypertension, hyperlipidemia, and diabetes mellitus. Triglyceride, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol levels were assessed without interruption of previous medical therapy, including lipid-lowering drugs. Hyperlipidemia was defined as total cholesterol >200 mg/dl, low-density lipoprotein cholesterol >130 mg/dl, high-density lipoprotein cholesterol <40 mg/dl, or triglyceride >150 mg/dl. The height and weight of each patient were measured at the time of admission, and body mass index was calculated. A body mass index of 18.5 to 24.9 kg/m 2 was considered normal, a body mass index of 25 to 30 kg/m 2 was considered overweight, and a body mass index >30 kg/m 2 was considered obese. Fasting blood glucose levels were obtained within the first 72 hours of hospitalization. Diabetes mellitus was diagnosed by a fasting blood glucose level >125 mg/dl (7.0 mmol/L), a random plasma glucose level >200 mg/dl (11.1 mmol/L), or a history of diabetes mellitus, including those treated with diet control, oral medications, or insulin. Hypertension was diagnosed if blood pressure averaged (>3 values) >140/90 mm Hg during admission or if a previous diagnosis of hypertension had been made.
Family history was defined as premature coronary heart disease at <55 years of age in a male and <65 years of age in a female first-degree relative, respectively. Smoking was defined as current or former smoking (quit >1 month before the onset of disease). Patients who had stopped smoking >2 years before the onset of disease were classified as nonsmokers.
No patient was excluded from the analysis. All patients provided written informed consent, and the ethics committee approved the database. All patients were advised to continue lifelong aspirin 100 mg/day and clopidogrel 75 mg/day for ≥12 months if appropriate.
All available inpatient and outpatient medical records were reviewed. Information regarding the clinical status at the latest clinical follow-up available was collected by clinical visits and telephone interviews.
The primary end point of our study was the incidence of major adverse cardiac events (MACEs), including cardiac death, myocardial infarction (MI), and target vessel revascularization (TVR; repeat PCI or coronary artery bypass grafting [CABG]) at immediate (in-hospital), short-term (30 days and 1 year), and long-term (median 3 years) follow-up.
Cardiac death was defined as any death from a cardiac cause (e.g., MI, low-output heart failure, fatal arrhythmia), procedure-related death, and death from an unknown cause. Target lesion revascularization was defined as any repeat intervention or CABG of the target lesion. The target lesion was defined as the treated segment 5 mm proximal to the stent and 5 mm distal to the stent. TVR was defined as any repeat intervention or CABG of any segment of the target vessel. The target vessel was defined as the entire major coronary vessel proximal and distal to the target lesion, including upstream and downstream branches, including the target lesion. Diagnosis of MI was made using the American College of Cardiology and European Society of Cardiology guidelines for acute, evolving, or recent MI. ST-segment elevation and non–ST-segment elevation MI were included. These guidelines require a characteristic increase and decrease of troponin or creatine kinase-MB with ≥1 of the following: ischemic symptoms, the development of pathologic Q waves on electrocardiography, ST-segment elevation or depression, coronary intervention, or pathologic findings of an acute MI. The occurrence of stent thrombosis was defined on the basis of the Academic Research Consortium definition. Stent thrombosis was defined as acute, subacute, late, or very late if the event occurred <24 hours, <30 days, <1 year, or >1 year after the procedure, respectively.
All continuous variables are reported as mean ± SD and categorical variables as frequencies. Cumulative event rates were evaluated using Kaplan-Meier curves. Cumulative events were calculated at 2-year and median follow-up. Univariate and multivariate analyses were performed to identify independent predictors of adverse events. Specifically, all variables significantly associated with the clinical event of interest on univariate analysis (p <0.10) were entered into subsequent models. After appropriate checks for underlying assumptions, multivariate Cox proportional-hazards analyses were performed for all pertinent covariates. The results of the multivariate Cox analyses are reported as hazard ratios (HRs) with 95% confidence intervals (CIs) and p values. A 2-tailed p value <0.05 was considered statistically significant. All analyses were performed using SPSS for Windows version 18.0.1 (SPSS, Inc., Chicago, Illinois).
Results
The baseline characteristics of participants are listed in Table 1 . From February 2003 to December 2011, 168 patients (average age 40.3 ± 2.0 years) underwent PCI and stent implantation. One hundred fifty-seven of the patients (93.5%) had ≥1 of the conventional risk factors (hypertension 51.6%, hyperlipidemia 72%, smoking 4.8%, overweight 43.9%, family history 10.8%, diabetes 31.8%). Forty patients (30%) had blood pressure >140/90 mm Hg on admission, almost half had low high-density lipoprotein cholesterol (<40 mg/dl), and 1/3 had high triglyceride (>150 mg/dl).
| Characteristic | Value |
|---|---|
| Age (yrs) | 40.3 ± 2.0 |
| Hypertension | 81 (51.6%) |
| Low-density lipoprotein >130 mg/dl | 29 (17.3%) |
| High-density lipoprotein <40 mg/dl | 83 (49.4%) |
| Triglyceride >150 mg/dl | 56 (33.3%) |
| Diabetes | 50 (31.8%) |
| Family history of early CAD | 17 (10.8%) |
| Smoker | 8 (4.8%) |
| Overweight (body mass index 25–30 kg/m 2 ) | 69 (43.9%) |
| Obese (body mass index >30 kg/m 2 ) | 17 (10.8%) |
| Autoimmune disease ∗ | 11 (6.5%) |
| Gynecologic disease | 6 (3.6%) |
| Postpartum | 4 (2.4%) |
| Contraceptives taking | 9 (5.4%) |
| Menopause | 0 |
| Old acute MI | 8 (4.7%) |
| Previous CABG | 2 (1.2%) |
| Previous PCI | 10 (6.0%) |
| Clinical presentation | |
| Non–ST-segment elevation MI | 11 (6.5%) |
| Anterior MI | 22 (13.1%) |
| Inferior MI | 21 (12.5%) |
| Unstable angina pectoris | 86 (51.2%) |
| Chronic renal failure | 3 (1.8%) |
| Chronic heart failure | 5 (2.97%) |
| Left ventricular ejection fraction <50% | 9 (5.7%) |
∗ Autoimmune diseases included rheumatic arthritis and Sjögren’s syndrome (n = 2), Takayasu’s arteritis (n = 4), systemic lupus erythematosus (n = 1), Graves’ disease (n = 1), thymoma (n = 1), myositis (n = 1), and membranous nephropathy (n = 1).
Autoimmune or connective tissue diseases were present in 6.5% of the population. About 4% of the population also had gynecologic diseases, 4 of whom had ovarian disease (oophoritic cysts or ovariotomy) and 2 of whom had uterine disease (endometriosis or hysterectomy). Four patients had symptoms beginning <6 months postpartum.
ST-segment elevation MI was the clinical presentation in 25.7% of the population. ST-segment elevation MI was also more frequent in patients with autoimmune or connective tissue disease (54.5%). All 9 patients who were taking contraceptives presented with acute MI (3 with non–ST-segment elevation MI, 6 with ST-segment elevation MI).
Coronary angiographic characteristics are listed in Table 2 . Single-vessel disease was present in 2/3 of patients, often involving the left anterior descending coronary artery (84.3%). A total of 12 bare-metal stents and 256 DES (95.6%) were implanted. Spontaneous dissection was noted in 3 patients, 2 of whom were postpartum. Of these, 2 patients were diagnosed by coronary angiography and 1 by intravascular ultrasound and optical coherence tomography.
| Characteristic | Value |
|---|---|
| Single-vessel disease | 117 (69.6%) |
| Triple-vessel disease | 18 (10.7%) |
| Diseased coronary artery | |
| Left main | 13 (7.7%) |
| Left anterior descending | 140 (83.3%) |
| Left circumflex | 42 (25%) |
| Right | 50 (29.8%) |
| Spontaneous coronary dissection | 3 (1.7%) |
| Average number of treated vessels | 1.3 ± 0.5 |
| Stented coronary artery | |
| Left main | 10 (6%) |
| Left anterior descending | 129 (76.8%) |
| Left circumflex | 32 (19%) |
| Right | 42 (25%) |
| Bifurcation stent | 5 (3%) |
| Average number of stents per vessel | 1.5 ± 1.0 |
| Average stent length per vessel (mm) | 27.8 ± 14.1 |
| Bare-metal stents | 12 (4.4%) |
| DES | 256 (95.6%) |
The incidence of in-hospital, short-term (30 days and 1 year), and long-term (median 3 years) adverse events is reported in Table 3 . During the hospital stay, there was 1 death secondary to acute thrombosis after left main coronary artery DES implantation in a patient with Takayasu’s arteritis. One acute MI occurred secondary to acute thrombosis in a patient who took contraceptives. The incidence of in-hospital MACEs was 1.2%.
| Event | In Hospital | 30 Days | 1 Year | Long Term |
|---|---|---|---|---|
| MACEs | 2 (1.2%) | 2 (1.2%) | 18 (10.7%) | 32 (19%) |
| Death | 1 (0.6%) | 1 (0.6%) | 3 (1.8%) | 4 (2.4%) |
| Acute MI | 2 (1.2%) | 2 (1.2%) | 3 (1.8%) | 7 (4.2%) |
| Non–ST-segment elevation MI | 2 (1.2%) | 2 (1.2%) | 2 (1.2%) | 3 (1.8%) |
| ST-segment elevation MI | 0 | 0 | 1 (0.6%) | 4 (2.4%) |
| Target lesion revascularization | 1 (0.6%) | 1 (0.6%) | 14 (8.3%) | 22 (13.2%) |
| TVR | 1 (0.6%) | 1 (0.6%) | 17 (10.1%) | 28 (16.7%) |
| Repeat PCI | 1 (0.6%) | 1 (0.6%) | 13 (7.8%) | 21 (12.5%) |
| Repeat CABG | 0 (0) | 0 (0) | 4 (2.4%) | 7 (4.2%) |
| Stent thrombosis | 2 (1.2%) | 2 (1.2%) | 3 (1.8%) | 6 (3.6%) |
At 30-day follow-up, no additional adverse events had occurred. After a median follow-up period of 36 months (interquartile range 15 to 60), 3 patients had died. Two patients died within 1 year, 1 from heart failure and the other during CABG for revascularization of an in-stent stenosis. The last patient died 2 years after index PCI. Overall mortality was 2.4%, and the incidence of MI was 4.2%.
Coronary angiographic follow-up was performed in 60% of patients, of whom 59 were readmitted for ischemic events. In-stent restenosis was found in 30 patients (28 with DES, 2 with bare-metal stents), and 28 underwent TVR (21 repeat PCI, 7 repeat CABG). Most TVR (63%) occurred within the first year after stent implantation. Three patients had new lesions and underwent revascularization. One patient had a stent fracture <1 year after sirolimus-eluting stent implantation.
Stent thrombosis occurred in 6 patients (3.5%): 2 acute, 1 late, and 3 very late. Of these patients, 3 had autoimmune disease (1 with rheumatic arteries and Sjögren’s syndrome, 2 with Takayasu’s arteritis).
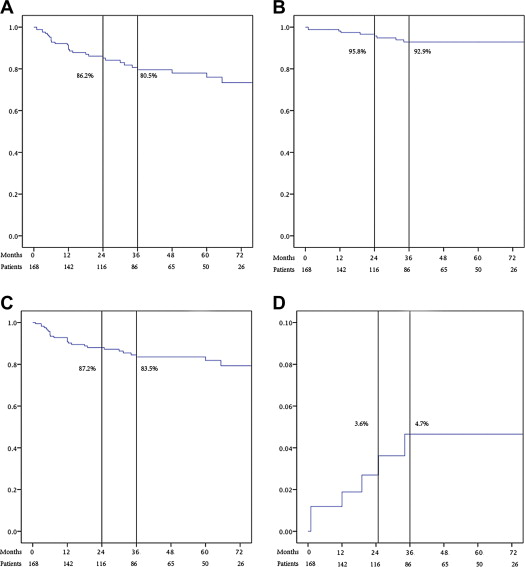
Kaplan-Meier survival curves of cumulative MACEs, death or MI, TVR-free survival, and stent thrombosis are shown in Figure 1 . Cumulative MACE-free survival at 2 and 3 years was 86.2% and 80.5%, respectively. TVR-free survival at 2 and 3 years was 87.2% and 83.5%, respectively. Cumulative rates of stent thrombosis at 2 and 3 years were 3.6% and 4.7%, respectively.