The prognostic value of dobutamine stress echocardiography (DSE) at >10-year follow-up is unknown. The aim of this study was to assess the very long-term prognostic value of DSE in a high-risk cohort of patients with known or suspected coronary artery disease. This prospective, single-center study included 3,381 patients who underwent DSE from January 1990 to January 2003. Two-dimensional echocardiographic images were acquired at rest, during dobutamine stress, and during recovery. Follow-up events were collected and included overall mortality, cardiac death, nonfatal myocardial infarction, and revascularization. The incremental value of DSE in the prediction of selected end points was evaluated using multivariate Cox proportional hazard analysis. During a mean follow-up of 13 ± 3.2 years (range 7.3 to 20.5 years), there were 1,725 deaths (51%), of which 1,128 (33%) were attributed to cardiac causes. Patients with an abnormal DSE had a higher mortality rate (44% vs 35% at 15-year follow-up, p <0.001) than those with a normal DSE. When comparing echocardiographic variables at rest to variables at maximum dose dobutamine, the chi-square of the test improved from 842 to 870 (p <0.0001) and from 684 to 740 (p <0.0001) for all-cause mortality and cardiac death, respectively. DSE provided incremental value in predicting all-cause mortality, cardiac death, and hard cardiac events. There seems, however, to be a “warranty period” of approximately 7 years, when the survival curves of a normal and abnormal DSE no longer diverge.
Exercise electrocardiography is the most frequently used method for noninvasive evaluation of coronary artery disease (CAD). Still, a substantial number of patients have an impaired exercise capacity, because of a weak general physical condition, neuropathy, or peripheral vascular disease. Dobutamine stress echocardiography (DSE) has been reported as a safe and effective noninvasive tool to provide diagnostic and prognostic information in various clinical scenarios. Currently, it is not known whether the prognostic value of DSE in patients with limited exercise capacity is preserved at very long-term (>10 years) follow-up. The goals of this study were to assess the very long-term outcome after DSE in a high-risk group of consecutive patients and to evaluate whether DSE has incremental prognostic value over clinical variables and echocardiographic data at rest.
Methods
This prospective study included 3,875 consecutive patients at high risk with known or suspected CAD, who were unable to perform an adequate exercise test. Indications for DSE were diagnosis of CAD (54%), preoperative evaluation before noncardiac surgery (34%), and risk stratification after myocardial infarction (MI, 12%). Of all patients who underwent DSE, 30% had a history of typical angina, and 13% had a history of atypical angina. Data were collected from patients who underwent DSE from January 1990 to January 2003 at the Thoraxcenter, Rotterdam, the Netherlands. Follow-up data at shorter intervals and of specific subgroups of this study cohort have been previously published. Thirty-nine patients were lost to follow-up, and 455 patients underwent early coronary revascularization in the first 60 days after DSE and were excluded from the analysis because referral for revascularization within this period is likely to be based on DSE results. The final population of this study consisted of 3,381 patients. This study was not subject to the Dutch Medical Research Involving Human Subjects Act. Therefore, approval from the local research ethics committee to conduct this prospective follow-up study was not required at the time of enrollment. The study was conducted according to the Declaration of Helsinki. All patients consented participation in this study.
Clinical characteristics including hypertension, hypercholesterolemia, smoking, previous MI, a history of heart failure, and/or revascularization were recorded at the time of DSE in a computerized database. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or the use of antihypertensive medication. Hypercholesterolemia was defined as total cholesterol >200 mg/dl or the use of cholesterol-lowering agents. Heart failure was defined according to the New York Heart Association classification and based on established guidelines at the time of diagnosis.
After baseline echocardiography, dobutamine was infused at a starting dose of 5 μg/kg/min for 3 minutes followed by 10 μg/kg/min for 3 minutes (low-dose stage). The dobutamine dose was increased by 10 μg/kg/min every 3 minutes up to a maximum dose of 40 μg/kg/min. Atropine (up to 1 mg) was administered intravenously at the end of the last stage if the target heart rate was not achieved. End points of the test were an achievement of the target heart rate (85% of the maximal heart rate predicted for age), the maximal dose of dobutamine and atropine, >2 mV downsloping ST-segment depression measured 80 ms from the J point compared with baseline, hypertension (blood pressure >240/120 mm Hg), a decrease in systolic blood pressure of >40 mm Hg, and significant arrhythmias.
Two-dimensional echocardiographic images were acquired at rest, during dobutamine stress, and during recovery using standard views. Regional wall motion and systolic wall thickening were scored on a 5-point scale using a standard 16-segment left ventricular model. Ischemia was defined as new or worsened wall motion abnormalities (WMA) during stress indicated by an increase of wall motion score ≥1 grade in ≥1 segment. A biphasic response in an akinetic or severely hypokinetic segment was considered as an ischemic response. Ischemia was not considered present when akinetic segments at rest became dyskinetic during stress. For each patient, a wall motion score index (WMSI) was calculated by dividing the sum of segment scores by the total number of interpreted segments. The test was considered abnormal if WMA were seen either at rest or during stress.
Outcome data were obtained by a questionnaire, evaluation of hospital records, contacting the patient’s general practitioner, and/or review of civil registries. The cause of death was retrieved at Statistics Netherlands ( www.cbs.nl ). This permitted high accuracy for determination of survival status. Deaths were classified as either documented cardiac death or other. Before contacting the patient, the online municipal civil registry was used to determine the patient’s present survival status. Survival status was retrieved in 99% of the patients. Questionnaires were sent to all patients alive. The response rate of this questionnaire was 83%. The date of response was used to calculate follow-up time. Follow-up events noted were overall mortality, hard cardiac events (non-fatal MI and cardiac death), and revascularization.
Continuous data are expressed as mean values ± SD. The Student t test was used to analyze continuous data, and the chi-square test was used for differences between proportions. The incremental value of DSE over the clinical variables in the prediction of selected end points was evaluated using multivariate Cox proportional hazard analysis (SPSS Software, version 21.0) including a model with baseline characteristics and clinical variables. Only variables that were significant in a univariate model were added to the multivariate model. Using a stepwise model, echocardiographic variables at rest were then added to the clinical model to investigate the increase in chi-square value of the model. Finally, the variables at peak-dose dobutamine were added to the model. The test was considered of additional value if there was a significant increase in chi-square value at the third step of the test. The echocardiographic variables that were added at rest and peak-dobutamine dose were heart rate, systolic and diastolic blood pressure, rate pressure product (defined as maximum heart rate times the maximum systolic blood pressure), WMSI, and WMA. The probability of survival was calculated using the Kaplan–Meier method, and survival curves were compared using the log-rank test. To determine the warranty period of DSE, the Cox proportional hazard analysis for an abnormal DSE was repeated at 1, 2, 3, and so on years of follow-up. A p value <0.05 was considered statistically significant.
Results
Mean age at time of DSE was 61 ± 12 years. There were 2,275 men (67%) and 1,106 women (33%). Forty-five percent of the patients had known CAD. Clinical characteristics are presented in Table 1 . The test was terminated for achievement of the target heart rate in 89% of the patients, maximal dobutamine/atropine dose in 3%, ST-segment changes in 3%, arrhythmias in 1%, severe angina in 1%, abnormal blood pressure in 1%, and other symptoms in 2%. Five hundred sixty-eight (17%) patients had typical angina during dobutamine stress.
| Variable | n = 3,381 |
|---|---|
| Men | 2,275 (67%) |
| Age (yrs) | 61.4 ± 12 |
| Hypertension | 1,005 (30%) |
| Hypercholesterolemia | 770 (23%) |
| Smoking | 988 (29%) |
| Diabetes mellitus | 378 (11%) |
| Heart failure | 454 (13%) |
| Coronary artery disease | 1,525 (45%) |
| Beta-blockers | 1,116 (33%) |
| Calcium-channel blockers | 816 (24%) |
| Angiotensin-converting-enzyme inhibitor | 845 (25%) |
| Diuretics | 477 (14%) |
| Nitrates | 1,031 (31%) |
DSE was normal in 1,170 of the patients (35%). Ischemia on DSE was detected in 1,610 patients (48%); of which 1,441 (90%) had WMA at rest. Six hundred one (18%) patients had WMA at rest alone. During a mean follow-up of 13 ± 3.2 years (range 7.3 to 20.5 years), there were 1,725 deaths (51%), of which 1,128 (33% of total study cohort) were attributed to cardiac causes. Two hundred ninety-seven patients (8.8%) had a nonfatal MI, and 793 patients were revascularized (23.5%) at during follow-up. The annualized mortality rate of patients who underwent revascularization after an ischemic event was comparable to the group who did not undergo percutaneous coronary intervention (3.9% vs 4.2%, respectively).
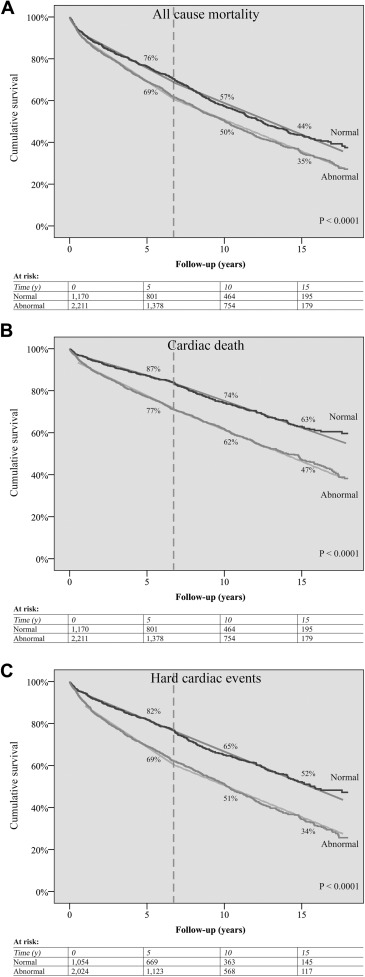
Cumulative survival curves ( Figure 1 ) showed a significantly better survival of patients with normal DSE in comparison with abnormal DSE (76% vs 69% at 5 years, 57% vs 50% at 10 years, and 44% vs 35% at 15 years; overall p <0.001). Figure 1 illustrates that also for the end points cardiac death (87% vs 77% at 5 years, 74% vs 62% at 10 years, and 63% vs 47% at 15 years; overall p <0.001) and hard cardiac events (82% vs 69% at 5 years, 65% vs 51% at 10 years, and 52% vs 34% at 15 years; overall p <0.001), the population with a normal DSE had significant lower chance of adverse events.
Univariate and multivariate predictors associated with an increased risk of all end points of interest are presented in Tables 2 and 3 . Echocardiographic variables at peak-dose dobutamine significantly increased the value of the test for all end points. When comparing echocardiographic variables at rest to variables at maximum dose dobutamine, the chi-square of the test improved from 842 to 870 (p <0.0001) and from 684 to 740 (p <0.0001) for all-cause mortality and cardiac death, respectively. WMSI during stress predicted both all-cause mortality and cardiac death. At 5 years of follow-up, the hazard ratio of having an abnormal DSE reached a maximum of 1.37 and started to decrease after 7 years of follow-up.
| Univariate | (1): Clinical | (2): (1) + DSE At Rest | (3): (2) + DSE At Peak | |
|---|---|---|---|---|
| HR (CI) | HR (CI) | HR (CI) | ||
| Male gender | 1.45 (1.31-1.62) | 1.39 (1.25-1.55) | 1.39 (1.25-1.55) | 1.38 (1.23-1.54) |
| Age | 1.06 (1.05-1.06) | 1.06 (1.05-1.06) | 1.06 (1.06-1.07) | 1.06 (1.06-1.07) |
| Coronary artery disease | Not significant | – | – | – |
| Heart failure | 1.91 (1.68-2.17) | 1.59 (1.38-1.82) | 1.36 (1.18-1.58) | 1.40 (1.21-1.62) |
| Diabetes mellitus | 1.44 (1.25-1.65) | 1.49 (1.30-1.72) | 1.41 (1.22-1.62) | 1.40 (1.21-1.61) |
| Hypertension | Not significant | – | – | – |
| Hypercholesterolemia | 0.71 (0.62-0.80) | 0.74 (0.65-0.84) | 0.68 (0.60-0.77) | 0.69 (0.60-0.78) |
| Smoking | 1.24 (1.12-1.37 | 1.42 (1.28-1.57) | 1.42 (1.28-1.58) | 1.42 (1.28-1.58) |
| Beta-blockers | 0.81 (0.73-0.89) | 0.86 (0.77-0.96) | Not significant | – |
| Calcium-channel blockers | Not significant | – | – | – |
| Angio-converting enzyme inhibitors | 1.29 (1.16-1.43) | Not significant | – | – |
| Diuretics | 1.73 (1.53-1.97) | 1.33 (1.15-1.53) | 1.23 (1.07-1.42) | 1.23 (1.07-1.42) |
| Digoxin | 2.24 (1.88-2.68) | 1.36 (1.12-1.65) | Not significant | – |
| Nitrates | Not significant | – | – | – |
| Heart rate rest | 1.11 (1.07-1.15) | – | 1.13 (1.09-1.18) | Not significant |
| Systolic blood pressure rest | 1.05 (1.03-1.07) | – | Not significant | – |
| Diastolic blood pressure rest | Not significant | – | – | – |
| Rate pressure product rest | 1.01 (1.00-1.01) | – | Not significant | – |
| Wall motion score index rest | 1.48 (1.38-1.59) | – | 1.32 (1.22-1.44) | Not significant |
| Rest wall motion abnormalities | 1.29 (1.17-1.42) | – | Not significant | – |
| Heart rate peak | 0.97 (0.95-0.99) | – | – | Not significant |
| Systolic blood pressure peak | 0.97 (0.95-0.99) | – | – | Not significant |
| Diastolic blood pressure peak | 0.95 (0.92-0.98) | – | – | Not significant |
| Rate pressure product peak | 1.00 (1.00-1.00) | – | – | Not significant |
| Wall motion score index peak | 1.54 (1.43-1.67) | – | – | 1.35 (1.23-1.48) |
| Peak wall motion abnormalities | 1.37 (1.25-1.51) | – | – | Not significant |
| Any wall motion abnormalities | 1.27 (1.15-1.41) | – | – | Not significant |
| X2-test | 842 | 870 | 870 | |
| p-value | – | P < 0.0001 | P < 0.0001 |
| Univariate | (1): Clinical | (2): (1) + DSE At Rest | (3): (2) + DSE At Peak | |
|---|---|---|---|---|
| HR (CI) | HR (CI) | HR (CI) | HR (CI) | |
| Male gender | 1.56 (1.36-1.78) | 1.46 (1.27-1.67) | 1.40 (1.22-1.61) | 1.38 (1.20-1.59) |
| Age | 1.07 (1.05-1.05) | 1.06 (1.06-1.07) | 1.06 (1.06-1.07) | 1.06 (1.05-1.07) |
| Coronary artery disease | 1.33 (1.18-1.50) | Not significant | – | – |
| Heart failure | 2.47 (2.14-2.86) | 2.00 (1.70-2.35) | 1.60 (1.36-1.89) | 1.65 (1.40-1.94) |
| Diabetes mellitus | 1.40 (1.17-1.67) | 1.42 (1.19-1.70) | 1.32 (1.11-1.58) | 1.30 (1.09-1.56) |
| Hypertension | Not significant | – | – | – |
| Hypercholesterolemia | 0.78 (0.67-0.90) | 0.80 (0.69-0.94) | 0.72 (0.62-0.84) | 0.73 (0.63-0.86) |
| Smoking | 1.36 (1.20-1.54) | 1.54 (1.36-1.74) | 1.54 (1.35-1.74) | 1.53 (1.35-1.73) |
| Beta-blockers | 0.81 (0.71-0.92) | 0.86 (0.75-0.98) | Not significant | – |
| Calcium-channel blockers | Not significant | – | – | – |
| Angio-converting enzyme inhibitors | 1.48 (1.30-1.68) | Not significant | – | – |
| Diuretics | 1.95 (1.67-2.26) | 1.34 (1.12-1.59) | Not significant | – |
| Digoxin | 2.68 (2.18-3.28) | 1.46 (1.17-1.83) | 1.36 (1.09-1.70) | 1.33 (1.06-1.66) |
| Nitrates | 1.32 (1.16-1.49) | Not significant | – | – |
| Heart rate rest | 1.12 (1.06-1.17) | – | 1.13 (1.08-1.18) | 1.14 (1.09-1.19) |
| Systolic blood pressure rest | 1.03 (1.01-1.06) | – | Not significant | – |
| Diastolic blood pressure rest | Not significant | – | – | – |
| Rate pressure product rest | 1.01 (1.00-1.01) | – | Not significant | – |
| Wall motion score index rest | 1.78 (1.64-1.94) | – | 1.54 (1.39-1.69) | Not significant |
| Rest wall motion abnormalities | 1.70 (1.50-1.93) | – | Not significant | – |
| Heart rate peak | 0.96 (0.94-0.99) | – | – | Not significant |
| Systolic blood pressure peak | 0.95 (0.93-0.97) | – | – | Not significant |
| Diastolic blood pressure peak | 0.93 (0.89-0.96) | – | – | Not significant |
| Rate pressure product peak | 1.00 (0.99-1.00) | – | – | Not significant |
| Wall motion score index peak | 1.93 (1.77-2.12) | – | – | 1.63 (1.47-1.81) |
| Peak wall motion abnormalities | 1.76 (1.57-1.99) | – | – | Not significant |
| Any wall motion abnormalities | 1.70 (1.49-1.94) | – | – | Not significant |
| X2-test | – | 684 | 734 | 740 |
| p-value | – | – | P <0.0001 | P <0.0001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


