INDICATIONS
Patients who have acquired long segment esophageal discontinuity and lack stomach as a viable replacement conduit primarily have two options for reconstruction: jejunum and colon. The jejunum is uniquely suitable for esophageal reconstruction because it is relatively abundant, does not require a formal preparation, has similar luminal size compared with esophagus, and does not undergo senescent lengthening like the colon does.
 CONTRAINDICATIONS
CONTRAINDICATIONS
Typical contraindications include Crohn disease, radiation enteritis, portal hypertension, short bowel syndrome, extensive fibrous adhesions, and superior mesenteric artery (SMA) syndrome. Patients who have unfavorable jejunal anatomy may require modifications to the standard approach or an alternative conduit.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
The most important part of the surgery is planning and preparation. When a patient is known to have an extensive disease that will preclude reconstruction with a stomach conduit, the operating room, staff, and patients and their families need to be prepared. The first step in planning the surgery is deciding which route will be taken for the small bowel. There are two main routes for reconstruction with jejunum: Posterior mediastinal and substernal. The posterior mediastinal route is frequently used when patients have immediate reconstruction with any conduit and the substernal route is more often used for delayed reconstruction due to scar tissue precluding the use of the posterior mediastinum. Given below is a list of characteristics of each route (Fig. 27.1A,B).
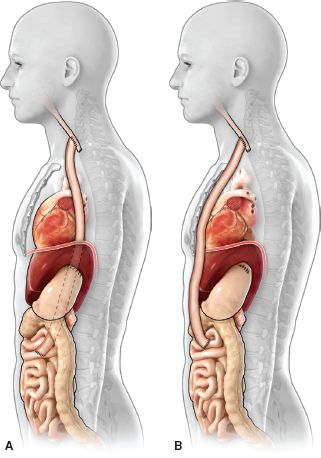
Figure 27.1 A: Posterior mediastinal route for supercharged jejunal conduit. B: Substernal route for supercharged jejunal conduit.
Posterior Mediastinal Route
 Already present if initial reconstruction
Already present if initial reconstruction
 More anatomic
More anatomic
 Potentially shorter route
Potentially shorter route
Substernal Route
 Best option for delayed reconstruction
Best option for delayed reconstruction
 Easier access to chest vessels
Easier access to chest vessels
 Outside field for potential recurrence or radiation
Outside field for potential recurrence or radiation
 May be unavailable if a previous coronary artery bypass graft (CABG) was placed
May be unavailable if a previous coronary artery bypass graft (CABG) was placed
 May empty better
May empty better
Anatomy
The jejunum is a long, hollow organ that extends from the ligament of Treitz and transverse mesocolon (superior and inferior duodenal recesses) to the ileum, which has an indistinct boundary of transition. The mesentery serves as the sole attachment of this organ to the body. The serosa, muscularis propria, and mucosa comprise the three layers of the jejunum wall. The muscularis propria, like the esophagus, has an outer longitudinal layer and an inner circular layer. The lumen is lined by folds that run perpendicular to the longitudinal axis called valvulae conniventes.
The blood supply to the jejunum arises from the SMA. Jejunal branches arise from the left side of this artery and the right side of the SMA provides branches to the ileum and colon. There are one to five jejunal arteries.11
Positioning
Patients are placed in the supine position. The legs are prepared into the field in the event that a saphenous vein graft harvest would be required. The head is turned slightly to the right and a roll is placed beneath the shoulders. The neck is prepared into the field. Slight modifications may need to be made for patients who have a tracheostomy or who require esophageal diversion reversal.
 SURGERY
SURGERY
Dissection of the Jejunum
 Midline abdominal incision
Midline abdominal incision
 Lysis of adhesions if present
Lysis of adhesions if present
 Identification of the ligament of Treitz
Identification of the ligament of Treitz
 Transillumination and mobilization of the bowel mesentery
Transillumination and mobilization of the bowel mesentery
 Identification of the segmental blood supply to the jejunum
Identification of the segmental blood supply to the jejunum
 Take down any feeding jejunostomy site
Take down any feeding jejunostomy site
 Do not divide any of the branches of the small bowel until the neck and tunnel have been prepared to minimize ischemia time
Do not divide any of the branches of the small bowel until the neck and tunnel have been prepared to minimize ischemia time
Preparing the Neck
Dissection of the Neck and Blood Supply/Partial manubriectomy and resection of the first rib (Fig. 27.2)
 Make an incision anterior to the sternocleidomastoid muscle low on the neck extending onto the chest either at or to the left of the midline.
Make an incision anterior to the sternocleidomastoid muscle low on the neck extending onto the chest either at or to the left of the midline.
 Detach the sternocleidomastoid at the head of the clavicle.
Detach the sternocleidomastoid at the head of the clavicle.
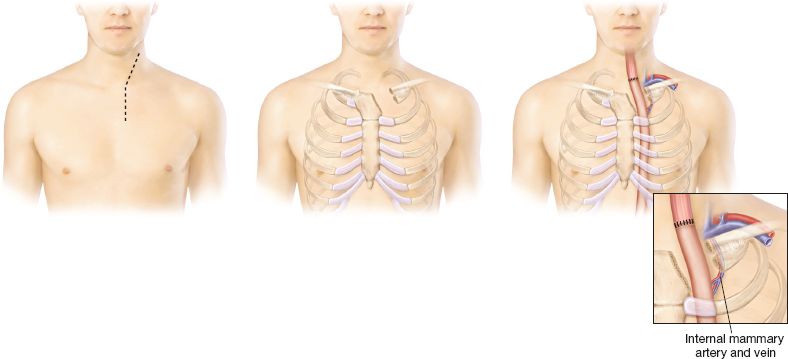
Figure 27.2 Manubriectomy and dissection of donor vessels.
 Dissect around the left first rib ~3 cm lateral of the sternal border.
Dissect around the left first rib ~3 cm lateral of the sternal border.
 Divide the clavicle just lateral to the head and medial to the ligamentous attachments of the clavicle to the first rib. Divide the first rib 3 cm lateral to the sternal border; allow enough space to dissect the left internal mammary artery (LIMA) for microvascular augmentation of the jejunal flap.
Divide the clavicle just lateral to the head and medial to the ligamentous attachments of the clavicle to the first rib. Divide the first rib 3 cm lateral to the sternal border; allow enough space to dissect the left internal mammary artery (LIMA) for microvascular augmentation of the jejunal flap.
 A hemimanubriectomy is performed angled to the left on top of the second rib. The manubrium, the head of clavicle, and the proximal first rib are removed en bloc. Use caution because the internal mammary artery will be located underneath the cartilaginous portion of the ribs, about 1 cm from the sternal border.
A hemimanubriectomy is performed angled to the left on top of the second rib. The manubrium, the head of clavicle, and the proximal first rib are removed en bloc. Use caution because the internal mammary artery will be located underneath the cartilaginous portion of the ribs, about 1 cm from the sternal border.
 A rongeur is used to resect additional bone if needed, smooth the edges so that nothing sharp will injure the bowel or mesentery.
A rongeur is used to resect additional bone if needed, smooth the edges so that nothing sharp will injure the bowel or mesentery.
 Prepare the recipient vessels for microvascular anastomosis. The LIMA is typically an adequate artery, the left internal mammary vein (LIMV) may or may not be robust enough for use. If not, consider using the jugular vein for mesenteric venous anastomosis. A saphenous vein graft can be used to lengthen the artery or vein depending on the position of the conduit and recipient mesenteric vessels.
Prepare the recipient vessels for microvascular anastomosis. The LIMA is typically an adequate artery, the left internal mammary vein (LIMV) may or may not be robust enough for use. If not, consider using the jugular vein for mesenteric venous anastomosis. A saphenous vein graft can be used to lengthen the artery or vein depending on the position of the conduit and recipient mesenteric vessels.
Creating the Tunnel for the Conduit
Creation of the Substernal Tunnel
 From the abdomen, an incision is made on the anterior midline aspect of the diaphragm.
From the abdomen, an incision is made on the anterior midline aspect of the diaphragm.
 Create a midline substernal tunnel while attempting to stay extrapleural. An intrapleural route may be necessary in some cases. Allow enough space for the conduit and mesentery to pass unobstructed (approximately 5 cm diameter should be adequate).
Create a midline substernal tunnel while attempting to stay extrapleural. An intrapleural route may be necessary in some cases. Allow enough space for the conduit and mesentery to pass unobstructed (approximately 5 cm diameter should be adequate).
The posterior mediastinal route is an alternative avenue for positioning of the jejunal conduit depending on the individual patient’s anatomic circumstances and the nature of the esophageal pathology being approached.
Selection and Division of Jejunal Branches
 One must choose the arcade based on transilluminated visualization of the mesenteric vascular segmental anatomy and the length of bowel being considered for transposition.
One must choose the arcade based on transilluminated visualization of the mesenteric vascular segmental anatomy and the length of bowel being considered for transposition.
 There will be anatomic variations and shortened mesenteries from scar tissue, but the ideal jejunal arterial choice is depicted in Figure 27.3A, B.
There will be anatomic variations and shortened mesenteries from scar tissue, but the ideal jejunal arterial choice is depicted in Figure 27.3A, B.
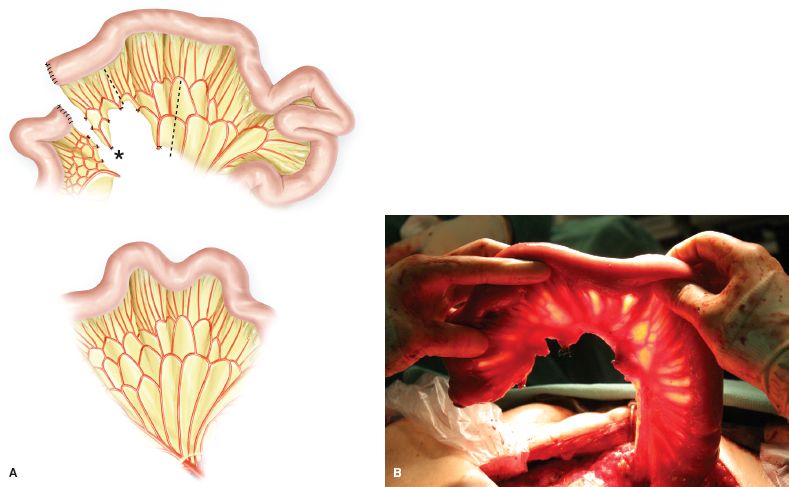
Figure 27.3 A: Selection and division of jejunal branches. Typical branching pattern of proximal jejunum; mesenteric and jejunal cut points are indicated. B: Divided jejunal branches prepared for anastomosis. Vessel loops are placed around recipient vessels for augmentation.
 The first branch of the jejunal blood supply provides blood to the proximal segment beginning after the ligament of Treitz; this first segment with its blood supply is typically left in situ for the Roux limb reconstruction.
The first branch of the jejunal blood supply provides blood to the proximal segment beginning after the ligament of Treitz; this first segment with its blood supply is typically left in situ for the Roux limb reconstruction.
 Perform all of the dissection before dividing any of the blood supply to the small bowel to minimize ischemic time. Once the second arcade has been identified and the remaining segments appear to be appropriate, the mesentery is divided a little proximal to the second arcade to provide additional proximal bowel length for what will become the monitoring flap.
Perform all of the dissection before dividing any of the blood supply to the small bowel to minimize ischemic time. Once the second arcade has been identified and the remaining segments appear to be appropriate, the mesentery is divided a little proximal to the second arcade to provide additional proximal bowel length for what will become the monitoring flap.
 This second arcade will eventually be connected by a microvascular anastomosis to the LIMA and LIMV or jugular vein.
This second arcade will eventually be connected by a microvascular anastomosis to the LIMA and LIMV or jugular vein.
 Open up the mesentery to allow lengthening of the flap (Fig. 27.3B)
Open up the mesentery to allow lengthening of the flap (Fig. 27.3B)
 The mesentery between the third and fourth arcades can be divided only up to the level of the bridging arteries. If the division of the mesentery is continued up to the level of the bowel wall, the third arcade segment of bowel will die.
The mesentery between the third and fourth arcades can be divided only up to the level of the bridging arteries. If the division of the mesentery is continued up to the level of the bowel wall, the third arcade segment of bowel will die.
 The second and third jejunal branches to the SMA are tied off. It is the key to divide the vessels as close to the SMA as possible so that collateral blood flow is maximized.
The second and third jejunal branches to the SMA are tied off. It is the key to divide the vessels as close to the SMA as possible so that collateral blood flow is maximized.
 The fourth arcade is left attached to the superior mesenteric artery (vascular pedicle).
The fourth arcade is left attached to the superior mesenteric artery (vascular pedicle).
 The mesentery between the second and third arcades can be divided up to the level of the bowel to allow the proximal jejunum to unfurl (Fig. 27.3A); this is a critical step to establish a straight jejunal conduit. At this point the most proximal end of the bowel is ischemic.
The mesentery between the second and third arcades can be divided up to the level of the bowel to allow the proximal jejunum to unfurl (Fig. 27.3A); this is a critical step to establish a straight jejunal conduit. At this point the most proximal end of the bowel is ischemic.
 Once the blood supply has been divided, the clock starts for ischemia time (do not divide this segment until the tunnel has been created and the donor vessels have been prepared).
Once the blood supply has been divided, the clock starts for ischemia time (do not divide this segment until the tunnel has been created and the donor vessels have been prepared).

Figure 27.4 A: Antecolic route. B: Retrocolic route.



