We aimed to evaluate how chest pain categorization, currently used to assess the pretest probability of coronary artery disease (CAD), predicts the actual presence of CAD in a population of patients with stable symptoms. We studied 475 consecutive patients enrolled in the Evaluation of Integrated Cardiac Imaging for the Detection and Characterization of Ischemic Heart Disease study based on possible symptoms of CAD. Chest pain or discomfort was categorized as typical angina, atypical angina, or as nonanginal according to the guidelines. Exertional dyspnea and fatigue suspected to be angina equivalents were classified as atypical angina. Patients with a probability of CAD <20 or >90% based on age, gender, and symptoms were excluded. The end points of this substudy were significant CAD (defined by invasive coronary angiography as >50% reduction in lumen diameter in the left main stem or >70% stenosis in a major coronary vessel or 30% to 70% stenosis with fractional flow reserve ≤0.8), inducible myocardial ischemia at noninvasive stress imaging, and their association. Patients’ symptoms had limited ability to predict the presence of significant CAD, global chi-square being 5.0. The inclusion of age increased global chi-square to 18.7 and gender increased it further to 51.1. Using inducible myocardial ischemia or the association of CAD with inducible ischemia as end points, the ability to predict these end points was again better for patient demographics than for patient symptoms. Thus, the ability of current models based on symptoms, age, and gender to predict the presence of CAD is mainly based on patient demographics as opposed to symptoms.
Chest pain accounts for up to 8% of all visits to the emergency departments and up to 10% of acute complaints evaluated in outpatient care. After the first systematic analysis of chest pain characteristics by Rose et al, Diamond and Forrester combined symptoms with patient age and gender to assess the pretest likelihood of coronary artery disease (CAD) at angiography. These results were confirmed by the Coronary Artery Surgery Study. Additional studies were conducted with data from the Duke Databank for Cardiovascular Disease, which also incorporated electrocardiographic findings and information about risk factors. More recently, the predictive model used by Diamond and Forrester was updated by Genders in a contemporary European population of patients with chest pain of uncertain origin. These risk scores are widely accepted in both the European and American guidelines on stable angina to estimate the pretest probability of CAD. The aim of this study was to evaluate how chest pain categorization predicts the actual presence of CAD in a contemporary European population of patients with stable symptoms.
Methods
We studied the patients enrolled in the Evaluation of Integrated Cardiac Imaging for the Detection and Characterization of Ischemic Heart Disease (EVINCI) study. Consecutive patients were enrolled from 14 European centers in 8 countries based on possible symptoms of stable CAD.
Chest pain or discomfort was defined as typical angina if substernal, provoked by exertion or emotional stress, and relieved by rest or nitrates; as atypical angina if satisfying 2 of the criteria; and as nonanginal if satisfying 1 or none. Exertional dyspnea and fatigue suspected to be angina equivalents were classified as atypical angina. Patients with an intermediate probability of CAD (20% to 90%) based on symptoms, age, and gender according to the model by Diamond and Forrester were invited to participate. Patients with acute coronary syndrome, known CAD, left ventricular ejection fraction <35%, more than moderate valve disease, or cardiomyopathy were excluded.
Each of the 475 patients who completed the protocol underwent a study of coronary anatomy by computed x-ray tomographic angiography and at least 1 coronary functional imaging study, including stress single-photon emission computed tomography (293 patients) or positron emission tomography (96 patients) and/or stress echocardiography (261 patients) or cardiac magnetic resonance (85 patients). Computed x-ray tomographic angiographic result was defined as abnormal if ≥1 major coronary artery had a diameter stenosis >50%. Inducible myocardial perfusion abnormality was defined as a summed segmental difference score between stress and rest images ≥2. Inducible wall motion abnormality was defined as an increase in segmental wall motion score ≥1 from rest to stress in ≥2 contiguous segments. If at least 1 noninvasive study result was abnormal, patients underwent invasive coronary angiography (307 patients). Significant CAD was defined by invasive angiography as >50% stenosis in the left main stem or >70% stenosis in a major coronary vessel or 30% to 70% stenosis with fractional flow reserve ≤0.8. The end points of the substudy on patient symptoms were significant CAD at invasive angiography, inducible myocardial ischemia at noninvasive stress imaging, and the association of significant CAD with inducible ischemia. The incremental value of patient symptoms and demographics was assessed using global chi-square from logistic regression models. Likelihood ratio test was used to evaluate the significance of the addition of age and gender to model including only symptoms; p ≤0.05 was considered significant. Calculations were made using STATA, v10 (StataCorp LP, College Station, Texas).
Results
A total of 475 patients with chest pain or equivalent symptoms completed the protocol ( Table 1 ). Patients’ symptoms were categorized as atypical angina in 61% of cases, typical angina in 25%, and as nonanginal chest pain in 14% of patients. The estimated pretest probability of CAD predicted by the Diamond and Forrester model was 59%. The actual prevalence of the study end points was significantly lower: 140 patients (29%, p <0.001). Coronary stenoses involved a single coronary vessel in 21% of patients, 2 vessels in 5%, 3 vessels in 2%, and the left main stem in 1% of patients. A total of 172 patients (36%) had inducible myocardial ischemia, and 100 (21%) had both significant coronary stenoses and inducible ischemia (p <0.001).
| Variable | Whole group (N = 475) | Significant NO (N = 335) | CAD YES (N = 140) | P -value |
|---|---|---|---|---|
| Age (years) | 60.0 ± 8.9 | 59.0 ± 9.1 | 62.3 ± 8.2 | <0.001 |
| Male | 291 (61.3%) | 182 (54.3%) | 109 (77.9%) | <0.001 |
| Non-anginal chest pain | 66 (13.9%) | 39 (11.6%) | 27 (19.3%) | |
| Atypical angina pectoris | 288 (60.6%) | 211 (63.0%) | 77 (55.0%) | 0.074 |
| Typical angina pectoris | 121 (25.5%) | 85 (25.4%) | 36 (25.7%) | |
| Family history of CAD | 160 (33.7%) | 117 (34.9%) | 43 (30.7%) | 0.376 |
| Smoker | 120 (25.3%) | 79 (23.6%) | 41(29.3%) | 0.192 |
| Diabetes mellitus | 115 (24.2%) | 68 (20.3%) | 47 (33.6%) | 0.002 |
| Hypercholesterolemia | 267 (56.2%) | 186 (55.5%) | 81 (57.9%) | 0.640 |
| Hypertension | 290 (61.1%) | 201 (60.0%) | 89 (63.6%) | 0.476 |
| Obesity | 112 (23.6%) | 82 (24.5%) | 30 (21.4%) | 0.475 |
| Diamond and Forrester probability | 58.9[54.4-67.1] | 58.9[46.1-67.1] | 67.1[54.4-79.4] | 0.027 |
| Genders probability | 49[34-59] | 49[28-59] | 56[44-69] | <0.001 |
Patients with significant CAD were older and more frequently men but had chest pain characteristics similar to those of patients without significant CAD ( Table 1 ). Diabetes mellitus was more frequent in patients with significant CAD than in those without. The pretest probability of CAD estimated according to the models by Diamond and Forrester and by Genders was significantly higher in patients with significant CAD than in those without.
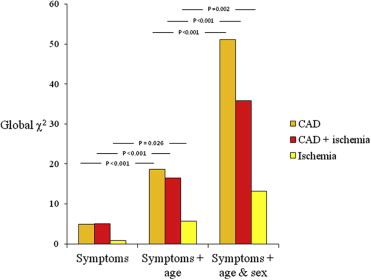
In our patients, symptoms had limited ability to predict the presence of significant CAD, global chi-square being 5.0. The inclusion of age increased global chi-square to 18.7, and gender increased it further to 51.1. Thus, the ability of a model based on symptoms, age, and gender to predict the presence of CAD was mainly based on patient demographics as opposed to symptoms. Using inducible myocardial ischemia or the association of CAD with inducible ischemia as end points, the ability to predict these end points was again better for patient demographics than for patient symptoms ( Figure 1 ).
Results
A total of 475 patients with chest pain or equivalent symptoms completed the protocol ( Table 1 ). Patients’ symptoms were categorized as atypical angina in 61% of cases, typical angina in 25%, and as nonanginal chest pain in 14% of patients. The estimated pretest probability of CAD predicted by the Diamond and Forrester model was 59%. The actual prevalence of the study end points was significantly lower: 140 patients (29%, p <0.001). Coronary stenoses involved a single coronary vessel in 21% of patients, 2 vessels in 5%, 3 vessels in 2%, and the left main stem in 1% of patients. A total of 172 patients (36%) had inducible myocardial ischemia, and 100 (21%) had both significant coronary stenoses and inducible ischemia (p <0.001).



