Left Ventriculography and Aortography
Mateen Akhtar
Frederick A. Heupler Jr.
Left ventriculography provides important anatomic and functional information that supplements coronary angiography. Left ventriculography allows assessment of left ventricular systolic function, degree of mitral regurgitation, and the presence/location of wall motion abnormality or ventricular septal defect (Table 5-1). Ventriculography should not be performed when a patient is hemodynamically unstable. Additional contraindications are listed in Table 5-2.
Preparation
Single-plane ventriculography is performed in most catheterization laboratories. Some operators prefer biplane ventriculography since it can provide more information about ventricular anatomy and function. Biplane ventriculography has limitations such as costly angiographic equipment, additional radiation exposure to both operator and patient, and longer angiographic setup time.
The Medrad powered flow injector is connected to extension tubing and loaded with contrast. During this process, air bubbles should be purged from the injector. Once appropriate pressure measurements have been obtained, the pigtail catheter is connected to extension tubing from the power injector via a blood-contrast interface to minimize the risk of air embolism with left ventriculography. Usually the left ventricular cavity is adequately visualized with 30 to 50 mL of contrast.
Table 5-1 Left Ventriculography: Indications | |||
|---|---|---|---|
|
Table 5-2 Left Ventriculography: Contraindications | |||||||
|---|---|---|---|---|---|---|---|
|
The parameters listed in Table 5-3 can serve as a baseline when deciding on the rate and volume of contrast injection. Certain patient characteristics and clinical settings will influence these settings. For instance, higher volumes of contrast dye (i.e., 50-60 mL) may be necessary to completely opacify the left atrium in patients with severe mitral regurgitation. Higher rates of contrast injection may be necessary in patients with increased cardiac output or dilated left ventricular cavity. Conversely, patients with smaller ventricular cavities such as elderly females or those with hypertensive heart disease may need only 30 to 36 mL of contrast dye for adequate imaging. All patients with hemodynamically significant valvular disease, left ventricular dysfunction, or elevated left ventricular end-diastolic pressure (LVEDP) should receive nonionic contrast for ventriculography.
Entering the Ventricle
The catheter most commonly used for ventriculography is an angled pigtail catheter. The distal segment of this catheter should be angled 145° to 155° in order to facilitate passage into the left ventricle while simultaneously preventing the endhole from contacting the endocardium, thereby reducing the risk of endocardial staining. The multiple side holes help dissipate the pressure of rapid power contrast injection and prevent excessive catheter movement.
Table 5-3 Standard Settings for Left Ventriculography | ||||||||
|---|---|---|---|---|---|---|---|---|
|
The pigtail catheter is advanced over a 0.035-in J-tipped wire to a position in the ascending aorta just superior to the aortic valve. The tip should be pointed toward the orifice of the valve and the catheter rotated so that the pigtail loop resembles a “6.” In this position, gently advancing the catheter will usually push it across the valve orifice and into the ventricle.
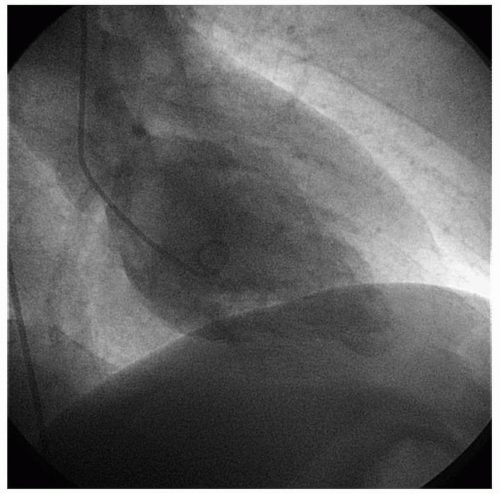
Occasionally, the pigtail catheter will prolapse into the ventricle while the pigtail remains in the ascending aorta. Slowly advancing the guidewire through the terminal portion of the catheter should provide enough additional support to allow entry into the ventricle. Once in the ventricle, the tip of the pigtail should be positioned in the midcavity avoiding contact with the papillary muscles and mitral valve (Figure 5-1).
Troubleshooting
Ventricular Ectopy
If the pigtail catheter irritates the apex, the risk of ventricular ectopy rises significantly. Gentle counterclockwise rotation and pullback should separate the catheter from the septal and apical walls and the ectopy will usually resolve.
Entrapment in Mitral Valve Apparatus
Occasionally, the catheter tip may become trapped within the mitral valve apparatus. If ventriculography is performed under these circumstances, transient but significant mitral regurgitation may develop. Gentle clockwise rotation should dislodge the catheter from the apparatus and place it in the center of the ventricle. If not, the catheter can be withdrawn from the ventricle and ventricular entry reattempted.
Once the catheter is stabilized within the left ventricle, it is connected to the pressure manifold, flushed, and used to record intraventricular pressures. Systolic pressure is typically recorded on a 200-mm Hg scale, while LVEDP is best appreciated on a 40-mm Hg scale. Markedly elevated LVEDP (>30 mm Hg) usually precludes left ventriculography. Administration of sublingual or intravenous nitroglycerin may reduce LVEDP to a more acceptable level.
In patients with compromised left ventricular systolic function, elevated LVEDP, or reduced creatinine clearance, a hand-injection left ventriculogram using digital subtraction angiography (DSA) may be preferred since only 10 mL of contrast is needed. Patients should be instructed to cease respiration and avoid any motion during cine acquisition in order to minimize artifact.
Troubleshooting
Crossing a Stenotic Aortic Valve
Crossing a stenotic aortic valve requires patience, experience, and a bit of luck. This task can be accomplished with a variety of catheters and wires depending on operator preference, experience, and patient anatomy. Some operators prefer a brief cine run of aortic valve opening and closing in right anterior oblique (RAO) and left anterior oblique (LAO) projections in order to identify the angle and plane of the aortic valve orifice prior to crossing it.
Due to the inherent thrombogenicity of guidewires, some operators advise administering 5,000 units of intravenous unfractionated heparin before attempting to cross a stenotic aortic valve. In addition, following every 3 minutes of unsuccessful wire manipulation, the wire should be removed and wiped, and the catheter should be flushed vigorously to prevent thrombus formation. Excessive force should never be used to pass the wire into the left ventricle. Common techniques for crossing a stenotic aortic valve are reviewed below.
Wire Selection
The most common wires utilized to cross a severely stenotic aortic valve are a straight-tipped wire (0.035 or 0.038) or a Rosen exchange J-tipped wire. The Rosen wire is a J-tipped wire with a J-curve that is narrower (5 mm diameter) than the usual J-tip (10 mm diameter). The advantage of the Rosen wire is that the J-tip eliminates the risk of left ventricular perforation, but it may be more difficult to pass across a very severely stenotic valve. The advantage of a straight-tipped wire is that it will cross virtually any stenotic aortic valve, but the straight tip can perforate the left ventricle. The safest procedure is to initially attempt to cross the valve with the Rosen wire, which can be accomplished in more than 90% of cases.
Catheter Selection
Common catheters utilized to cross the aortic valve are the pigtail, Amplatz left coronary, Feldman, Judkins right coronary, and multipurpose catheters. The Amplatz and Feldman catheters are preferred if the aorta is dilated. The length of the secondary curve of these catheters should be adjusted proportionally to the diameter of the aorta. The Judkins right coronary and multipurpose catheters are preferred when the aortic root is narrow.
Technique
Once the selected catheter is positioned in the ascending aorta, the guidewire is cautiously advanced through the endhole of the catheter in an attempt to cross the valve orifice. Carefully advancing and rotating the catheter simultaneously should eventually direct the wire across the aortic valve. The tip of the wire should be directed anteriorly and to the patient’s left. Generally, it is easier to cross the valve in the RAO projection. The angiographer should only attempt to advance the wire across the valve during systole. Altering the amount of wire protruding from the pigtail catheter may help direct the wire. For instance, more wire protruding from the pigtail catheter directs the wire toward the right coronary sinus, whereas less wire protruding directs the wire to the left coronary sinus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree