Left Ventricular Diastolic Function
The diagnosis and management of diastolic heart failure has always been somewhat controversial because it is harder to characterize, and the treatment strategies are less well studied than for systolic heart failure. Clinically, a diagnosis of diastolic heart failure is usually considered when a patient has symptoms and/or signs typical of heart failure (as for systolic heart failure) but their LV systolic function is normal or near-normal (EF >50 per cent).
Diastolic heart failure is also known as ‘heart failure with preserved ejection fraction’ (HFPEF), distinguishing it from systolic heart failure (‘heart failure with reduced ejection fraction’, HFREF). There is however evidence that diastolic dysfunction is also present in patients with systolic dysfunction, so some authorities regard the distinction between systolic and diastolic failure as false and argue that systolic and diastolic dysfunction are part of a single spectrum, and that diastolic dysfunction is often a precursor to systolic dysfunction. It certainly seems that there is significant overlap between systolic and diastolic dysfunction and they should not be regarded as mutually exclusive entities.
HEART FAILURE WITH PRESERVED EF
Many authorities argue that LV diastolic dysfunction can be present regardless of whether systolic function is normal or not. However, if you wish to specifically diagnose heart failure with preserved EF, you need to confirm that systolic function is indeed virtually normal. The European Society of Cardiology criteria for ‘normal or mildly abnormal LV function’ are:
CAUSES OF IMPAIRED LV DIASTOLIC FUNCTION
Diastolic dysfunction is thought to reflect ‘stiffness’ or impaired relaxation of the LV, and so occurs in conditions where the LV becomes less compliant:
ageing
hypertension
myocardial ischaemia
aortic stenosis
infiltrative cardiomyopathies.
ECHO ASSESSMENT OF LV DIASTOLIC FUNCTION
Any assessment of LV diastolic function also includes a full assessment of LV dimensions, mass and systolic function as outlined in Chapter 15. Remember to look for features indicative of the underlying aetiology of diastolic dysfunction (e.g. aortic stenosis, ischaemic heart disease).
Assess left atrial (LA) size, as outlined in Chapter 18. In diastolic dysfunction, LA dilatation reflects the cumulative effect of elevated LV filling pressures over a prolonged period of time. However, remember that LA dilatation can also be seen in other conditions including mitral stenosis/regurgitation and atrial fibrillation or flutter.
Many methods are available to characterize LV diastolic function on echo, but the most widely used are:
LV inflow
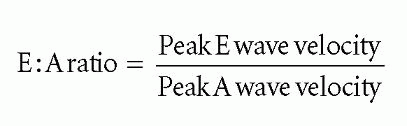
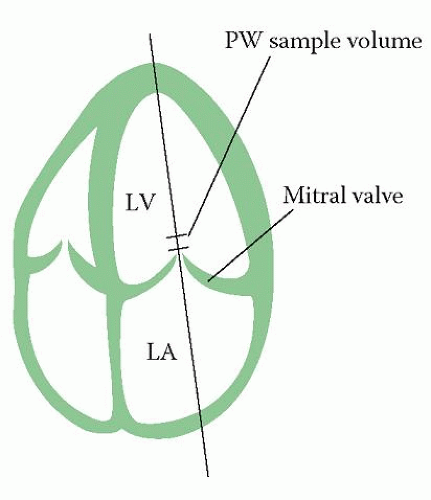
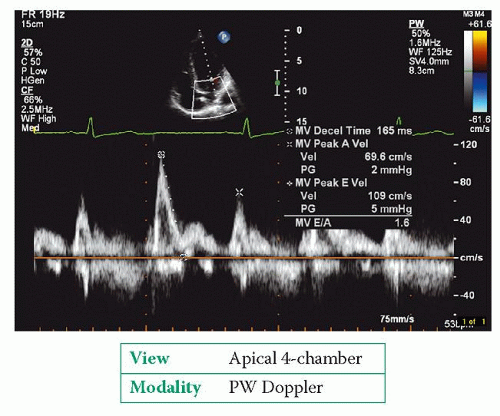
To assess LV inflow, perform PW Doppler in the apical 4-chamber view with a 1-3 mm sample volume placed at the tips of the mitral valve leaflets (Fig. 17.1). Obtain a PW Doppler trace (Fig. 17.2) and measure:
peak E wave velocity
peak A wave velocity
E wave deceleration time (DT)
isovolumic relaxation time (IVRT).
A sweep speed of 25 or 50 mm/s is used initially to look for respiratory variation in peak E and A wave velocities. The sweep speed is then increased to 100 mm/s before taking at least three sets of measurements with the patient’s breath held at end-expiration.