INDICATIONS/CONTRAINDICATIONS
The open left lower lobectomy (LLL) is traditionally considered as one of the easiest anatomic pulmonary resections to perform. In fact, a common term for the open LLL is the “intern lobectomy” referring to the relative ease of the procedure allowing a surgical intern to perform the surgery as an introduction to general thoracic techniques. However, ironically with the proliferation of minimally invasive thoracic surgery such as video- or robotic-assisted thoracic surgery (VATS and RATS), a need for an open lobectomy suggests complex patient or tumor anatomy that would make VATS or RATS prohibitive. These situations include need for a bronchoplasty or arterioplasty such as a left lower lobe sleeve resection, with reimplantation of the left upper lobe bronchus (described elsewhere in this textbook) or even tumor growth into the left atrium requiring cardiopulmonary bypass for a R0 resection.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
All patients planned for pulmonary resection should undergo pulmonary function testing (PFT). Forced expiratory volume in 1 second (FEV1) and diffusing capacity of the lung for carbon monoxide (DLCO) are often considered the most important pulmonary function measurements for assessing postoperative risk; and the DLCO has been demonstrated to be a predictor of postoperative morbidity and mortality. FEV1 and DLCO are reported as absolute values, as well as “percent predicted” (predicted value based on age, gender, and height). The FEV1 and DLCO percent predicted is a better representative of pulmonary function than the absolute values of the tests.
A FEV1 >1.5 L is suitable for lobectomy, and a FEV1 of 2 L, or >80% predicted and a DLCO >80% predicted are suitable for pneumonectomy. Regardless of the preoperative predicted values, the predicted postoperative (PPO) FEV1 or DLCO should be calculated. PPO FEV1 and DLCO are calculated by estimating the quantity of lung parenchyma lost after surgical removal. For lobectomy, counting the number of anatomic segments removed is used for calculation (Fig. 17.1). For pneumonectomy the fraction of lung perfusion measured by quantitative radionuclide ventilation/perfusion (V/Q) scan is used to determine PPO FEV1 and PPO DLCO (Fig. 17.1). PPO FEV1 or DLCO <30% indicates an increased risk for perioperative and cardiopulmonary morbidity after pulmonary resection, and these patients should undergo additional exercise testing to confirm inoperability. This includes cardiopulmonary exercise testing to determine maximal oxygen consumption (VO2max).
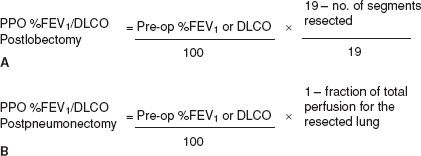
Figure 17.1 A: Calculating the predicted postoperative (PPO) FEV1 or DLCO. For lobectomy, counting the number of anatomic segments removed is used for calculation. B: For pneumonectomy the fraction of lung perfusion measured by quantitative radionuclide ventilation/perfusion scan is used.
For operative planning, a chest computed tomography (CT) scan is performed with intravenous (IV) contrast to define anatomy and tumor characteristics. The chest CT should extend through a horizontal plan of the upper portion of the kidneys, encompassing the bilateral adrenal glands and the majority of the liver, which are common targets of lung cancer metastasis. A positron emission tomography (PET)/CT scan should be performed for primary lung cancers larger than 1 cm in size to identify metastasis, and in larger tumors and/or tumors with high metabolic activity on PET, or patients with neurologic symptoms, a brain magnetic resonance imaging (MRI) should be performed to evaluate for brain metastasis. There should be a low threshold to perform endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) and/or video cervical mediastinoscopy to stage the lymph nodes of the mediastinum.
 SURGERY
SURGERY
This chapter describes the essential principles of a conventional open LLL. General anesthesia is obtained with single-lung isolation. This is performed with either a double-lumen endotracheal tube (right-sided or left) or a balloon bronchial blocker. The patient is placed in the right lateral decubitus position, left side up, and the table is flexed to allow widening of the intercostal spaces and distraction of the ipsilateral hip out of the way of the surgeons.
An open LLL can be performed through any number of incisions, including a posterolateral incision, muscle-sparing axillary incision, or an anterior thoracotomy. We prefer a posterolateral incision (described elsewhere) carried through the fifth intercostal space, which provides a bird’s-eye view of the fissure between the left upper and lower lobes.
The usual indication for an LLL is for primary lung cancer. For primary lung cancer, a mediastinal lymph node sampling or dissection must be performed for accurate staging. This involves systematic assessment of stations 7, 8L, 9L, 5, and 6 as well as nonmediastinal stations 10 and 11. This can be done at the beginning of the operation, during the course of the procedure, or at the end. Additional station 10 and 11 lymph nodes, and more segmental stations 12 and 13 are included in the specimen.
The open LLL involves three main steps: (1) Division of the inferior pulmonary vein (IPV), (2) division of the interlobar basal pulmonary artery, and (3) division of the lower lobe bronchus. There is no oncologic advantage to dividing the vein or artery first.
Division of the Inferior Pulmonary Vein
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


