In adults, the left atrial (LA) volume has been shown to reflect diastolic function and is a powerful predictor of cardiac morbidity and mortality. Normative LA volume values in children and the effect of loading conditions on the LA volume in those with congenital heart disease are lacking. The purposes of the present study were to (1) establish normal LA volume values for children, (2) assess the effect of left ventricular volume loading conditions on LA volume, and (3) describe the effect of abnormal myocardial relaxation on the LA volume. We retrospectively reviewed the echocardiograms from 3 pediatric cohorts: group N (n = 522), children with normal echocardiographic findings; group VSD/PDA (n = 71), children with ventricular septal defect (VSD; n = 50) or patent ductus arteriosus (PDA; n = 21); and group HC (n = 63), children with hypertrophic cardiomyopathy (HC). In group N, we identified the LA volume indexed to the body surface area (LA volume index) as a consistent measure of the LA volume in children 3 to 23 months old (mean 16 ± 3 ml/m 2 ) and 2 to 17 years old (mean 22 ± 4 ml/m 2 ). LA dilation was more common in group VSD/PDA than in group N (27% vs 2%, p <0.0001) and in children with moderate or large shunts than in those with smaller shunts (61% vs 5%, p <0.0001). In group HC, the LA volume index correlated with the mitral valve E/e′ ratio (p <0.0001). In conclusion, this is the first study to establish normal pediatric LA volume values. The LA volume index is a reproducible measure of LA size in children ≥3 months old. The LA volume index reflects a chronically increased left ventricular volume load in children with VSD or PDA and chronically elevated left ventricular filling pressures in children with HC.
Given the lack of data regarding the left atrial (LA) volume in children, an investigation of the LA volume in the pediatric population is a timely, clinically important endeavor. The objectives of our study were to (1) generate normative data for the LA volume in children, (2) identify whether changes in the LA volume correlate with changes in the chronic left-to-right shunt volume in children with ventricular septal defect (VSD) or patent ductus arteriosus (PDA), and (3) identify whether the LA volume correlates with diastolic dysfunction in children with hypertrophic cardiomyopathy (HC).
Methods
All children (age range 0 to 17 years) who had undergone outpatient transthoracic echocardiography at our institution with documentation of the LA volume from January 2004 to December 2006 were identified (n = 4,353). We reviewed each study and clinical history for potential confounding medical conditions. To avoid the confounding effects of acute illness on the cardiac hemodynamics, subjects were excluded from the study if they had been hospital in-patients when echocardiography had been performed. Other exclusion criteria included a history of prematurity, cardiac disease (except for isolated PDA or VSD), a chronic medical disorder, and evidence of an inherited syndrome.
From this group, a cohort of children with normal echocardiographic findings (group N) was selected. A second cohort (group VSD/PDA) was also identified, consisting of otherwise healthy children with isolated PDA or VSD, excluding any children with an atrial level shunt. A third cohort with left ventricular (LV) diastolic dysfunction consisted of children with HC who had undergone echocardiographic evaluation from January 2005 to October 2009 (group HC). All group HC subjects had Doppler evidence of diastolic dysfunction.
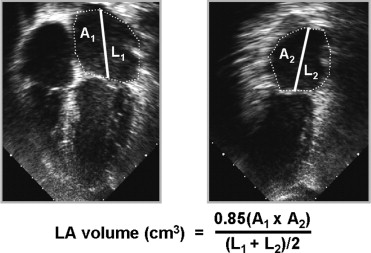
For all groups, the demographic and echocardiographic data were abstracted from the medical records, and all echocardiographic images were reviewed. The echocardiograms consisted of traditional 2-dimensional, spectral Doppler, and color-flow Doppler imaging to assess the chamber size, cardiac anatomy, and the presence and size of shunt lesions. Pulsed-wave Doppler in the mitral valve inflow and in the pulmonary veins and the tissue Doppler velocity of the lateral and medial mitral annulus at the cardiac base were measured to assess the LV diastolic function. These measurements were performed using previously reported standards. The LA volume was calculated using a modified biplane area-length method ( Figure 1 ), which has been previously validated. The intra- and interobserver variability in LA volume measurement was assessed by randomly selecting 25 healthy patients from group N and 25 “abnormal” patients from group HC. The LA volume of each of these patients was measured twice (separated by at least a 1-day interval) by a single observer (intraobserver) and by 2 separate observers (interobserver). In addition, all LA volume measurements in our study were reviewed and remeasured from the digitally archived studies by a single observer.
We compared the LA volume with the demographic data, including age, height, weight, and body surface area. The strength of the correlation with these variables was assessed. The LA volume was analyzed both as the absolute volume and indexed to the body surface area. The LA volume index was calculated by dividing the LA volume by the body surface area, using the same method validated for adults. The body surface area was calculated using the Haycock formula: [0.024265 × (height in centimeters) 0.3964 × (weight in kilograms) 0.5378] . The LA volume and LA volume index data from group N were used to establish age-related normative values. Furthermore, the LA volume index was compared to the established echocardiographic measurements of diastolic function, including the pulmonary venous inflow Doppler, mitral inflow Doppler, and tissue Doppler velocity measurements.
In group VSD/PDA, the relative size of the VSD or PDA was graded as small, moderate, or large. The PDA size was semiquantitatively determined by the absolute PDA size (compared to the branch pulmonary artery size) and the quantity of left to right shunting. The VSD size was determined semiquantitatively using the anatomic size of the VSD, the degree of shunt flow across the defect, Doppler velocity across the VSD, and the degree of chronic left heart dilation (including LA and LV size). The LA volume index for group VSD/PDA was compared to the expected normal values from group N to identify whether LA enlargement was related to the degree of left-to-right shunting. A subject was identified as having LA enlargement if the LA volume index exceeded the 95% confidence interval for age using our group N normative data.
In group HC, the echocardiographic evaluation included an assessment of LV systolic function, LV wall thickness, the presence and severity of LV outflow tract obstruction, and the degree of mitral regurgitation. LV outflow tract obstruction was defined as a maximum instantaneous gradient of ≥20 mm Hg at rest or with provocation. The traditional parameters of diastolic function were also obtained, including mitral valve inflow Doppler, pulmonary venous inflow Doppler, and tissue Doppler velocities. The LA volume index was compared to these structural and functional measurements.
The LA volume and LA volume index were compared to the demographic and echocardiographic data using univariate logistic regression analysis. Variables found to have a significant univariate association with LA volume were analyzed using a multivariate logistic regression model to adjust for potential confounders. Normal values for the LA volume index are expressed as the mean ± SD. Comparisons of sets of paired variables were performed using the chi-square test. Probability values of <0.05 were considered statistically significant. All statistical analyses were conducted using JMP, version 7.0.1 (SAS Institute, Cary, North Carolina). The Mayo Clinic institutional review board approved the present study.
Results
We identified 522 echocardiograms with normal findings (group N). The demographic data for group N are listed in Table 1 . On univariate analysis, the LA volume significantly correlated with multiple age-related variables, including height, weight, and body surface area. The LA volume was not influenced by gender. Multivariate analysis revealed that LA volume was most closely related to the body surface area, with a correlation strength of R 2 = 0.81 ( Table 2 ).
| Variable | Normal (n = 522) | VSD (n = 50) | PDA (n = 21) | HC (n = 63) |
|---|---|---|---|---|
| Demographics | ||||
| Females | 47.5% | 52.0% | 57.1% | 30.1% |
| Age (years) | 10.0 ± 5.9 | 4.3 ± 4.7 | 5.0 ± 5.0 | 12.9 ± 4.2 |
| Weight (kg) | 41.4 ± 25.7 | 19.8 ± 19.5 | 19.6 ± 16.0 | 59.5 ± 29.7 |
| Body surface area (m 2 ) | 1.3 ± 0.5 | 0.7 ± 0.5 | 0.7 ± 0.4 | 1.6 ± 0.5 |
| Shunt size (%) | ||||
| Small | — | 37 (74.0%) | 10 (47.6%) | — |
| Moderate | — | 9 (18.0%) | 5 (23.8%) | — |
| Large | — | 4 (8.0%) | 6 (28.6%) | — |
| Other echocardiographic findings | ||||
| Moderate/severe mitral regurgitation | — | — | — | 31.7% |
| Left ventricular outflow tract obstruction | — | — | — | 68.2% |
| Systolic anterior motion of mitral valve | — | — | — | 79.3% |
| Septal thickness (mm) | — | — | — | 23.8 ± 9.4 |
| Demographic | Univariate p Value | R2 | Multivariate p Value |
|---|---|---|---|
| Gender | NS | — | — |
| Age | <0.0001 | 0.71 | 0.99 |
| Height | <0.0001 | 0.74 | NA ⁎ |
| Weight | <0.0001 | 0.79 | 0.78 |
| Body surface area | <0.0001 | 0.81 | <0.0001 |
⁎ Not included in multivariate analysis because of potential confounding effect.
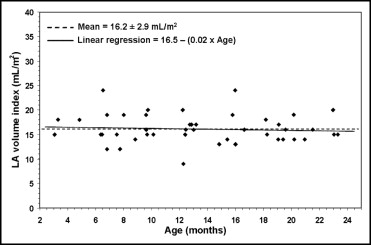
We next examined whether the LA volume indexed to the body surface area (LA volume index) was dependent on age. The youngest children had the smallest LA volume index values. However, we found that the LA volume index was consistent if the cohort was considered in 2 separate categories: children aged 3 to 23 months ( Figure 2 ) and those aged 2 to 17 years ( Figure 3 ). The mean LA volume index differed slightly between these 2 age groups.
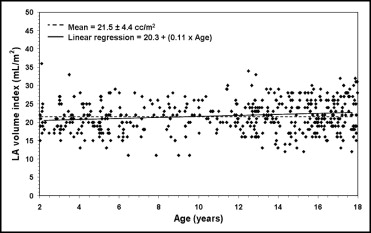
On univariate analysis of children aged 2 to 17 years, the LA volume index exhibited an incremental, but statistically significant, relation with several measures of LV diastolic function, including the mitral inflow E wave velocity, A wave velocity, E/A ratio, mitral annular tissue Doppler e′ velocity, and pulmonary vein velocities. On multivariate analysis, the mitral E/A ratio (p = 0.007) and pulmonary vein systolic velocity (p = 0.02) correlated independently with an increasing LA volume index.
Table 1 lists the data for the 71 patients with either an isolated VSD (n = 50) or PDA (n = 21; group VSD/PDA), of whom, collectively, 54% were females and whose mean age was 4.5 ± 4.8 years. The median LA volume index increased with increasing shunt size: 20 ml/m 2 (range 8 to 42) among those with a small shunt, 26 ml/m 2 (range 15 to 68) among those with a moderate shunt, and 32 ml/m 2 (range 17 to 124) among those with a large shunt. LA enlargement was present in 27% of group VSD/PDA, significantly more than among group N (p <0.0001). Children with moderate or large intracardiac shunts were more likely to manifest LA enlargement than children whose left-to-right shunts were assessed as small (61% vs 5%, p <0.0001; Figure 4 ).




