20 Leadless Pacing Concepts
All pacing leads are associated with complications, including infection, fracture, failure, and dislodgement1,2 (see Chapter 19 for problems associated with transvenous pacing leads). Also, extraction of a chronically implanted lead is a high-risk procedure. Access to the left ventricle is achieved with a pacing lead advanced into the coronary sinus and positioned in a coronary vein branch. Implantation of the left ventricular lead may be technically challenging and associated with a significant incidence of failure to access and implant the lead, implantation in a suboptimal location, and complications.3,4 With new device systems that require implantation of multiple leads, and with patients living longer, the incidence of lead complications increases over time. Therefore, efforts are ongoing to develop a pacing system that eliminates the pacing lead as a conduit for energy transfer.
 Pacing in Cardiac Resynchronization Therapy
Pacing in Cardiac Resynchronization Therapy
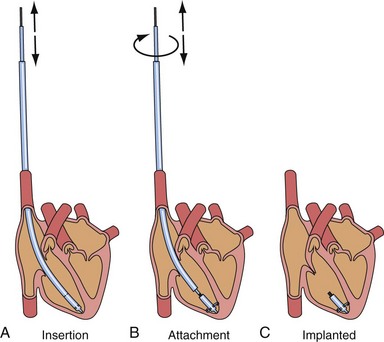
Compared with epicardial pacing, endocardial left ventricular (LV) stimulation minimizes the conduction delay from the epicardium to the endocardium and may result in more physiologic conduction, with greater hemodynamic benefit. An animal experiment of eight anesthetized dogs with induced left bundle branch block (LBBB) studied the acute hemodynamic effects of endocardial and epicardial LV pacing. Electrical activation and repolarization were evaluated with 122 epicardial and endocardial electrodes. Compared with epicardial pacing, endocardial pacing doubled the degree of electrical resynchronization and increased the LV dP/dtmax by 90% and stroke work by 50% (Fig. 20-1). During single-site LV pacing, the range of atrioventricular (AV) intervals with more than 10% increase in LV resynchronization and LV dP/dtmax was significantly longer for endocardial than epicardial pacing. Epicardial pacing, but not endocardial pacing, was associated with a transmural dispersion of repolarization.5
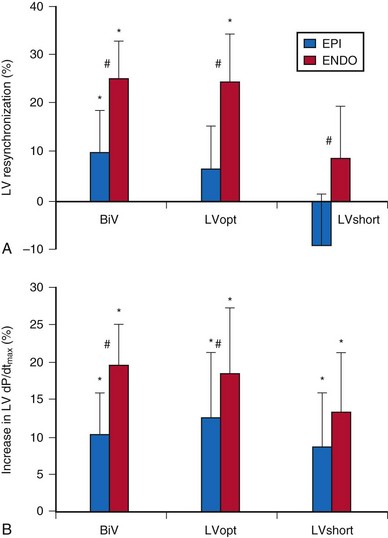
Figure 20-1 Acute hemodynamics of epicardial and endocardial CRT.
(Data from Van Deuren C, van Geldorp IE, Rademakers LM, et al. Endocardial left ventricular pacing improves cardiac resynchronization therapy in canine LBBB hearts. Circ Arrhythm Electrophysiol 2:580-587, 2009.)
Randomized clinical trials on cardiac resynchronization therapy (CRT) have demonstrated its clinical benefits. The acute hemodynamic response to CRT in patients with nonischemic dilated cardiomyopathy depends on the pacing site, with major interindividual and intraindividual variations. In 35 patients with heart failure of nonischemic etiology referred for CRT implantation, the acute hemodynamic response to DDD-LV pacing was systematically assessed at 11 predetermined LV pacing sites. Pacing at the endocardial LV site with the best hemodynamic response doubled the increase in dP/dtmax compared to epicardial coronary sinus pacing6 (Fig. 20-2). CRT with endocardial LV pacing maximizes hemodynamic benefit and may be associated with fewer nonresponders.
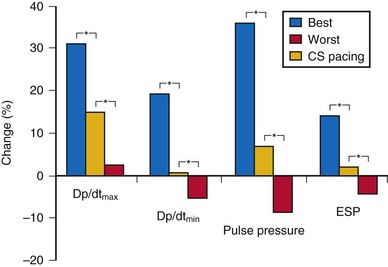
Figure 20-2 Acute hemodynamic changes of DDD-LV pacing.
(Data from Derval N, Steendijk P, Gula LJ, et al. Optimizing hemodynamics in heart failure patients by systematic screening of left ventricular pacing sites: the lateral left ventricular wall and the coronary sinus are rarely the best sites. J Am Coll Cardiol 55:566-575, 2010.)
In a retrospective study comparing chronic epicardial and endocardial pacing, 23 patients with severe heart failure and wide QRS were implanted with CRT devices. Fifteen patients underwent conventional epicardial LV pacing, and eight underwent endocardial LV pacing by atrial transeptal approach because of unfavorable coronary sinus anatomy. Six months after implant, echocardiography and Doppler tissue imaging were performed during right ventricular (RV) and biventricular (BiV) pacing to evaluate LV function, LV wall velocities, and regional electromechanical delay. The septal wall (21.3% vs. 11%) and lateral wall (54% vs. 41%) electromechanical delay was reduced more by endocardial than epicardial CRT compared with RV pacing.7 Endocardial LV pacing improves LV function better than epicardial pacing when measured by standard echocardiographic parameters such as aortic and mitral time-velocity integral (40% vs. 2%) and lateral LV wall systolic motion (31% vs. 14%).7 Endocardial CRT appears to provide more homogeneous intraventricular resynchronization than epicardial CRT and is associated with better LV filling and systolic performance.
Cardiac resynchronization therapy with multisite LV stimulation has been associated with better LV remodeling and a higher left ventricular ejection fraction (LVEF) than conventional BiV stimulation.8 Forty patients with permanent atrial fibrillation undergoing implantation of CRT device were enrolled in a multicenter randomized single-blind crossover study. Each patient had one lead implanted in the right ventricle and two LV leads implanted in two separate coronary veins. Echocardiographic parameter of resynchronization, reverse remodeling, quality of life, and 6-minute walking distance with triple-site (one RV and two LV) versus dual-site (one RV and one LV) stimulation were compared. Triple-site stimulation was associated with a higher LVEF and smaller LV end-systolic volume and diameter.
 Totally Self-Contained Intracardiac Pacemaker
Totally Self-Contained Intracardiac Pacemaker
After the first clinical use of implantable pacing system in 1960, a totally self-contained leadless intracardiac pacemaker had been developed as a new concept of pacing technology. The intracardiac pacemaker was as small as a capsule 8 mm in diameter and 18 mm long, with integral electrodes and an attachment mechanism.9 It was small enough to be implanted entirely within the heart when delivered with a catheter guided by a transvenous sheath (Fig. 20-3). The attachment mechanism consisted of radially directed spiral barbs, with the stimulation electrodes located away from the attachment site. In an animal study of three dogs implanted with the prototype of this “capsule” intracardiac pacemaker, after several weeks of implant, the stimulation threshold was stable and less than 1 microjoule per pulse. The first functioning investigational model of the intracardiac pacemaker used a mercury battery as the power source for asynchronous electronic pacing. The system was implanted in a dog with induced heart block and provided asynchronous pacing for 66 days with no complications, because the capsule was in the right ventricle.
Chemical batteries, biologic fuel, kinetic energy, and nuclear-powered energy have been evaluated for incorporation into the capsule intracardiac pacemaker as power sources. Betacel, a family of beta-voltaic nuclear batteries (Douglas Laboratories, McDonnell-Douglas Astronautics, St. Louis) had been developed and incorporated into the first nuclear-powered intracardiac pacemaker.9 The investigational system had been implanted in a dog for asynchronous pacing at 100 beats per minute (bpm) to demonstrate the feasibility of this pacing technology. It was once thought that such technology might enable the battery life of a pacemaker to be extended to several decades. However, results of safety and feasibility on further testing were not reported.
Kinetic Energy
Many concepts have been patented for the development of a leadless pacing system. More than a decade ago, the automatic energy-generating system for quartz watches had been used as a leadless pacemaker power source in an experimental animal model.10 A mechano-electrical energy conversion system developed for quartz watches that converted kinetic energy into electrical energy was used as the power source of a commercially available pulse generator circuit and directly sutured on the epicardial surface of the canine heart. After a full charge, adequate energy was generated for continuous overdrive pacing of the heart for 60 minutes. The stroke motion of the myocardium generated pulses of energy that were stored in a capacitor. The charging and discharging results suggested that the automatic power-generating system might supply enough energy for use in a cardiac pacemaker. It was thought that this might be developed into a button-type cardiac pacemaker to be implanted by a thoracoscopic procedure.
Acoustic (Ultrasound) Energy
The next development in alternative energy sources for pacing to replace the pacing lead was the use of ultrasound (ultrasonic, acoustic) energy. The use of ultrasound-mediated energy to drive a remotely positioned electrode for direct myocardial stimulation was first reported in 2006.11 This new technology uses the mechano-electrical properties of piezoelectric materials for transformation of energy. The experimental setup used in the acute study included an ultrasound-transmitting transducer connected to an ultrasound generator and a steerable bipolar electrophysiology (EP) catheter incorporating a receiver-electrode near the distal end (Fig. 20-4). Ultrasound energy was amplitude adjusted and transmitted at about 330 kHz. The low frequency used in this application enables better tissue penetration. Ultrasound pulses generated from the transmitting transducer travel through the chest wall to reach the receiver-electrode, with circuitry to transform the pulses into electrical energy for myocardial stimulation.
The feasibility and safety of this novel technology was first demonstrated acutely in animals.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree