SNC alterations
Congenital and acquired disorders of the control of the respiratory center
Myelomeningocele and Arnold-Chiari malformations
Alterations in the ventilation pump
Congenital hypotonias
Myasthenia gravis
Phrenic and diaphragmatic paralysis
Myopathy
Muscular dystrophy
Guillain-Barré syndrome
Botulism
Diaphragmatic hernia
Spinal muscular atrophy
Skeletal alterations
Kyphoscoliosis
Thoracic walls deformities
Alterations in the airway and respiratory parenchyma
Obstruction of the high airway: craniofacial malformative syndromes (Pierre Robin, Treacher Collins)
Laryngotracheomalasia
Tracheoesophageal fistula
Subglottic stenosis
Vocal chords paralysis
Bronchopulmonary alterations
Bronchopulmonary dysplasia
Cystic fibrosis
Lung hypoplasia
Obliterans bronchiolitis
Others
Congenital and acquired cardiopathies
Metabolic diseases
Respiratory: Involving the lung parenchyma or airway.
Central nervous system: The beginning of the ventilation is affected, especially during deep sleep.
Respiratory pump: When nerve tracts, motoneurons, neuromuscular plate, musculature, or thoracic cavity are affected.
Mixed: Involving more than one of the aforementioned causes.
Susceptible to improvement: Such as bronchopulmonary dysplasia, airway malacia, Guillain-Barré syndrome, obliterans bronchiolitis.
Stable or progressive: Includes neuromuscular disease, hypoventilation syndrome.
Chronic Mechanical Ventilation Indications
The main indication of mechanical ventilation is to maintain gaseous exchange. Therefore, it is indicated in patients with chronic respiratory insufficiency, which include alterations of chest wall (severe scoliosis), alterations in breath control (central hypoventilation syndromes), serious alterations of the airway (malacia in trachea or bronchus), and alterations of lung parenchyma, such as obliterans bronchiolitis and bronchopulmonary dysplasia.
PaCO2 > 45 mmHg PaO2 < 65 mmHg
Limited air intake
Use of accessory musculature
Decrease of physical activity
Scarce weight gain
Objectives of Chronic Mechanical Ventilation
Patients requirements are different, as well as goals or objectives to achieve with each one.
Revert hypoxemia
Revert respiratory acidosis
Alleviate respiratory work
Decrease systemic or myocardial oxygen consumption
Stabilize chest wall
Decrease the lung iatrogenic lesion and other ventilation complications
Extend and improve life quality
Provide an environment which increases each individual’s potential
Reduce morbidity
Favor an appropriate child physical growth and psychosocial development
Selection of Ventilation Method
Duration: Quantity of hours per day of needing support. If more than 12 hours per day are required, the invasive way through tracheostomy is preferred. If the need is equal or less than 12 hours, non-invasive way, using the most appropriate interface for the patient.
Tolerance to interfaces: This is an essential factor in the success or failure of non-invasive ventilation. Anatomical, psychological, and mental health factors may provoke intolerance to facial, nasal, or naso-buccal mask, and therefore the patient must be ventilated through tracheostomy.
Risk/benefit balance and ethical decisions: The decision of using chronic ventilation and the method applied, force us to consider universal ethical principles. For instance, the case of limitation of therapeutic efforts.
Scenario: Currently, chronic ventilation can occur in different scenarios, such as in a critical patient unit or in the pediatric room of a critical patients hospital, in a chronic patients hospital, or at home, depending on the degree of complexity of the patient and access to domiciliary programs.
Need for autonomy: Patients with night exclusive ventilation have a greater autonomy for doing daily life activities such as attending school. In patients with total ventilation, this autonomy can be given through appropriate equipment selection.
Ventilation Modes
CPAP : It delivers continuous positive pressure in the airway during the whole respiratory cycle. It requires the patient to breathe spontaneously and be able to start an effective inhalation. It prevents the collapse of the upper and lower tract of the airway, as well as in the alveoli, improving oxygenation. It is used in patients with severe malacia and when removing the mechanical ventilation.
Spontaneous (S): Two leveled pressure (IPAP/EPAP): It gives inspiratory and expiratory pressure, without the need for backup rate. It is used as a previous step at the employment of CPAP.
Spontaneous/cyclic (S/T): Two leveled pressure with respiratory frequency (RF).
Dual: Two leveled inspiratory pressure (IPAP max/IPAP min). With assured tidal volume with or without respiratory frequency. Both are utilized for the treatment of patients with neuromuscular diseases or diseases of the lung parenchyma.
Intermittent synchronization (SIMV/PC): It gives two leveled pressure (MIP/PEEP), backup respiratory rate, and programmable support pressure. In patients without ventilatory autonomy; for example, type I spinal atrophy, severe bronchopulmonary dysplasia, or obliterans bronchiolitis.
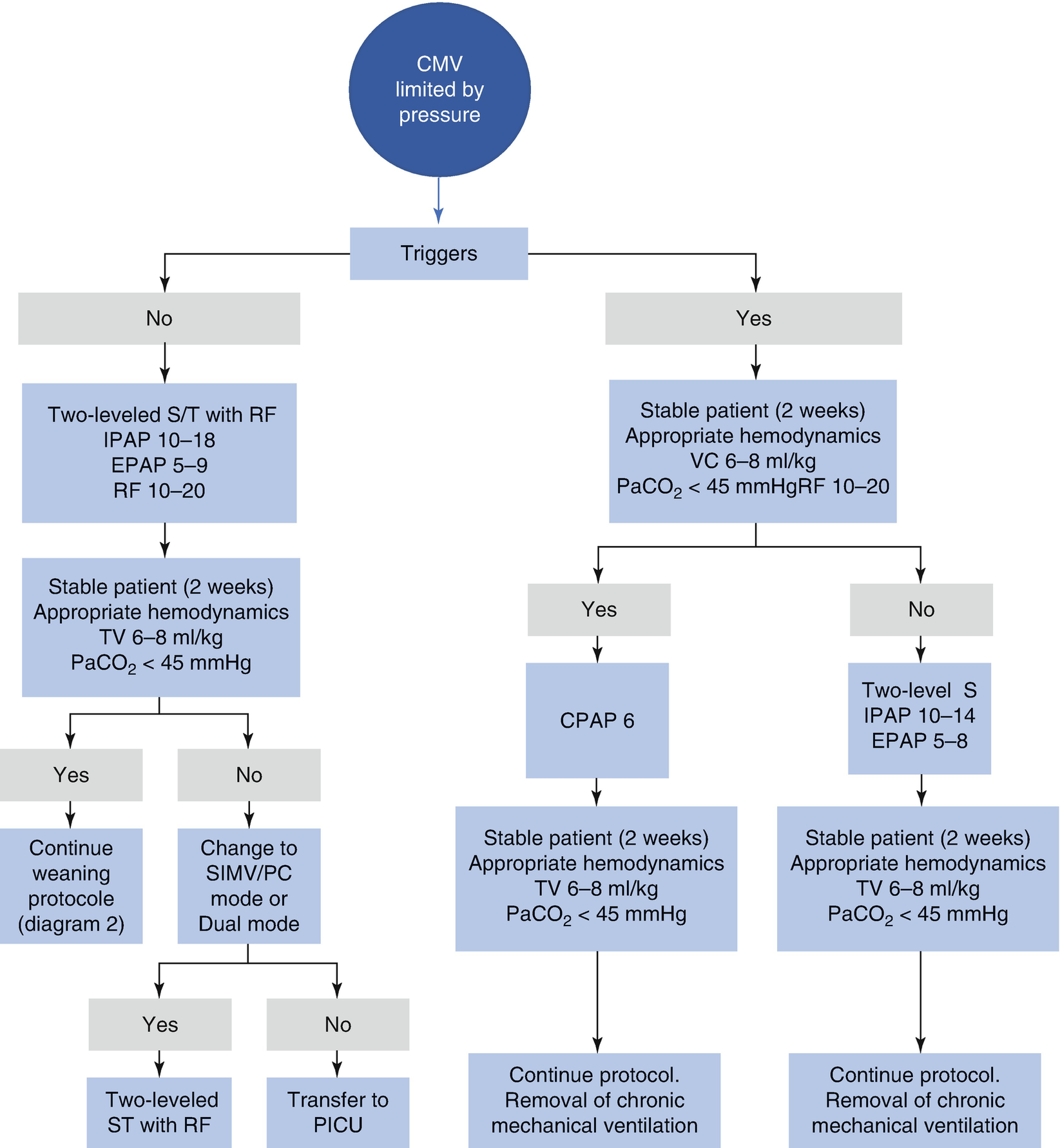
Selection of method of ventilation
Equipment
Registration: Through cards, which are interpreted through a software, we can obtain information about hours of equipment use, percentage of respirations triggered by the patient, pressures and volume given by the ventilator in each respiration and for those generated by the patient, if present.
Autonomy: It refers to the possibility of functioning without electric supply, in other words, whether the equipment possesses a battery or not. In this case, the internal battery duration is important, because it will enable us to use the equipment for transferences, or for going with the patient to school or other daily life activities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


